Back
Abstract Session
Osteoarthritis (OA) and related disorders
Session: Abstracts: Osteoarthritis – Clinical (1639–1644)
1643: Use of Oral Analgesics and Risk of Comorbidities in Osteoarthritis: Findings from Primary Care Settings in the UK
Monday, November 14, 2022
10:00 AM – 10:10 AM Eastern Time
Location: Room 120
- SS
Subhashisa Swain, PhD;PT;MPH
University of Oxford
Oxford, United Kingdom
Presenting Author(s)
Subhashisa Swain1, Carol Coupland2, Anne Kamps3, Jos Runhaar4, Andrea Dell ‘Isola5, Aleksandra Turkiewicz5, Danielle E Robinson1, Victoria Y Strauss1, Christian Mallen6, Chang-Fu Kuo7, Aliya Sarmanova8, Daniel Prieto Alhambra1, Martin Englund5, Sita Bierma-Zeinstra3, Michael Doherty2 and Weiya Zhang2, 1University of Oxford, Oxford, United Kingdom, 2University of Nottingham, Nottingham, United Kingdom, 3Erasmus University Medical Centre, Rotterdam, Netherlands, 4Erasmus Medical Center, Rotterdam, Netherlands, 5Lund University, Lund, Sweden, 6Keele University, Keele, United Kingdom, 7Chang Gung Memorial Hospital, Taoyuan, Taiwan, 8University of Bristol, Bristol, United Kingdom
Background/Purpose: People with osteoarthritis (OA) often have multiple other conditions (comorbidities).Role of different oral analgesics on the development of comorbidities in people with OA have only focused on few chronic conditions. We examined the contribution of paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids towards development of a wide range of comorbidities in people with and without OA.
Methods: This was an observational cohort study using the UK primary care Clinical Practice Research Datalink (CPRD) GOLD containing data on ~20 million people. We identified 261,273 people with incident OA and 261,273 controls matched for age (±2 years), sex, and practice in 1:1 ratio. Controls were assigned the same index date (the date of first diagnosis of OA) as their matched cases for the start of follow-up. We studied exposure to three types of analgesics prescriptions; paracetamol, NSAIDs, and opioids, separately. People with prescription or comorbidity outcome of study interest before the index date were excluded from the study. Analgesics exposure was defined as at least two prescriptions within 90 days, and was assessed every six months as yes/no until the end of the study/outcome of interest/death/last data available (maximum 22 years), whichever came first. Comorbidities were grouped into 9 categories as cancer, cardiovascular disease (CVD), endocrine, psychological, renal, gastrointestinal (GI), genitourinary, hepatic, and neurological conditions. Propensity scores for the prescription of each analgesic were calculated using a logistic regression model. The propensity score adjusted time varying exposure analysis was undertaken using a multivariable Cox model, and hazard ratios (HR) and 95% confidence interval (CI) were calculated. Smoking status, alcohol intake, propensity score, ever prescription of proton pump inhibitors (PPIs) and other comorbidities were adjusted in the Cox model.
Results: The mean age was 59.4 (12.8) years for people with OA and 60.2 (SD 12.8) years for controls, with 57.7% being female. Nearly two third people of OA had opioids prescriptions compared to one fifth in controls. (Table 1) People with OA using opioids or paracetamol exposure had nearly 1.2 to 2 times increased risks of developing all nine studied comorbidities. In people with OA and opioids users the hazards were 1.5 times higher for cancer, psychological and 1.2 to 1.5 times for GI, hepatic, CVD, neurological and endocrine conditions. Paracetamol users with OA had higher risk of respiratory comorbidities with GI, cancer, psychological comorbidities. NSAIDs exposure in OA was associated with cancer, CVD, GI, psychological, and renal comorbidities in people with OA. (Figure 1) Positive interaction between OA and NSAIDs was seen towards CVD and endocrine, between OA and paracetamol for endocrine, and OA and Opioids for renal comorbidities only.
Conclusion: People with OA using opioids or paracetamol had signfiicant association with more number of comorbidities. Interaction between OA and analgesics for all studied comorbidities were not commonly found. A careful approach must be taken while prescribing opioids and paracetamol for people with OA.
The study is supported by FOREUM.
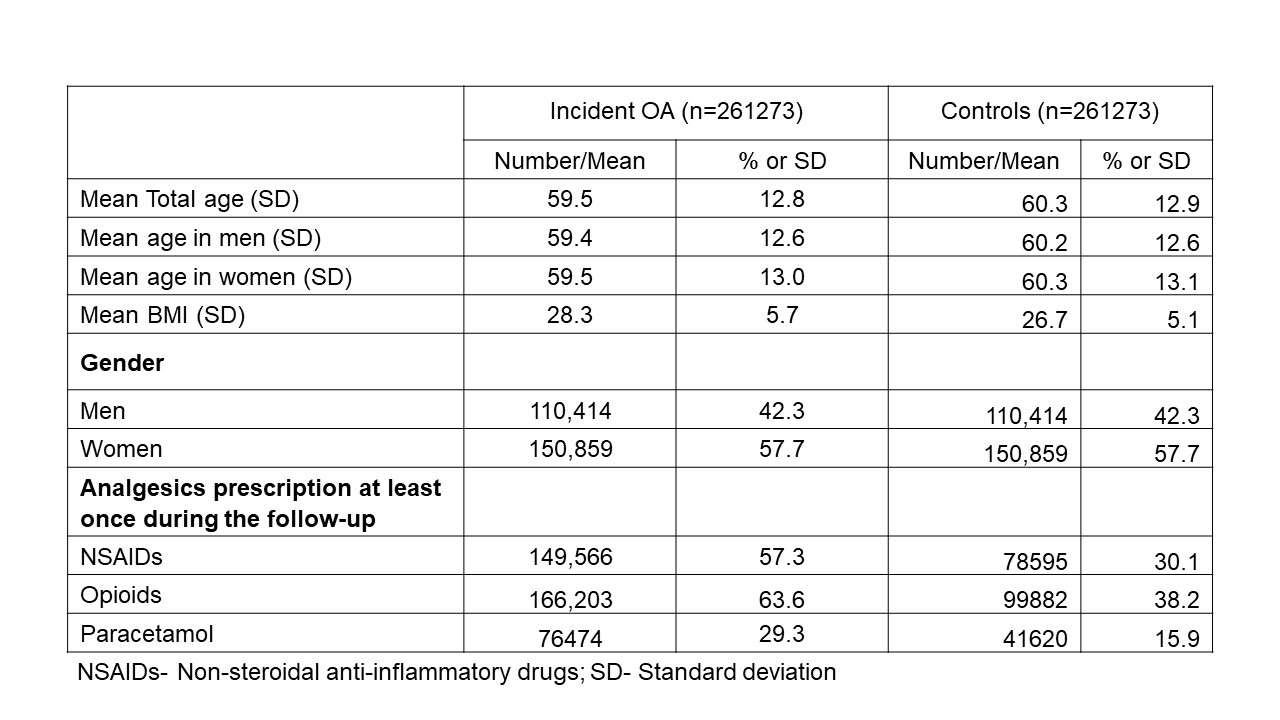
Table 1 Basic demographic characteristics at index date
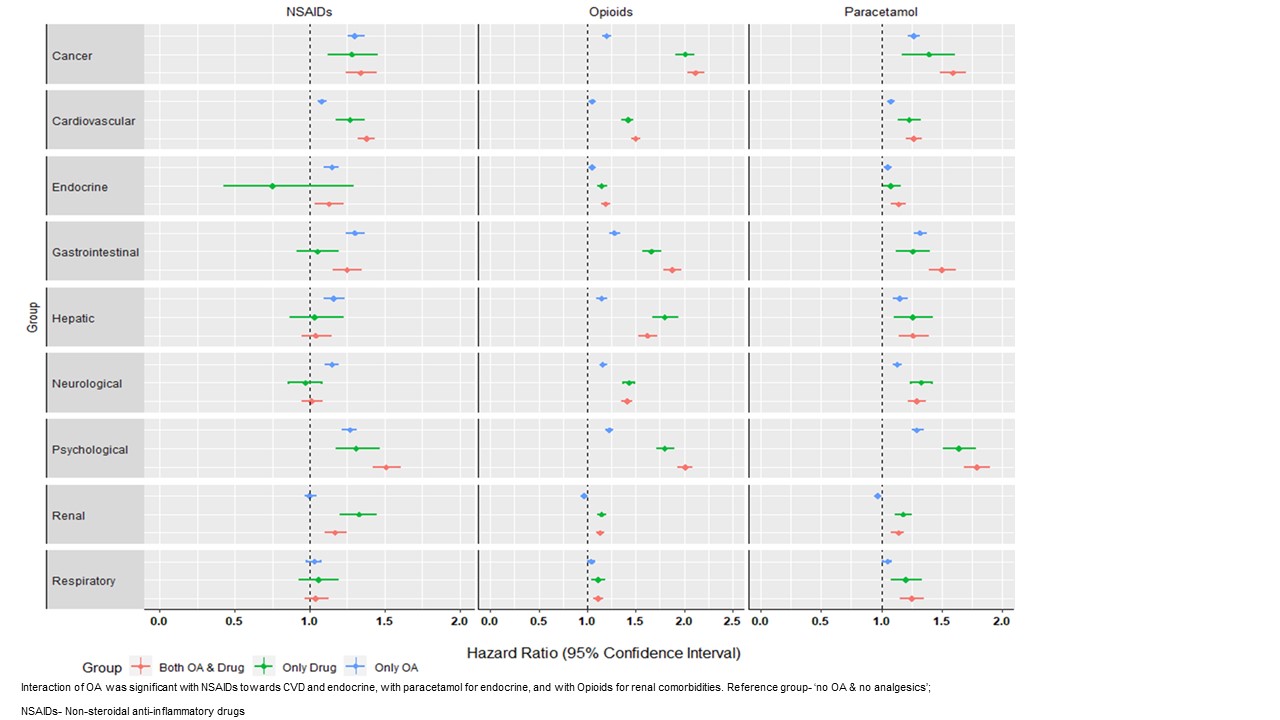 Figure 1- Adjusted hazard ratio for risk of developing comorbidities.
Figure 1- Adjusted hazard ratio for risk of developing comorbidities.
Disclosures: S. Swain, None; C. Coupland, None; A. Kamps, None; J. Runhaar, None; A. Dell ‘Isola, None; A. Turkiewicz, None; D. E Robinson, None; V. Y Strauss, None; C. Mallen, None; C. Kuo, None; A. Sarmanova, None; D. Prieto Alhambra, None; M. Englund, None; S. Bierma-Zeinstra, None; M. Doherty, None; W. Zhang, None.
Background/Purpose: People with osteoarthritis (OA) often have multiple other conditions (comorbidities).Role of different oral analgesics on the development of comorbidities in people with OA have only focused on few chronic conditions. We examined the contribution of paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids towards development of a wide range of comorbidities in people with and without OA.
Methods: This was an observational cohort study using the UK primary care Clinical Practice Research Datalink (CPRD) GOLD containing data on ~20 million people. We identified 261,273 people with incident OA and 261,273 controls matched for age (±2 years), sex, and practice in 1:1 ratio. Controls were assigned the same index date (the date of first diagnosis of OA) as their matched cases for the start of follow-up. We studied exposure to three types of analgesics prescriptions; paracetamol, NSAIDs, and opioids, separately. People with prescription or comorbidity outcome of study interest before the index date were excluded from the study. Analgesics exposure was defined as at least two prescriptions within 90 days, and was assessed every six months as yes/no until the end of the study/outcome of interest/death/last data available (maximum 22 years), whichever came first. Comorbidities were grouped into 9 categories as cancer, cardiovascular disease (CVD), endocrine, psychological, renal, gastrointestinal (GI), genitourinary, hepatic, and neurological conditions. Propensity scores for the prescription of each analgesic were calculated using a logistic regression model. The propensity score adjusted time varying exposure analysis was undertaken using a multivariable Cox model, and hazard ratios (HR) and 95% confidence interval (CI) were calculated. Smoking status, alcohol intake, propensity score, ever prescription of proton pump inhibitors (PPIs) and other comorbidities were adjusted in the Cox model.
Results: The mean age was 59.4 (12.8) years for people with OA and 60.2 (SD 12.8) years for controls, with 57.7% being female. Nearly two third people of OA had opioids prescriptions compared to one fifth in controls. (Table 1) People with OA using opioids or paracetamol exposure had nearly 1.2 to 2 times increased risks of developing all nine studied comorbidities. In people with OA and opioids users the hazards were 1.5 times higher for cancer, psychological and 1.2 to 1.5 times for GI, hepatic, CVD, neurological and endocrine conditions. Paracetamol users with OA had higher risk of respiratory comorbidities with GI, cancer, psychological comorbidities. NSAIDs exposure in OA was associated with cancer, CVD, GI, psychological, and renal comorbidities in people with OA. (Figure 1) Positive interaction between OA and NSAIDs was seen towards CVD and endocrine, between OA and paracetamol for endocrine, and OA and Opioids for renal comorbidities only.
Conclusion: People with OA using opioids or paracetamol had signfiicant association with more number of comorbidities. Interaction between OA and analgesics for all studied comorbidities were not commonly found. A careful approach must be taken while prescribing opioids and paracetamol for people with OA.
The study is supported by FOREUM.
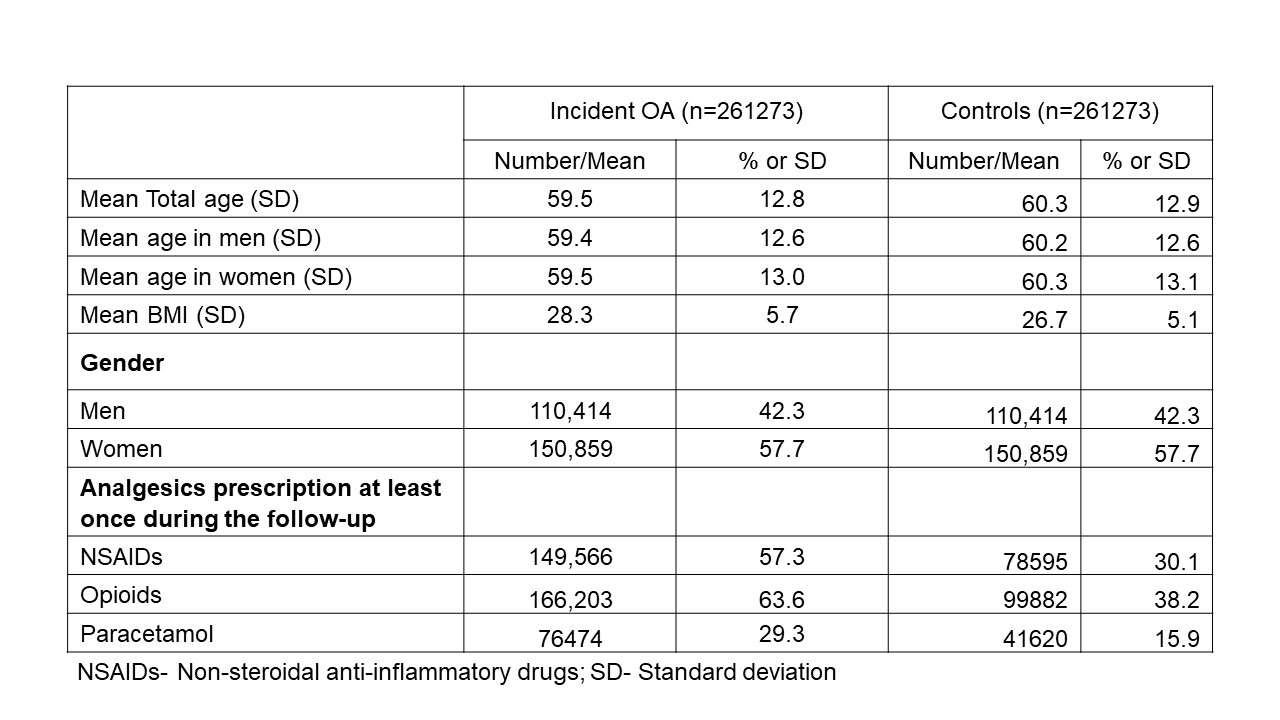
Table 1 Basic demographic characteristics at index date
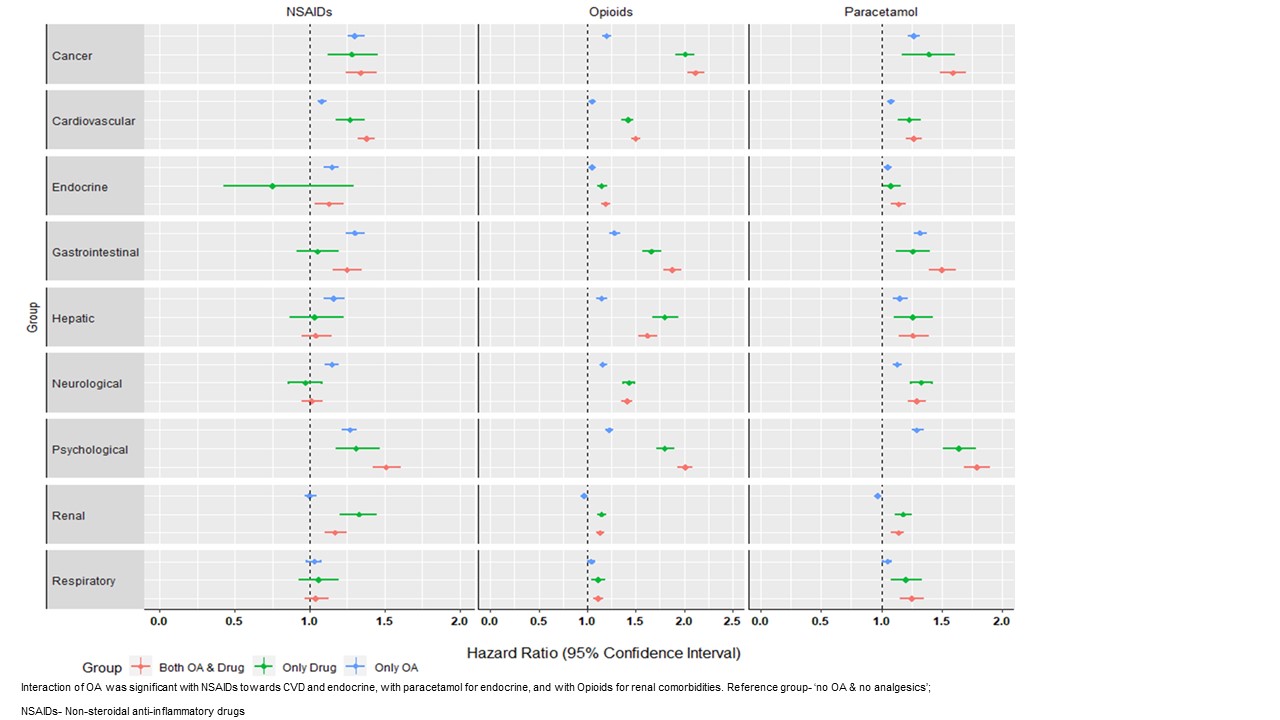 Figure 1- Adjusted hazard ratio for risk of developing comorbidities.
Figure 1- Adjusted hazard ratio for risk of developing comorbidities. Disclosures: S. Swain, None; C. Coupland, None; A. Kamps, None; J. Runhaar, None; A. Dell ‘Isola, None; A. Turkiewicz, None; D. E Robinson, None; V. Y Strauss, None; C. Mallen, None; C. Kuo, None; A. Sarmanova, None; D. Prieto Alhambra, None; M. Englund, None; S. Bierma-Zeinstra, None; M. Doherty, None; W. Zhang, None.

