Back
Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1486–1517) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
1486: Derivation and Internal Validation of a Disease-specific Cardiovascular Risk Prediction Model for Patients with Psoriatic Arthritis and Psoriasis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- KC
Keith Colaco, MSc
University of Toronto
Toronto, ON, Canada
Abstract Poster Presenter(s)
Keith Colaco1, Ker-Ai Lee2, Vinod Chandran3, Paula Harvey4, Richard Cook2, Vincent Piguet4, Dafna Gladman5 and Lihi Eder6, 1University of Toronto, Toronto, ON, Canada, 2University of Waterloo, Waterloo, ON, Canada, 3Departments of Medicine and Laboratory Medicine and Pathobiology, University of Toronto/ Schroeder Arthritis Institute, Krembil Research Institute, University Health Network, Toronto, ON, Canada, 4Women's College Hospital, Toronto, ON, Canada, 5Toronto Western Hospital, Schroeder Arthritis Institute, Toronto, ON, Canada, 6Women’s College Research Institute, Department of Medicine, University of Toronto, Toronto, ON, Canada
Background/Purpose: Cardiovascular risk in patients with psoriatic disease (PsD) may be underestimated by conventional scoring systems. We derived and internally validated a 5-year disease-specific cardiovascular risk prediction model for patients with PsD.
Methods: Participants from a longitudinal PsD cohort without a prior history of cardiovascular events who were followed from 1992 to 2020 were analyzed. Data on cardiovascular risk factors, and PsD-related features that included measures of musculoskeletal and skin inflammation, patient-reported outcomes and medications were obtained from the cohort's database. The study outcome included a composite cardiovascular event including any of the following: angina, myocardial infarction, congestive heart failure, transient ischemic attack, stroke, revascularization procedures and cardiovascular death. Using time-varying covariates, we fit models to predict cardiovascular events within a 5-year time period. A base prediction model including traditional cardiovascular risk factors was first assessed, followed by an expanded model that included the base model and PsD-related features. Model performance was assessed using measures of discrimination and calibration, and sensitivity and specificity.
Results: A total of 1,336 patients (92% with psoriatic arthritis) were analyzed (mean age 48 ± 12.9 years, 46.8% female) (Table 1). During a mean follow-up of 6.8 years, 85 (6.4%) patients developed incident cardiovascular events. Discriminative ability of the base model (with traditional cardiovascular risk factors alone) was excellent, with an AUC of 85.5 (95% CI 81.9-89.1) (Figure 1). An expanded model that included traditional cardiovascular risk factors and the number of damaged joints did not improve risk discrimination compared to the base model (AUC 85.5, 95% CI 82.0-89.1). All models were well calibrated and appeared to be an accurate estimate of the observed number of cardiovascular events (Figure 2). Sensitivity and specificity of the 10% cut-off point for cardiovascular risk was 49% and 92%, respectively. When considering the total number of cardiovascular events, depending on the model, up to 53% of events occurred in patients who were classified as 'intermediate risk' (< 10%).
Conclusion: A prediction model that includes traditional cardiovascular risk factors alone is accurate in predicting cardiovascular risk in patients with PsD, showing excellent discrimination and calibration in this patient population.
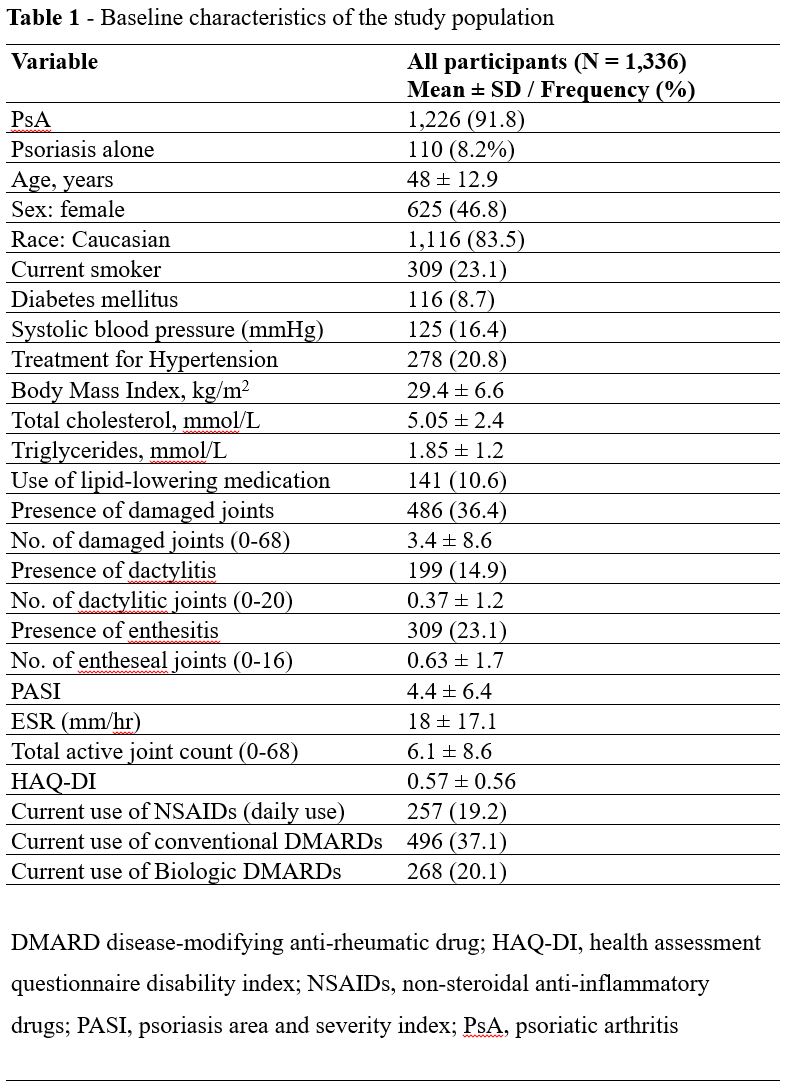 Table 1 - Baseline characteristics of the study population.
Table 1 - Baseline characteristics of the study population.
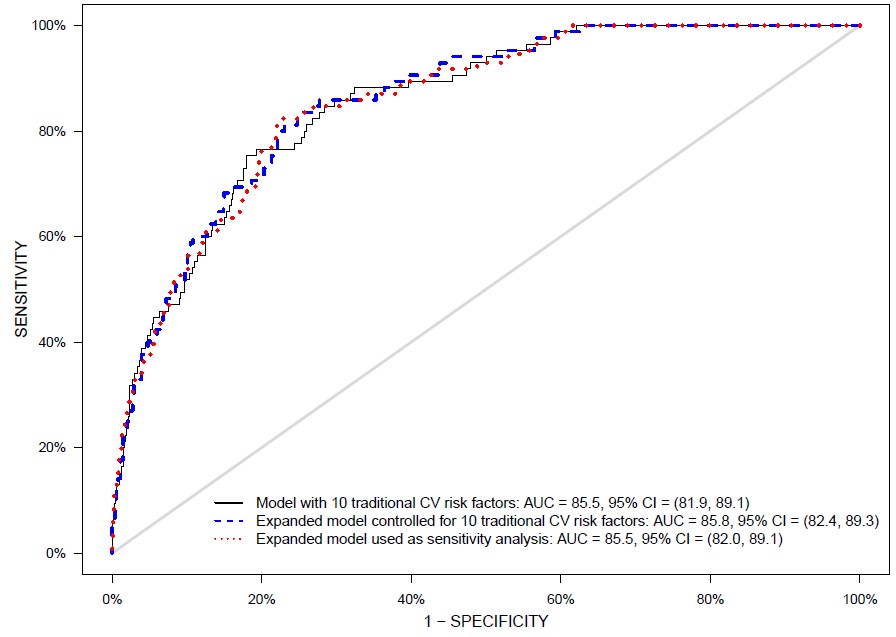 Figure 1. Receiver operating characteristic (ROC)-curve for the different risk prediction models. Comparison of base model (traditional CV risk factors) and expanded model (traditional CV risk factors plus other disease-related factors) for prediction of cardiovascular events.
Figure 1. Receiver operating characteristic (ROC)-curve for the different risk prediction models. Comparison of base model (traditional CV risk factors) and expanded model (traditional CV risk factors plus other disease-related factors) for prediction of cardiovascular events.
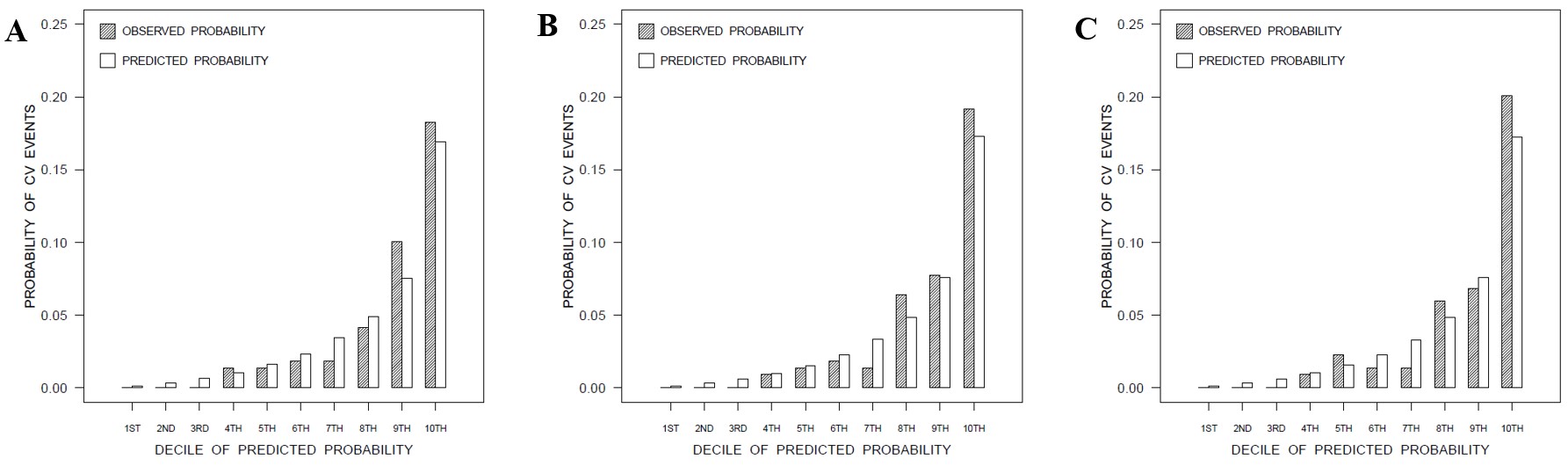 Figure 2 - Observed (grey) versus predicted (white) probability of CV events in deciles of predicted risk, for the base (A), expanded (B), and sensitivity analysis (C) risk prediction models.
Figure 2 - Observed (grey) versus predicted (white) probability of CV events in deciles of predicted risk, for the base (A), expanded (B), and sensitivity analysis (C) risk prediction models.
Disclosures: K. Colaco, None; K. Lee, None; V. Chandran, AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Novartis, Amgen, Pfizer Inc, UCB; P. Harvey, None; R. Cook, None; V. Piguet, None; D. Gladman, AbbVie, Amgen, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, Bristol-Myers Squibb(BMS), Galapagos, UCB Pharma, Celgene; L. Eder, AbbVie, Lilly, Novartis, UCB, Pfizer.
Background/Purpose: Cardiovascular risk in patients with psoriatic disease (PsD) may be underestimated by conventional scoring systems. We derived and internally validated a 5-year disease-specific cardiovascular risk prediction model for patients with PsD.
Methods: Participants from a longitudinal PsD cohort without a prior history of cardiovascular events who were followed from 1992 to 2020 were analyzed. Data on cardiovascular risk factors, and PsD-related features that included measures of musculoskeletal and skin inflammation, patient-reported outcomes and medications were obtained from the cohort's database. The study outcome included a composite cardiovascular event including any of the following: angina, myocardial infarction, congestive heart failure, transient ischemic attack, stroke, revascularization procedures and cardiovascular death. Using time-varying covariates, we fit models to predict cardiovascular events within a 5-year time period. A base prediction model including traditional cardiovascular risk factors was first assessed, followed by an expanded model that included the base model and PsD-related features. Model performance was assessed using measures of discrimination and calibration, and sensitivity and specificity.
Results: A total of 1,336 patients (92% with psoriatic arthritis) were analyzed (mean age 48 ± 12.9 years, 46.8% female) (Table 1). During a mean follow-up of 6.8 years, 85 (6.4%) patients developed incident cardiovascular events. Discriminative ability of the base model (with traditional cardiovascular risk factors alone) was excellent, with an AUC of 85.5 (95% CI 81.9-89.1) (Figure 1). An expanded model that included traditional cardiovascular risk factors and the number of damaged joints did not improve risk discrimination compared to the base model (AUC 85.5, 95% CI 82.0-89.1). All models were well calibrated and appeared to be an accurate estimate of the observed number of cardiovascular events (Figure 2). Sensitivity and specificity of the 10% cut-off point for cardiovascular risk was 49% and 92%, respectively. When considering the total number of cardiovascular events, depending on the model, up to 53% of events occurred in patients who were classified as 'intermediate risk' (< 10%).
Conclusion: A prediction model that includes traditional cardiovascular risk factors alone is accurate in predicting cardiovascular risk in patients with PsD, showing excellent discrimination and calibration in this patient population.
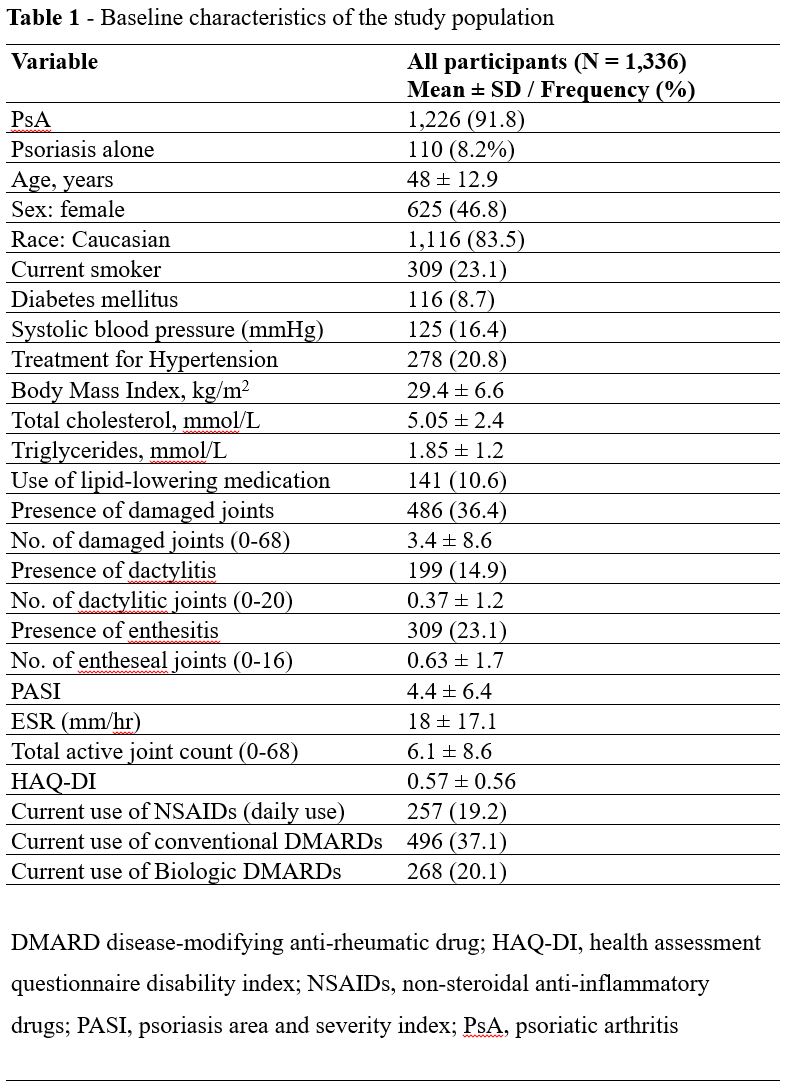 Table 1 - Baseline characteristics of the study population.
Table 1 - Baseline characteristics of the study population.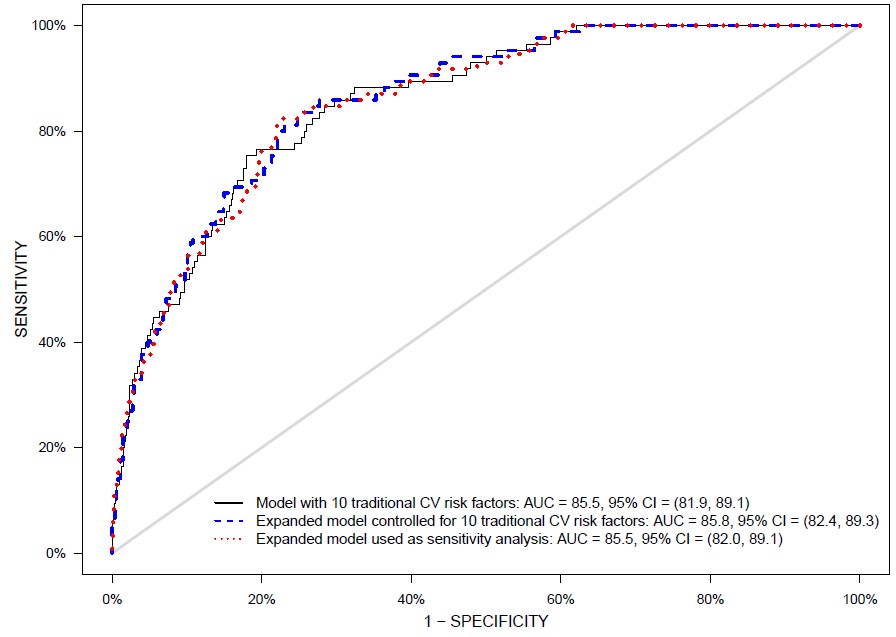 Figure 1. Receiver operating characteristic (ROC)-curve for the different risk prediction models. Comparison of base model (traditional CV risk factors) and expanded model (traditional CV risk factors plus other disease-related factors) for prediction of cardiovascular events.
Figure 1. Receiver operating characteristic (ROC)-curve for the different risk prediction models. Comparison of base model (traditional CV risk factors) and expanded model (traditional CV risk factors plus other disease-related factors) for prediction of cardiovascular events. 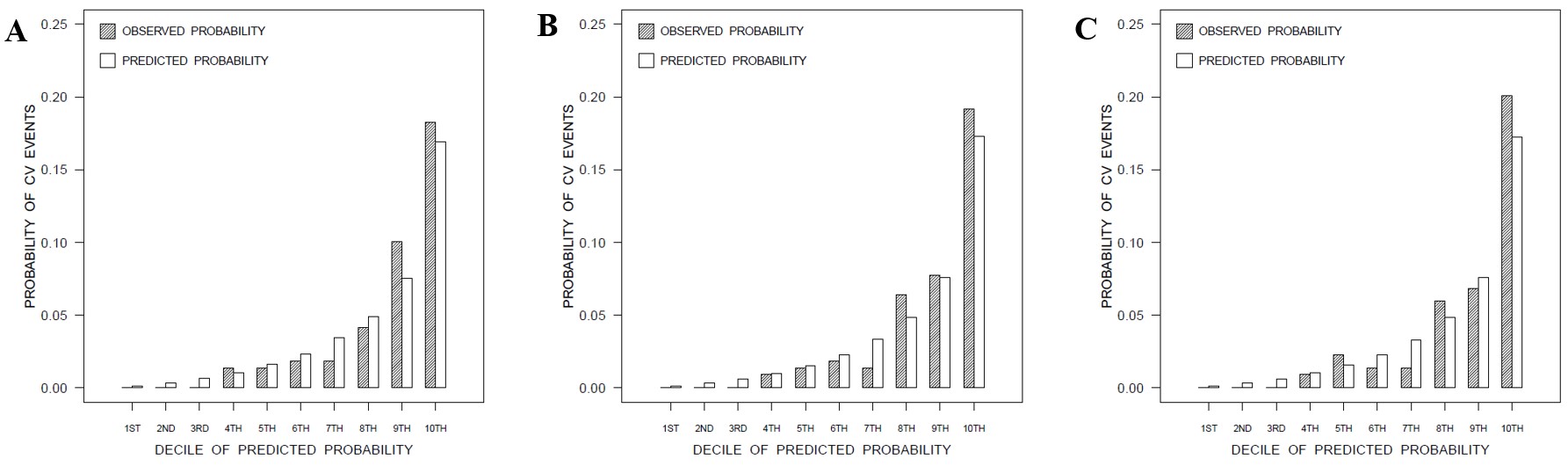 Figure 2 - Observed (grey) versus predicted (white) probability of CV events in deciles of predicted risk, for the base (A), expanded (B), and sensitivity analysis (C) risk prediction models.
Figure 2 - Observed (grey) versus predicted (white) probability of CV events in deciles of predicted risk, for the base (A), expanded (B), and sensitivity analysis (C) risk prediction models. Disclosures: K. Colaco, None; K. Lee, None; V. Chandran, AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Novartis, Amgen, Pfizer Inc, UCB; P. Harvey, None; R. Cook, None; V. Piguet, None; D. Gladman, AbbVie, Amgen, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, Bristol-Myers Squibb(BMS), Galapagos, UCB Pharma, Celgene; L. Eder, AbbVie, Lilly, Novartis, UCB, Pfizer.

