Back
Abstract Session
Vasculitis
Session: Abstracts: Vasculitis – Non-ANCA-Associated and Related Disorders I (1615–1620)
1615: Myocardial Infarction in Patients with Systemic Vasculitis and Population Controls: Characteristics and Overall Mortality
Sunday, November 13, 2022
4:30 PM – 4:40 PM Eastern Time
Location: Ballroom AB
- PS
Pavlos Stamatis, MD, PhD, MSc
Lund University
Larissa, Greece
Presenting Author(s)
Pavlos Stamatis1, Moman Mohammad2, David Erlinge2, Carl Turesson3, David Jayne4 and Aladdin Mohammad5, 1Department of Clinical Sciences Lund, Rheumatology, Lund University, Sweden, Larissa, Larisa, Greece, 2Department of Clinical Sciences Lund, Cardiology, Lund University, Lund, Sweden, 3Rheumatology, Department of Clinical Sciences, Malmö, Lund University, Malmö, Sweden, 4University of Cambridge, Cambridge, United Kingdom, 5Rheumatology, Department of Clinical Sciences, Lund University, Lund, Sweden
Background/Purpose: The deleterious effect of inflammation combined with glucocorticoid treatment may increase the risk for atherosclerotic events. The aims of this study were to investigate differences in baseline characteristics and survival after incident MI in patients with systemic vasculitis [SV: ANCA-associated vasculitis (AAV) and Giant Cell Arteritis (GCA)] compared to a matched reference "non-vasculitis" population with MI.
Methods: The study cohort consisted of 1527 patients with SV (GCA n=1202; AAV n=325) diagnosed between 1997-2016 in Skåne, southern Sweden. Using a unique personal identification number, the SV cohort was linked to the national SWEDEHEART register which covers every coronary care unit admission in Sweden. All cases with SV diagnosed with acute MI after the onset of SV were identified and, matched with 10 controls (age, sex and year of MI diagnosis. Baseline characteristics were compared between SV-patients and controls. The risk for death at 1, and 3 years after the MI was assessed using a Cox regression model.
Results: A total of 86 patients (6%) were diagnosed with incident MI corresponding to proportions of 7% and 5% among AAV and GCA patients respectively. Table 1 presents the baseline characteristics of patients with SV and reference subjects. A history of MI, in particular, and stroke was less common in patients with SV. Patients with SV presented more often with elevated CRP and had on average lower haemoglobin levels.
The frequency of STEMIs was slightly higher in patients with SV but there were no differences in treatment strategy, with equal proportion of patients undergoing angiography and percutaneous coronary intervention with stent implantation among patients with SV and their controls. There were no differences in the 1-year and 3-year mortality, hazard ratio (HR) of 1.16 (95% CI, 0.71-1.89) and 0.98 (95% CI, 0.64-1.49), respectively. Subgroup analyses investigating the 1-year all-cause mortality in AAV and GCA separately showed no outcome differences compared to controls, with HR 1.26 (95% CI, 0.52-3.08) and 1.11 (0.63-1.95) respectively.
Conclusion: In this population-based cohort, patients with systemic vasculitis suffering from myocardial infarction were less likely to have a previous history of cardiovascular events compared to controls. Apart from this, they had a comparable risk profile at presentation, were treated to the same extent with percutaneous coronary intervention and showed no difference in outcome compared to matched controls.
One- and 3-year all-cause mortality was not increased in patients with SV after their MI diagnosis.
The impact of glucocorticoids and other anti-inflammatory therapies on the risk of atherothrombosis and related outcomes should be further studied.
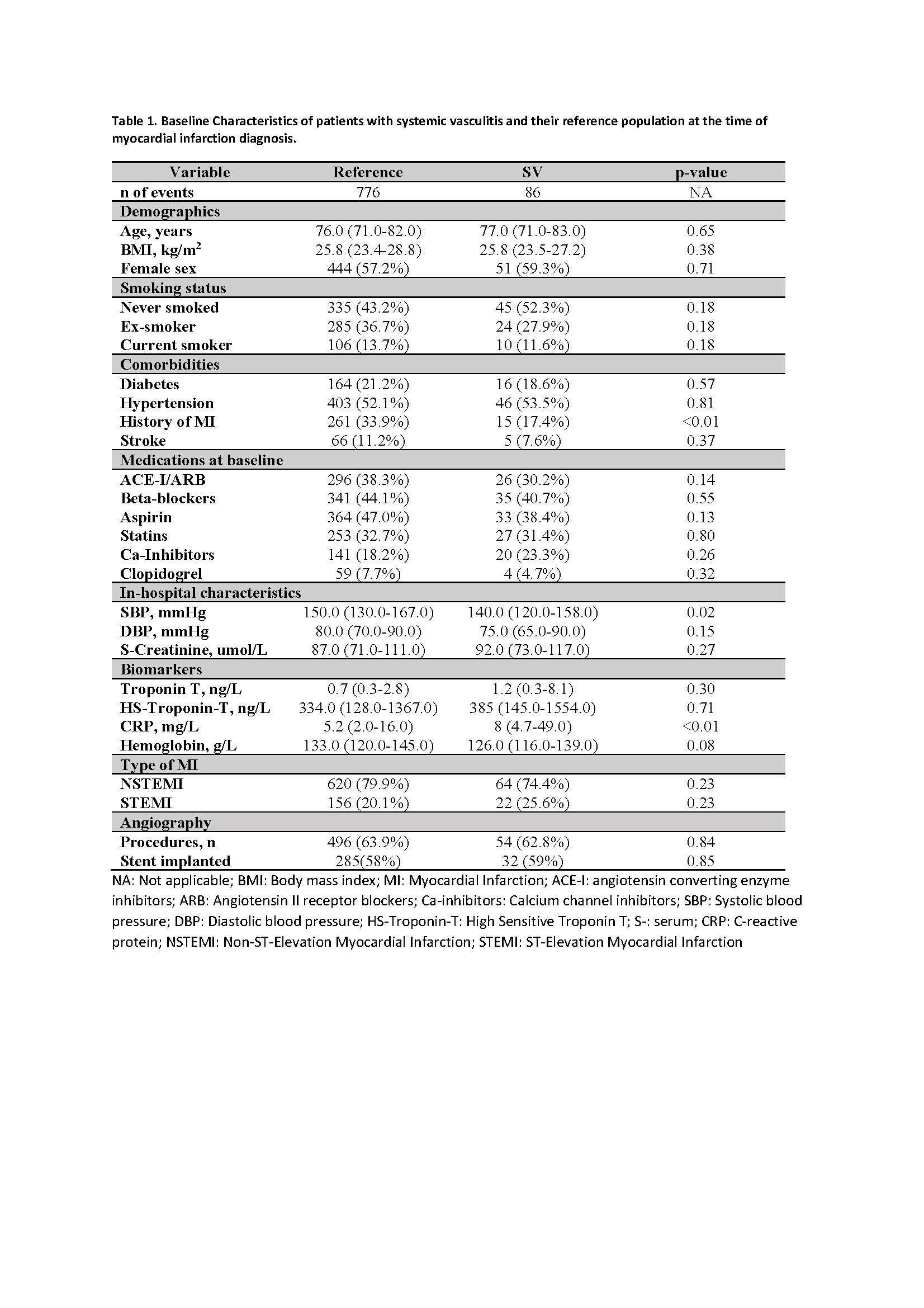 Table 1. Baseline Characteristics of patients with systemic vasculitis and their reference population at the time of myocardial infarction diagnosis
Table 1. Baseline Characteristics of patients with systemic vasculitis and their reference population at the time of myocardial infarction diagnosis
.jpg) Figure 1. One-year all-cause mortality
Figure 1. One-year all-cause mortality
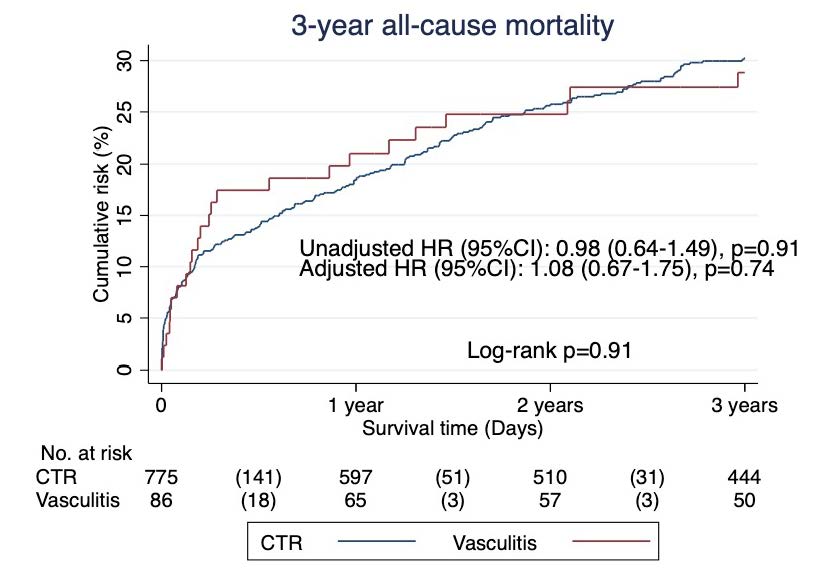 Figure 2. Three-year all-cause mortality
Figure 2. Three-year all-cause mortality
Disclosures: P. Stamatis, None; M. Mohammad, None; D. Erlinge, None; C. Turesson, AbbVie/Abbott, Nordic Drugs, Bristol-Myers Squibb(BMS); D. Jayne, Aurinia, AstraZeneca, GlaxoSmithKline (GSK), Roche/Genentech, Vifor, Bristol-Myers Squibb(BMS), Chemocentryx, Novartis, Takeda, Boehringer-Ingelheim, Otsuka, UCB, Amgen, Kessai; A. Mohammad, None.
Background/Purpose: The deleterious effect of inflammation combined with glucocorticoid treatment may increase the risk for atherosclerotic events. The aims of this study were to investigate differences in baseline characteristics and survival after incident MI in patients with systemic vasculitis [SV: ANCA-associated vasculitis (AAV) and Giant Cell Arteritis (GCA)] compared to a matched reference "non-vasculitis" population with MI.
Methods: The study cohort consisted of 1527 patients with SV (GCA n=1202; AAV n=325) diagnosed between 1997-2016 in Skåne, southern Sweden. Using a unique personal identification number, the SV cohort was linked to the national SWEDEHEART register which covers every coronary care unit admission in Sweden. All cases with SV diagnosed with acute MI after the onset of SV were identified and, matched with 10 controls (age, sex and year of MI diagnosis. Baseline characteristics were compared between SV-patients and controls. The risk for death at 1, and 3 years after the MI was assessed using a Cox regression model.
Results: A total of 86 patients (6%) were diagnosed with incident MI corresponding to proportions of 7% and 5% among AAV and GCA patients respectively. Table 1 presents the baseline characteristics of patients with SV and reference subjects. A history of MI, in particular, and stroke was less common in patients with SV. Patients with SV presented more often with elevated CRP and had on average lower haemoglobin levels.
The frequency of STEMIs was slightly higher in patients with SV but there were no differences in treatment strategy, with equal proportion of patients undergoing angiography and percutaneous coronary intervention with stent implantation among patients with SV and their controls. There were no differences in the 1-year and 3-year mortality, hazard ratio (HR) of 1.16 (95% CI, 0.71-1.89) and 0.98 (95% CI, 0.64-1.49), respectively. Subgroup analyses investigating the 1-year all-cause mortality in AAV and GCA separately showed no outcome differences compared to controls, with HR 1.26 (95% CI, 0.52-3.08) and 1.11 (0.63-1.95) respectively.
Conclusion: In this population-based cohort, patients with systemic vasculitis suffering from myocardial infarction were less likely to have a previous history of cardiovascular events compared to controls. Apart from this, they had a comparable risk profile at presentation, were treated to the same extent with percutaneous coronary intervention and showed no difference in outcome compared to matched controls.
One- and 3-year all-cause mortality was not increased in patients with SV after their MI diagnosis.
The impact of glucocorticoids and other anti-inflammatory therapies on the risk of atherothrombosis and related outcomes should be further studied.
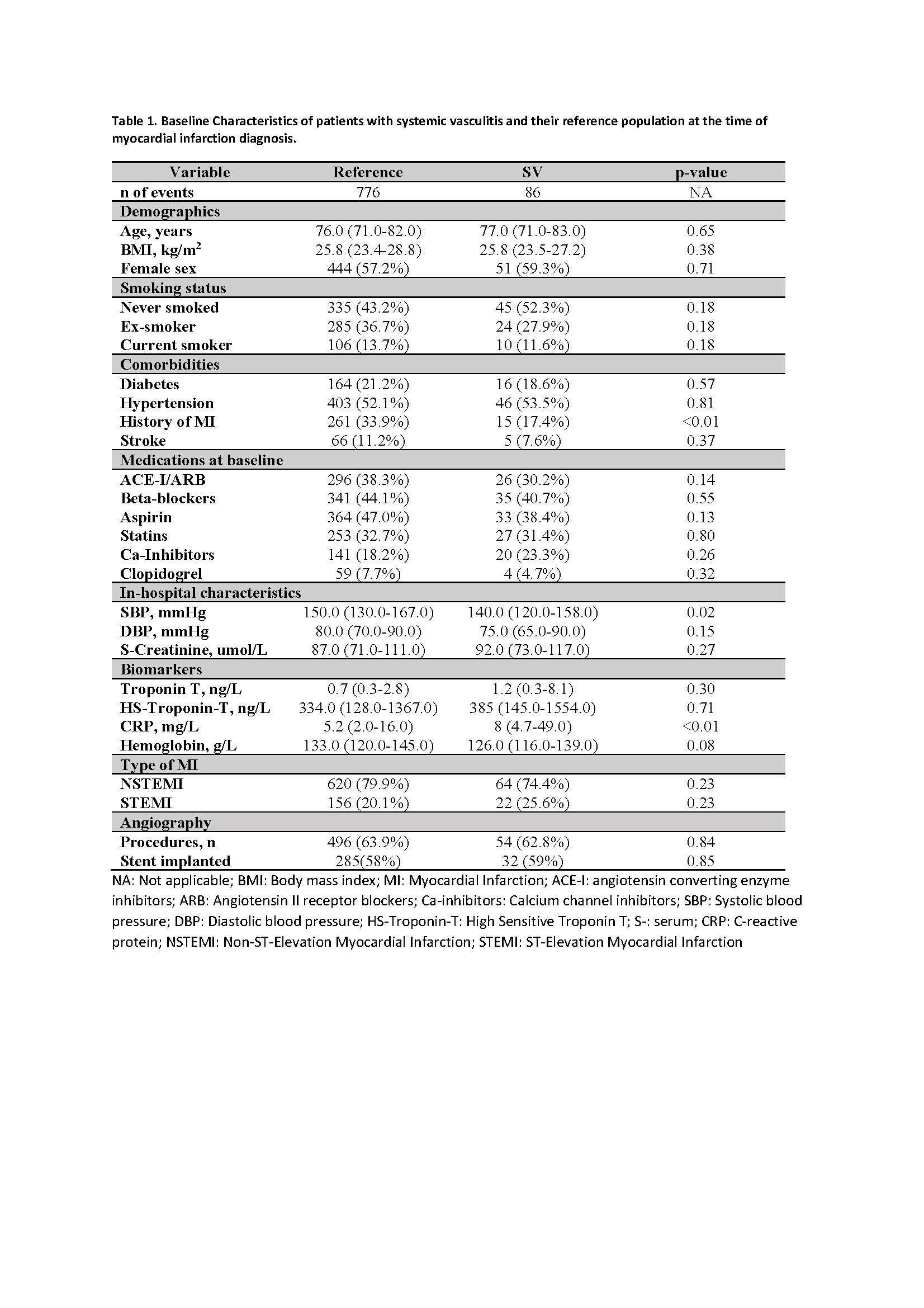 Table 1. Baseline Characteristics of patients with systemic vasculitis and their reference population at the time of myocardial infarction diagnosis
Table 1. Baseline Characteristics of patients with systemic vasculitis and their reference population at the time of myocardial infarction diagnosis.jpg) Figure 1. One-year all-cause mortality
Figure 1. One-year all-cause mortality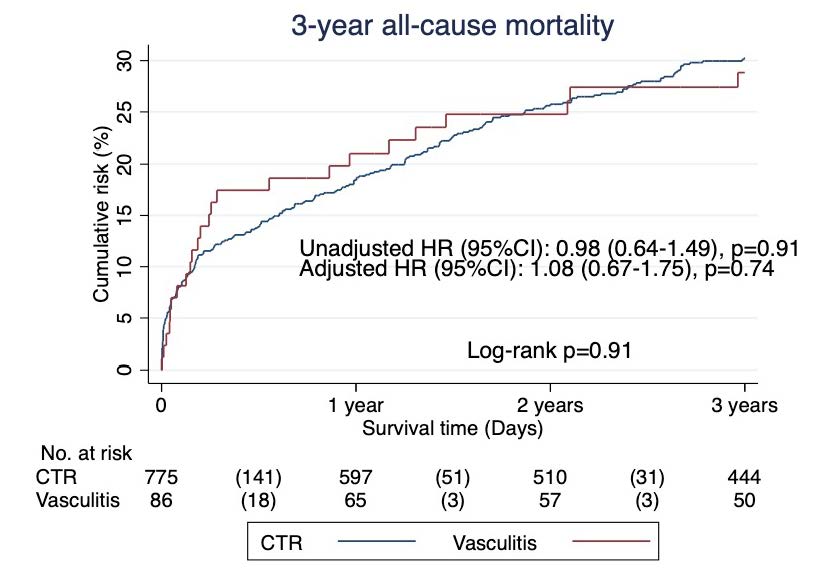 Figure 2. Three-year all-cause mortality
Figure 2. Three-year all-cause mortalityDisclosures: P. Stamatis, None; M. Mohammad, None; D. Erlinge, None; C. Turesson, AbbVie/Abbott, Nordic Drugs, Bristol-Myers Squibb(BMS); D. Jayne, Aurinia, AstraZeneca, GlaxoSmithKline (GSK), Roche/Genentech, Vifor, Bristol-Myers Squibb(BMS), Chemocentryx, Novartis, Takeda, Boehringer-Ingelheim, Otsuka, UCB, Amgen, Kessai; A. Mohammad, None.

