Back
Abstract Session
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes I: Diagnosis and Disease Activity (1609–1614)
1609: Comorbidity Clusters in Ankylosing Spondylitis and Their Association with Disease Activity and Functional Impairment: Data from the PSOAS Cohort
Sunday, November 13, 2022
4:30 PM – 4:40 PM Eastern Time
Location: Room 113
.jpg)
Paras Karmacharya, MD, MS
Vanderbilt University, Nashville, TN
Hermitage, TN, United States
Presenting Author(s)
Paras Karmacharya1, Cynthia Crowson2, Ryan Lennon3, Dilli Poudel4, John Davis3, Alexis Ogdie5, Jean Liew6, Michael Ward7, Mariko Ishimori8, Michael Weisman9, Matthew Brown10, Mohammad Rahbar11, Mark Hwang12, John Reveille13 and Lianne Gensler14, 1Vanderbilt University, Nashville, TN, 2Mayo Clinic, Eyota, MN, 3Mayo Clinic, Rochester, MN, 4Indiana Regional Medical Center, Indiana, PA, 5Department of Medicine, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, 6Boston University, Boston, MA, 7National Institutes of Health, Rockville, MD, 8Cedars-Sinai Health System, Los Angeles, CA, 9Adjunct Professor of Medicine, Stanford University; Distinguished Professor of Medicine Emeritus, David Geffen School of Medicine at UCLA, Los Angeles, CA, 10Genomics England, London, United Kingdom, 11University of Texas Health Science Center at Houston, Houston, TX, 12McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, 13University of Texas McGovern Medical School, Houston, TX, 14Department of Medicine, Division of Rheumatology, University of California San Francisco, San Francisco, CA
Background/Purpose: Comorbidities occur more frequently in patients with ankylosing spondylitis (AS) than in the general population and are associated with higher morbidity and mortality. Some comorbidities may be associated, making one more likely in the presence of another, and different combinations of comorbidities may have differential considerations for AS management and outcomes. The objective of our study was to examine the association of clusters of comorbidities at baseline with disease activity and functional status over time in AS.
Methods: We performed a longitudinal study from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort, a multicenter, prospective cohort from five centers (4 in the US, 1 in Australia). AS patients ≥ 18 years fulfilling modified New York criteria for AS (study period 2002-20) were included. Patient-reported AS comorbidities (N=28) and extra-musculoskeletal manifestations (EMMs) within 3 years of enrollment (pre-specified on the baseline case-report form) which occurred in ≥1%, were included. Undocumented comorbidities were assumed to be absent if missing in < 15% of patients, and those missing in >50% of patients were excluded. Comorbidity clusters were identified using K-median clustering. The optimal number of clusters was determined using a scree plot of the sum of squared errors. Baseline characteristics of the clusters were compared. Comorbidities and EMMs were collected at baseline and every 2 years, and the disease activity (ASDAS-CRP) and functional status (BASFI) measures were collected every 6 months. Generalized estimating equation models with an auto-regressive correlation structure (to account for multiple observations per patient) were used to examine the associations between comorbidity clusters and measures of disease activity and functional status over time.
Results: We included 1,270 AS patients (9,885 visits) with a mean age of 44.6 ±14.3 years, 74.4% male, and 80.1% white. Mean AS symptom duration was 21.6±14 years, 83% were HLA-B27 positive, and CRP was elevated in 42% of patients at baseline. The median follow-up was 2.9 years (IQ range: 1.0-6.8 years). Depression was the most prevalent comorbidity (33%) followed by hypertension (28%); uveitis was the most common EMM (34%). We identified five comorbidity clusters: depression (n=345, 27%), no comorbidities (n=281, 22%), hypertension (n=266, 21%), uveitis (n=249, 20%), and miscellaneous comorbidities (n=129, 10%) (Figure). The cluster with no comorbidities was significantly younger, with a lower symptom duration (p< 0.001). Depression and uveitis clusters had a significantly higher number of females (33% and 34% respectively) compared to the cluster with no comorbidities (20%). Patients in the depression cluster tended to have more comorbidities and worse disease activity and functional status compared to those with no comorbidities (Table).
Conclusion: Distinct comorbidity clusters were identified in AS patients in the PSOAS cohort. In addition to the number of comorbidities, the type of comorbidity seems to be important to longitudinal outcomes in AS. The depression cluster was associated with worse disease activity and function.
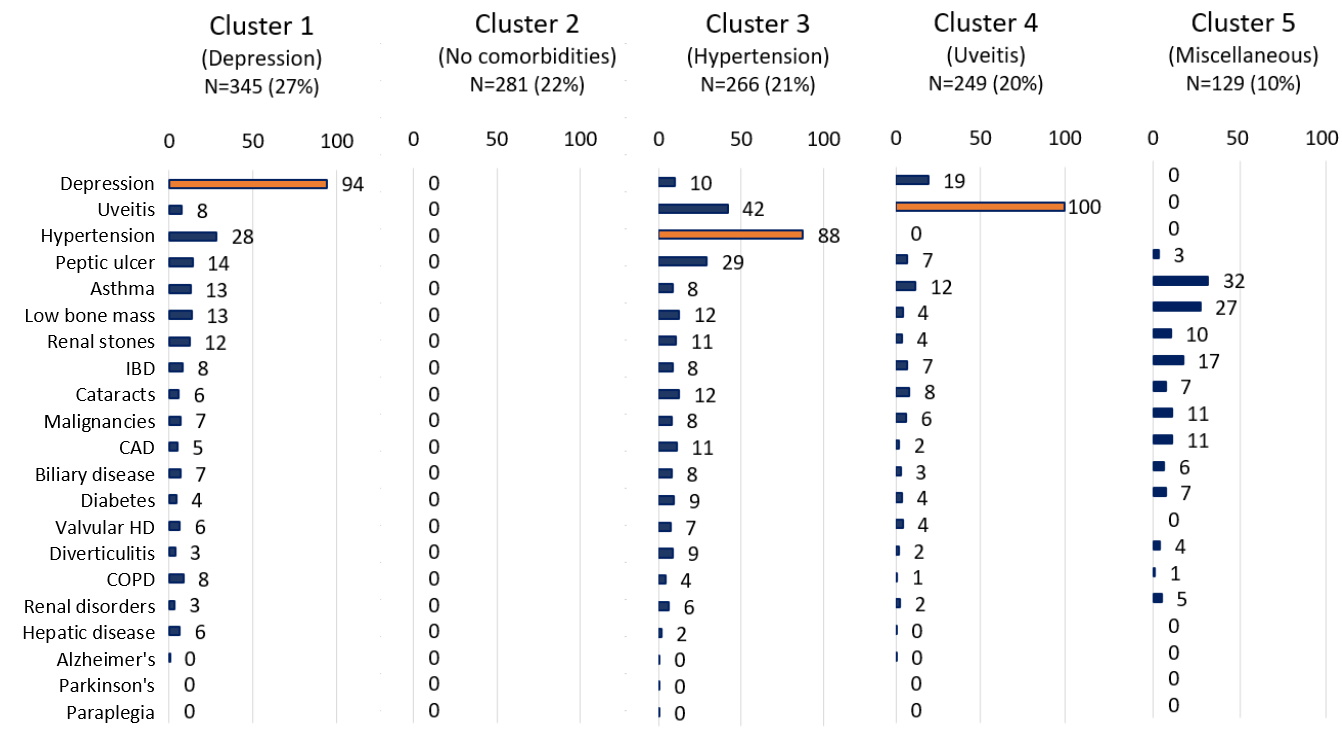 Figure. Baseline comorbidity clusters in ankylosing spondylitis from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort.
Figure. Baseline comorbidity clusters in ankylosing spondylitis from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort.
.jpg) Table. Age, sex, race, time from baseline adjusted associations between comorbidity clusters, compared to cluster 2 (no comorbidities), and disease activity/ functional status measures over time in ankylosing spondylitis based on generalized linear models.
Table. Age, sex, race, time from baseline adjusted associations between comorbidity clusters, compared to cluster 2 (no comorbidities), and disease activity/ functional status measures over time in ankylosing spondylitis based on generalized linear models.
Disclosures: P. Karmacharya, None; C. Crowson, None; R. Lennon, None; D. Poudel, None; J. Davis, Pfizer; A. Ogdie, AbbVie, Amgen, Novartis, Pfizer Inc, Bristol-Myers Squibb, Celgene, Janssen, CorEvitas, Gilead Sciences, Eli Lilly, GlaxoSmithKline, Happify Health, UCB; J. Liew, None; M. Ward, None; M. Ishimori, None; M. Weisman, None; M. Brown, UCB Pharma, Pfizer, Clementia, Ipsen, Incyte, Regeneron, Grey Wolf Therapeutics, Xinthera, Novartis; M. Rahbar, None; M. Hwang, Novartis; J. Reveille, Eli Lilly; L. Gensler, Novartis, Pfizer Inc, UCB Pharma, AbbVie, Eli Lilly, Janssen, Gilead, Moonlake.
Background/Purpose: Comorbidities occur more frequently in patients with ankylosing spondylitis (AS) than in the general population and are associated with higher morbidity and mortality. Some comorbidities may be associated, making one more likely in the presence of another, and different combinations of comorbidities may have differential considerations for AS management and outcomes. The objective of our study was to examine the association of clusters of comorbidities at baseline with disease activity and functional status over time in AS.
Methods: We performed a longitudinal study from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort, a multicenter, prospective cohort from five centers (4 in the US, 1 in Australia). AS patients ≥ 18 years fulfilling modified New York criteria for AS (study period 2002-20) were included. Patient-reported AS comorbidities (N=28) and extra-musculoskeletal manifestations (EMMs) within 3 years of enrollment (pre-specified on the baseline case-report form) which occurred in ≥1%, were included. Undocumented comorbidities were assumed to be absent if missing in < 15% of patients, and those missing in >50% of patients were excluded. Comorbidity clusters were identified using K-median clustering. The optimal number of clusters was determined using a scree plot of the sum of squared errors. Baseline characteristics of the clusters were compared. Comorbidities and EMMs were collected at baseline and every 2 years, and the disease activity (ASDAS-CRP) and functional status (BASFI) measures were collected every 6 months. Generalized estimating equation models with an auto-regressive correlation structure (to account for multiple observations per patient) were used to examine the associations between comorbidity clusters and measures of disease activity and functional status over time.
Results: We included 1,270 AS patients (9,885 visits) with a mean age of 44.6 ±14.3 years, 74.4% male, and 80.1% white. Mean AS symptom duration was 21.6±14 years, 83% were HLA-B27 positive, and CRP was elevated in 42% of patients at baseline. The median follow-up was 2.9 years (IQ range: 1.0-6.8 years). Depression was the most prevalent comorbidity (33%) followed by hypertension (28%); uveitis was the most common EMM (34%). We identified five comorbidity clusters: depression (n=345, 27%), no comorbidities (n=281, 22%), hypertension (n=266, 21%), uveitis (n=249, 20%), and miscellaneous comorbidities (n=129, 10%) (Figure). The cluster with no comorbidities was significantly younger, with a lower symptom duration (p< 0.001). Depression and uveitis clusters had a significantly higher number of females (33% and 34% respectively) compared to the cluster with no comorbidities (20%). Patients in the depression cluster tended to have more comorbidities and worse disease activity and functional status compared to those with no comorbidities (Table).
Conclusion: Distinct comorbidity clusters were identified in AS patients in the PSOAS cohort. In addition to the number of comorbidities, the type of comorbidity seems to be important to longitudinal outcomes in AS. The depression cluster was associated with worse disease activity and function.
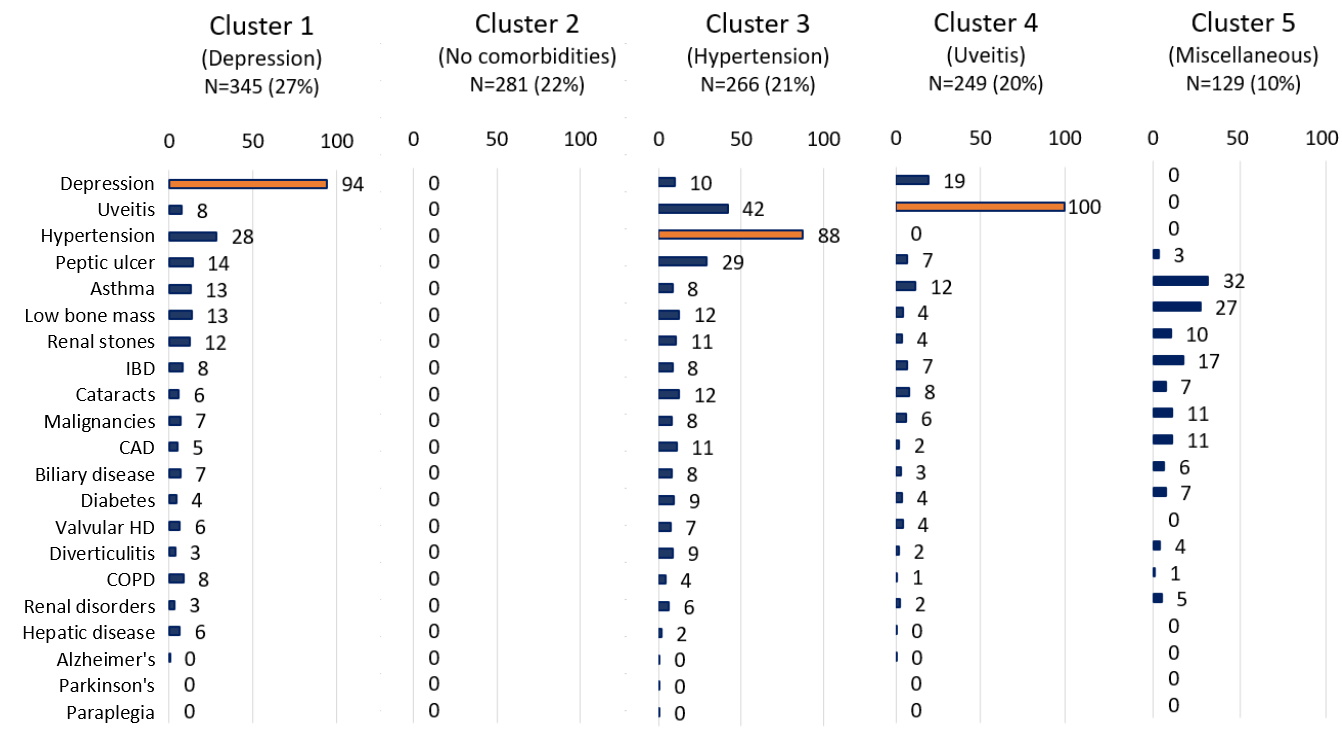 Figure. Baseline comorbidity clusters in ankylosing spondylitis from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort.
Figure. Baseline comorbidity clusters in ankylosing spondylitis from the Prospective Study Of Ankylosing Spondylitis (PSOAS) cohort..jpg) Table. Age, sex, race, time from baseline adjusted associations between comorbidity clusters, compared to cluster 2 (no comorbidities), and disease activity/ functional status measures over time in ankylosing spondylitis based on generalized linear models.
Table. Age, sex, race, time from baseline adjusted associations between comorbidity clusters, compared to cluster 2 (no comorbidities), and disease activity/ functional status measures over time in ankylosing spondylitis based on generalized linear models.Disclosures: P. Karmacharya, None; C. Crowson, None; R. Lennon, None; D. Poudel, None; J. Davis, Pfizer; A. Ogdie, AbbVie, Amgen, Novartis, Pfizer Inc, Bristol-Myers Squibb, Celgene, Janssen, CorEvitas, Gilead Sciences, Eli Lilly, GlaxoSmithKline, Happify Health, UCB; J. Liew, None; M. Ward, None; M. Ishimori, None; M. Weisman, None; M. Brown, UCB Pharma, Pfizer, Clementia, Ipsen, Incyte, Regeneron, Grey Wolf Therapeutics, Xinthera, Novartis; M. Rahbar, None; M. Hwang, Novartis; J. Reveille, Eli Lilly; L. Gensler, Novartis, Pfizer Inc, UCB Pharma, AbbVie, Eli Lilly, Janssen, Gilead, Moonlake.

