Back
Poster Session C
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1518–1542) Systemic Sclerosis and Related Disorders – Clinical Poster II
1540: Correlations of Soluble Interleukin-2 Receptor Serum Levels with Markers of Inflammation and Pathological High-sensitivity Troponin T and Its Possible Role as a Predictor of Early Clinical Progress in Systemic Sclerosis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LS
Luise Schumacher, -None-
University of Lübeck, Germany
Stralsund, Germany
Abstract Poster Presenter(s)
Luise Schumacher1, Sebastian Klapa2, Antje Mueller3 and Gabriela Riemekasten4, 1University of Lübeck, Lübeck, Germany, 2Universityhospital Schleswig-Holstein; University of Lübeck; Clinic of Rheumatology and Clinical Immunology, Luebeck, Germany, 3University Hospital Schleswig-Holstein (UKSH), Lübeck, 4University Clinic Schleswit-Holstein (UKSH), Luebeck, Germany
Background/Purpose: Systemic sclerosis (SSc) is characterized by chronic inflammation leading to damage of the vascular endothelium and excessive collagen deposition in several target organs. The interaction of interleukin 2 (IL-2) with the corresponding receptor (IL-2R) is involved in the regulation of autoimmune processes. The shedding product of the IL-2R alpha chain, soluble IL-2 receptor (sIL-2R, CD25), can either reduce or enhance immune responses. Previously, elevated serum levels of sIL-2R were found in the bronchoalveolar lavage of SSc patients with and without interstitial lung disease (SSc-ILD) as well as serologically in patients with early SSc, and thus suggested to be a biomarker for clinical development in SSc. Furthermore, the presence of idiopathic inflammatory myositis (IMM) seems to play a role since SSc-IMM overlap patients have shown higher markers of inflammation and more frequent organ manifestations.
Methods: To determine if serological levels of sIL-2R could serve as predictor of clinical complications in SSc, sera were analysed [limited cutaneous SSc (lcSSc) n=160; diffuse cutaneous SSc (dcSSc), n=137] using a sandwich ELISA. Clinical data (pulmonary fibrosis, PAH, mRSS, cardiac involvement, therapy) and serological markers (hs-CRP, NT-proBNP, neutrophil counts, creatine kinase, hs-troponin T, beta2-microglobulin) were assessed at the time of serum sampling and up to 48 months after baseline. Clinical progress was defined by the need to change therapies.
Results: Patients with dcSSc presented elevated levels of sIL-2R compared to all SSc (dcSSc: 765±593 U/ml vs. 646±473 U/ml, p=0.0001; Fig.1). In SSc general, sIL-2R levels correlated with beta2-microglobulin (r=0.6161, p< 0.0001, ROC-AUC:0.8428), hs-CRP (r=0.4091, p< 0.0001, ROC-AUC:0.7110), NT-proBNP (r=0.2610, p< 0.0001, ROC-AUC:0.6793), neutrophiles (r=0.2749, p< 0.0001) and hs-troponin T (r=0.4548, p< 0.0001, ROC-AUC:0.8729). Further, sIL-2R levels discriminated normal from pathological levels of hs-troponin T (sensitivity 80.0%, specificity 80.1%), these results being even more significant in patients without myositis (ROC-AUC: 0.9111; sensitivity 81.82.0%, specificity 87.85%). Using Log-rank test and Mantel-Cox proportional hazard models, we found that sIL-2R levels above 900 U/ml predicted early clinical progress in SSc within 12 months which had led to therapy escalation (HR:6.20, p< 0.0001; Fig. 2).
Conclusion: In SSc, serum levels of sIL-2R could be of diagnostic value by identifying clinical progress. Its role in pathophysiology, especially regarding disease manifestations such as cardiac involvement needs to be further investigated.
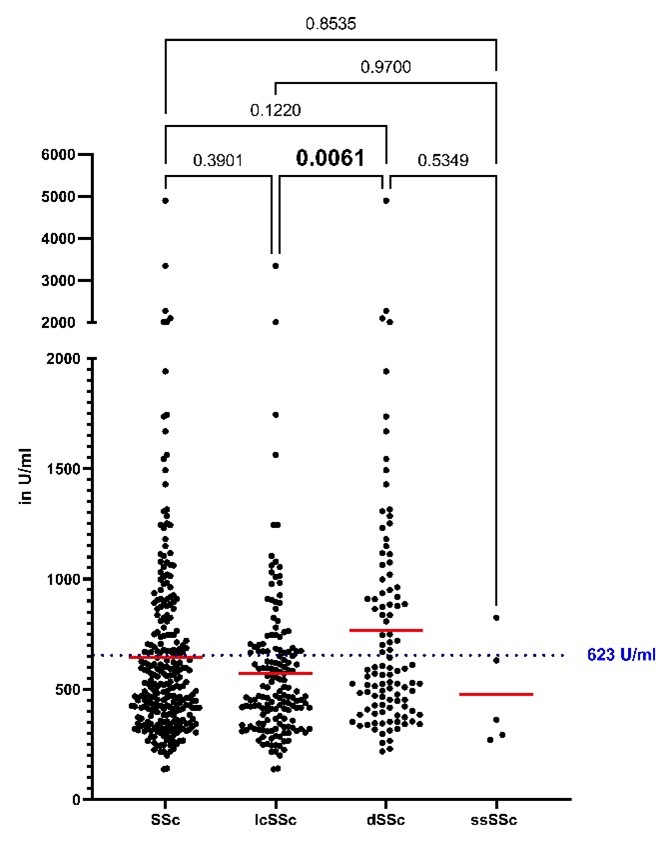 Fig. 1: sIL-2R levels in SSc. Patients with dcSSc presented elevated levels of sIL-2R compared to lcSSc (dcSSc: 765±593 U/ml vs. 572±361 U/ml, p=0.0061).
Fig. 1: sIL-2R levels in SSc. Patients with dcSSc presented elevated levels of sIL-2R compared to lcSSc (dcSSc: 765±593 U/ml vs. 572±361 U/ml, p=0.0061).
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1290399-2-ANY.jpg width=440 height=426.484641638225 border=0 style=border-style: none;>
Disclosures: L. Schumacher, None; S. Klapa, None; A. Mueller, None; G. Riemekasten, Boehringer Ingelheim.
Background/Purpose: Systemic sclerosis (SSc) is characterized by chronic inflammation leading to damage of the vascular endothelium and excessive collagen deposition in several target organs. The interaction of interleukin 2 (IL-2) with the corresponding receptor (IL-2R) is involved in the regulation of autoimmune processes. The shedding product of the IL-2R alpha chain, soluble IL-2 receptor (sIL-2R, CD25), can either reduce or enhance immune responses. Previously, elevated serum levels of sIL-2R were found in the bronchoalveolar lavage of SSc patients with and without interstitial lung disease (SSc-ILD) as well as serologically in patients with early SSc, and thus suggested to be a biomarker for clinical development in SSc. Furthermore, the presence of idiopathic inflammatory myositis (IMM) seems to play a role since SSc-IMM overlap patients have shown higher markers of inflammation and more frequent organ manifestations.
Methods: To determine if serological levels of sIL-2R could serve as predictor of clinical complications in SSc, sera were analysed [limited cutaneous SSc (lcSSc) n=160; diffuse cutaneous SSc (dcSSc), n=137] using a sandwich ELISA. Clinical data (pulmonary fibrosis, PAH, mRSS, cardiac involvement, therapy) and serological markers (hs-CRP, NT-proBNP, neutrophil counts, creatine kinase, hs-troponin T, beta2-microglobulin) were assessed at the time of serum sampling and up to 48 months after baseline. Clinical progress was defined by the need to change therapies.
Results: Patients with dcSSc presented elevated levels of sIL-2R compared to all SSc (dcSSc: 765±593 U/ml vs. 646±473 U/ml, p=0.0001; Fig.1). In SSc general, sIL-2R levels correlated with beta2-microglobulin (r=0.6161, p< 0.0001, ROC-AUC:0.8428), hs-CRP (r=0.4091, p< 0.0001, ROC-AUC:0.7110), NT-proBNP (r=0.2610, p< 0.0001, ROC-AUC:0.6793), neutrophiles (r=0.2749, p< 0.0001) and hs-troponin T (r=0.4548, p< 0.0001, ROC-AUC:0.8729). Further, sIL-2R levels discriminated normal from pathological levels of hs-troponin T (sensitivity 80.0%, specificity 80.1%), these results being even more significant in patients without myositis (ROC-AUC: 0.9111; sensitivity 81.82.0%, specificity 87.85%). Using Log-rank test and Mantel-Cox proportional hazard models, we found that sIL-2R levels above 900 U/ml predicted early clinical progress in SSc within 12 months which had led to therapy escalation (HR:6.20, p< 0.0001; Fig. 2).
Conclusion: In SSc, serum levels of sIL-2R could be of diagnostic value by identifying clinical progress. Its role in pathophysiology, especially regarding disease manifestations such as cardiac involvement needs to be further investigated.
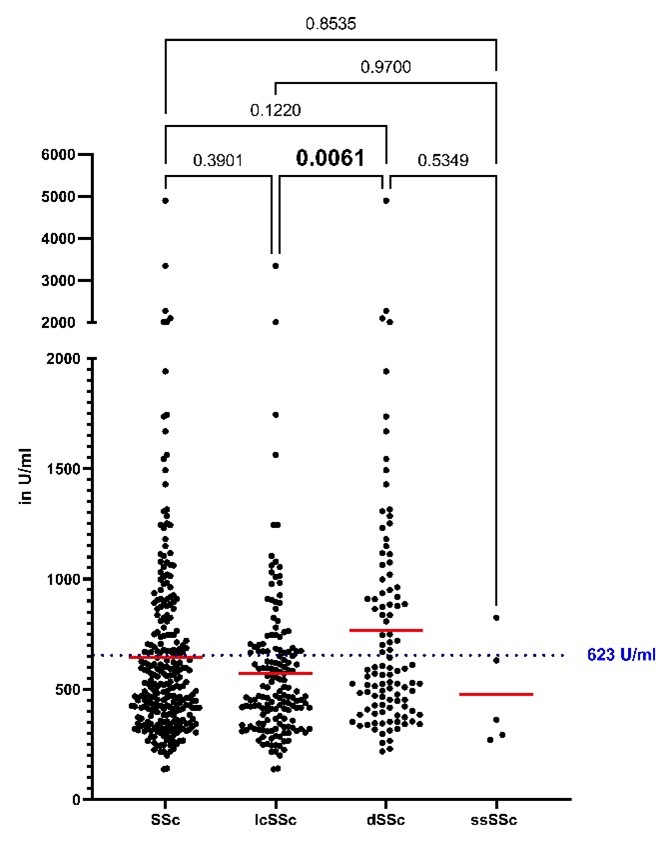 Fig. 1: sIL-2R levels in SSc. Patients with dcSSc presented elevated levels of sIL-2R compared to lcSSc (dcSSc: 765±593 U/ml vs. 572±361 U/ml, p=0.0061).
Fig. 1: sIL-2R levels in SSc. Patients with dcSSc presented elevated levels of sIL-2R compared to lcSSc (dcSSc: 765±593 U/ml vs. 572±361 U/ml, p=0.0061). <img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1290399-2-ANY.jpg width=440 height=426.484641638225 border=0 style=border-style: none;>
Fig. 2: sIL-2R values >900 U/ml predicted early clinical progress in SSc (HR:6.20, p < 0.0001) within 12 months which required therapy escalation.
Disclosures: L. Schumacher, None; S. Klapa, None; A. Mueller, None; G. Riemekasten, Boehringer Ingelheim.

