Back
Abstract Session
Systemic lupus erythematosus (SLE)
Session: Abstracts: SLE – Treatment (1651–1656)
1656: Efficacy and Safety of Cenerimod in Patients with Moderate to Severe Systemic Lupus Erythematosus (SLE): A Multicenter, Randomized, Parallel-Group, Double-Blind, Placebo-Controlled, Dose-Finding Phase 2b Trial
Monday, November 14, 2022
10:15 AM – 10:25 AM Eastern Time
Location: Room 113
- AA
Anca Askanase, MD, MPH
Director
Columbia University Medical Center
New York, NY, United States
Presenting Author(s)
Anca Askanase1, Ouali Berkani2, clélia Cahuzac3, peter Cornelisse3, David D'Cruz4, Kenneth Kalunian5, Joan Merrill6, Marilia Pozzobon3 and Sandra Navarra7, 1Columbia University Medical Center, New York, NY, 2IDORSIA, Allschwil, Switzerland, 3Idorsia Pharmaceuticals Ltd, Allschwil, Switzerland, 4Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom, 5University of California San Diego, La Jolla, CA, 6Oklahoma Medical Research Foundation, Oklahoma City, OK, 7University of Santo Tomas, Manila, Philippines
Background/Purpose: Sphingosine-1-phosphate (S1P) regulates lymphocyte egress from lymphoid organs. In an SLE proof-of-concept study, cenerimod—a potent, selective S1P receptor modulator—reduced lymphocyte count and disease activity (measured by a SLEDAI-2K modified to exclude leukopenia [mSLEDAI-2K]) vs placebo (PBO) (Hermann. Lupus Sci Med 2019;6:e000354). The current phase 2 study (CARE) evaluated efficacy and safety of 4 cenerimod doses in moderate to severe SLE (NCT03742037).
Methods: Patients with SLE, mSLEDAI-2K ≥6 and current or past ANA or anti-dsDNA were randomized to daily oral cenerimod (0.5, 1, 2 or 4 mg) or PBO. Background SLE medication had to be stable for ≥30 days pre-randomization (corticosteroids ≥15 days).
Study duration was 18 months (M), two 6M treatment periods and a 6M follow-up. After the first 6M, patients on cenerimod 4 mg were rerandomized to cenerimod 2 mg or PBO to assess reversibility of lymphopenia and potential withdrawal effects.
The primary endpoint was change from baseline (BL) to M6 in mSLEDAI-2K. Secondary endpoints were SLE Responder Index SRI-4 and BILAG-2004 improvement. Safety endpoints included adverse events (AEs) and AEs of special interest (AESI). The Hochberg procedure was used to compare endpoints within each endpoint family and hierarchically within each dose across endpoints to preserve a 5% 2-sided Type I family-wise error rate.
Results: Of 427 randomized patients, 339 completed 12M of treatment. BL characteristics were balanced across groups (Table 1). The study did not meet its primary endpoint after type I error control. In an exploratory analysis the reduction in mSLEDAI-2K from BL to M6 at cenerimod 4 mg vs PBO was statistically significant without accounting for type I error control; least squares [LS] mean difference (95% CI) -1.19(-2.25, -0.12), nominal P=0.0291 (Table 2). This effect was greater in patients with greater disease severity (BILAG-2004 Grade B in ≥2 organ systems and/or Grade A in ≥1 organ system at BL) (LS mean difference [95%CI] -1.39[-2.59, -0.19]) and high IFN-1 gene expression signature status (LS mean difference [95%CI] -2.79[-4.50, -1.08]) vs the overall population. At M6 and M12, the proportion of SRI-4 responders was higher in patients randomized to cenerimod 4 mg in the first 6M. This difference was also greater in high IFN-1 patients (difference +24% at M6 and +8% at M12). Sustained mSLEDAI-2K response started earlier in patients on cenerimod 4 mg vs PBO; this difference was greater in the IFN-1 high subgroup vs the overall population (Figure). Lymphocyte count decreased in all cenerimod groups; greater decreases were seen with the 2 and 4 mg doses and recovered by M12 in those rerandomized to PBO.
AEs were similar across treatment groups (Table 2). The % of reported hypertension AEs was higher in the cenerimod 1 and 4 mg groups vs PBO; however monthly objective measurements showed no increases in mean systolic or diastolic blood pressure. AESI were mild and transient; 1 death due to acute coronary syndrome occurred (1 mg group).
Conclusion: Cenerimod in patients with SLE was generally well tolerated. Exploratory analysis suggests that cenerimod 4 mg might improve disease and warrants further study, especially in IFN-1 high patients and greater disease severity.
.jpg) Table 1. Baseline patient and disease characteristics
Table 1. Baseline patient and disease characteristics
.jpg) Table 2. Efficacy outcomes at Month 6 and Month 12 and safety outcomes at Month 12
Table 2. Efficacy outcomes at Month 6 and Month 12 and safety outcomes at Month 12
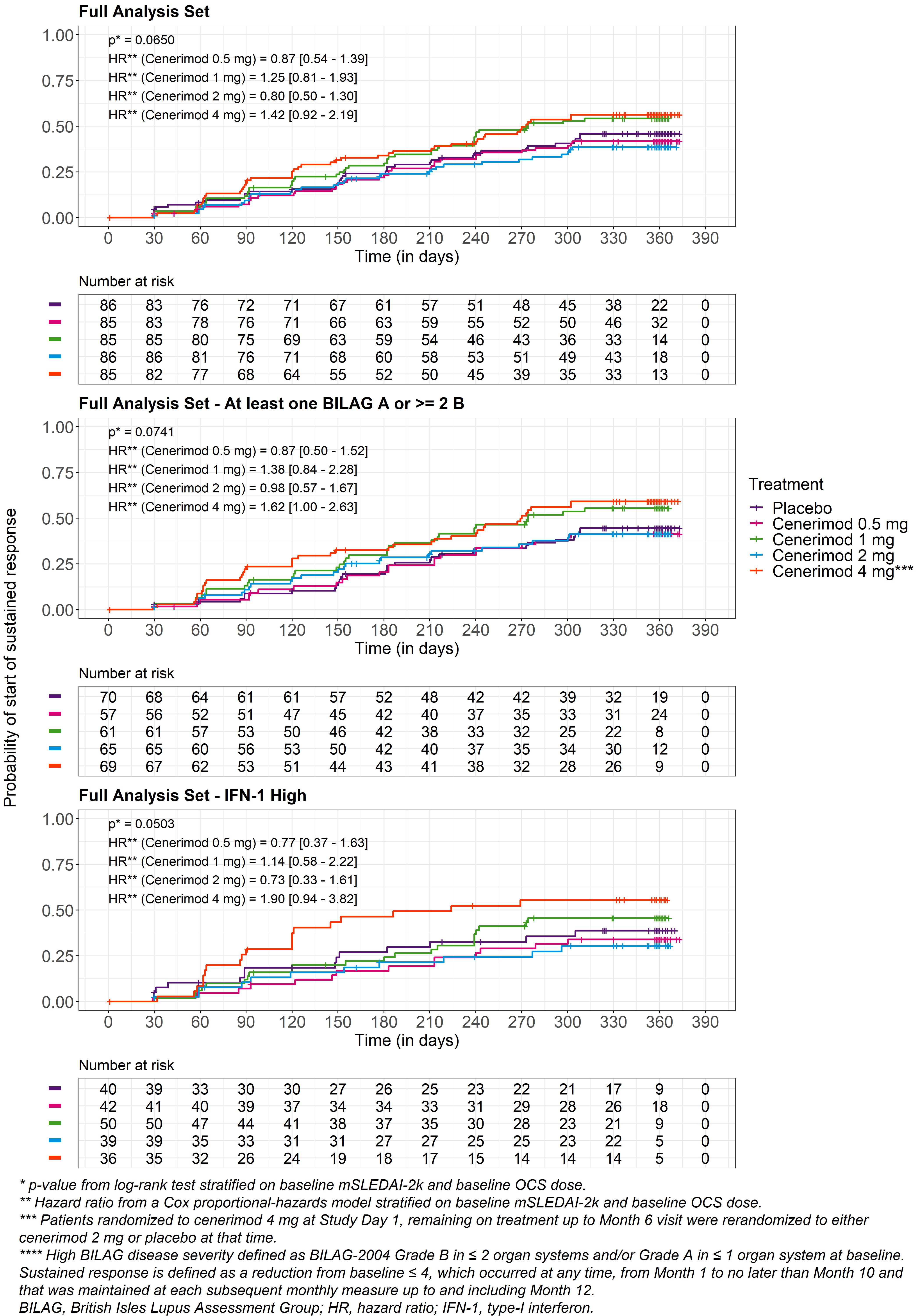 Figure. Sustained response in A, full analysis set; B, patients with high BILAG severity****; C, patients with high IFN-1 signature
Figure. Sustained response in A, full analysis set; B, patients with high BILAG severity****; C, patients with high IFN-1 signature
Disclosures: A. Askanase, AstraZeneca, GlaxoSmithKlein(GSK), Aurinia, Amgen, Pfizer, Idorsia, Eli Lilly, UCB, AbbVie/Abbott, Janssen, Bristol-Myers Squibb(BMS); O. Berkani, Idorsia pharmaceuticals Ltd; c. Cahuzac, Idorsia Pharmaceuticals Ltd; p. Cornelisse, Idorsia Pharmaceuticals Ltd; D. D'Cruz, GlaxoSmithKlein(GSK), UCB, Vifor, Eli Lilly, Idorsia; K. Kalunian, AbbVie/Abbott, Amgen, AstraZeneca, Aurinia, Biogen, Bristol Myers Squibb (BMS), Eli Lilly, Equillium, Genentech, Gilead, Janssen, Roche, Lupus Research Alliance, Pfizer, Sanford Consortium, Viela, Nektar; J. Merrill, UCB, GlaxoSmithKline, AbbVie, EMD Serono, Remegen, Celgene/Bristol Myers Squibb, AstraZeneca, Amgen, Janssen, Lilly, Genentech, Aurinia, Astellas, Alexion, Sanofi, Zenas, Proventio; M. Pozzobon, Idorsia Pharmaceuticals Ltd; S. Navarra, Biogen, Astellas, Janssen, Novartis, Pfizer, Boehringer-Ingelheim, GlaxoSmithKline (GSK).
Background/Purpose: Sphingosine-1-phosphate (S1P) regulates lymphocyte egress from lymphoid organs. In an SLE proof-of-concept study, cenerimod—a potent, selective S1P receptor modulator—reduced lymphocyte count and disease activity (measured by a SLEDAI-2K modified to exclude leukopenia [mSLEDAI-2K]) vs placebo (PBO) (Hermann. Lupus Sci Med 2019;6:e000354). The current phase 2 study (CARE) evaluated efficacy and safety of 4 cenerimod doses in moderate to severe SLE (NCT03742037).
Methods: Patients with SLE, mSLEDAI-2K ≥6 and current or past ANA or anti-dsDNA were randomized to daily oral cenerimod (0.5, 1, 2 or 4 mg) or PBO. Background SLE medication had to be stable for ≥30 days pre-randomization (corticosteroids ≥15 days).
Study duration was 18 months (M), two 6M treatment periods and a 6M follow-up. After the first 6M, patients on cenerimod 4 mg were rerandomized to cenerimod 2 mg or PBO to assess reversibility of lymphopenia and potential withdrawal effects.
The primary endpoint was change from baseline (BL) to M6 in mSLEDAI-2K. Secondary endpoints were SLE Responder Index SRI-4 and BILAG-2004 improvement. Safety endpoints included adverse events (AEs) and AEs of special interest (AESI). The Hochberg procedure was used to compare endpoints within each endpoint family and hierarchically within each dose across endpoints to preserve a 5% 2-sided Type I family-wise error rate.
Results: Of 427 randomized patients, 339 completed 12M of treatment. BL characteristics were balanced across groups (Table 1). The study did not meet its primary endpoint after type I error control. In an exploratory analysis the reduction in mSLEDAI-2K from BL to M6 at cenerimod 4 mg vs PBO was statistically significant without accounting for type I error control; least squares [LS] mean difference (95% CI) -1.19(-2.25, -0.12), nominal P=0.0291 (Table 2). This effect was greater in patients with greater disease severity (BILAG-2004 Grade B in ≥2 organ systems and/or Grade A in ≥1 organ system at BL) (LS mean difference [95%CI] -1.39[-2.59, -0.19]) and high IFN-1 gene expression signature status (LS mean difference [95%CI] -2.79[-4.50, -1.08]) vs the overall population. At M6 and M12, the proportion of SRI-4 responders was higher in patients randomized to cenerimod 4 mg in the first 6M. This difference was also greater in high IFN-1 patients (difference +24% at M6 and +8% at M12). Sustained mSLEDAI-2K response started earlier in patients on cenerimod 4 mg vs PBO; this difference was greater in the IFN-1 high subgroup vs the overall population (Figure). Lymphocyte count decreased in all cenerimod groups; greater decreases were seen with the 2 and 4 mg doses and recovered by M12 in those rerandomized to PBO.
AEs were similar across treatment groups (Table 2). The % of reported hypertension AEs was higher in the cenerimod 1 and 4 mg groups vs PBO; however monthly objective measurements showed no increases in mean systolic or diastolic blood pressure. AESI were mild and transient; 1 death due to acute coronary syndrome occurred (1 mg group).
Conclusion: Cenerimod in patients with SLE was generally well tolerated. Exploratory analysis suggests that cenerimod 4 mg might improve disease and warrants further study, especially in IFN-1 high patients and greater disease severity.
.jpg) Table 1. Baseline patient and disease characteristics
Table 1. Baseline patient and disease characteristics.jpg) Table 2. Efficacy outcomes at Month 6 and Month 12 and safety outcomes at Month 12
Table 2. Efficacy outcomes at Month 6 and Month 12 and safety outcomes at Month 12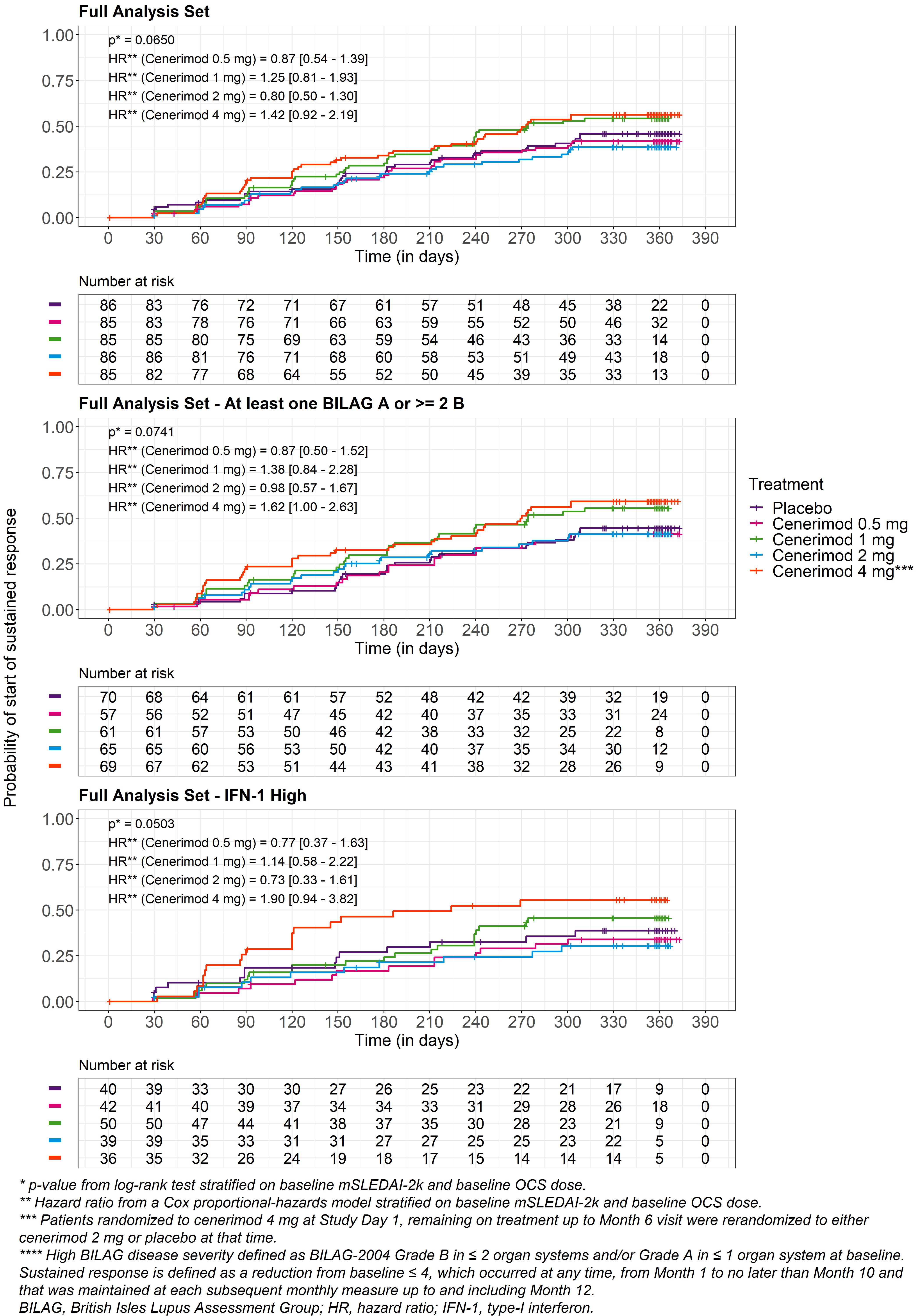 Figure. Sustained response in A, full analysis set; B, patients with high BILAG severity****; C, patients with high IFN-1 signature
Figure. Sustained response in A, full analysis set; B, patients with high BILAG severity****; C, patients with high IFN-1 signatureDisclosures: A. Askanase, AstraZeneca, GlaxoSmithKlein(GSK), Aurinia, Amgen, Pfizer, Idorsia, Eli Lilly, UCB, AbbVie/Abbott, Janssen, Bristol-Myers Squibb(BMS); O. Berkani, Idorsia pharmaceuticals Ltd; c. Cahuzac, Idorsia Pharmaceuticals Ltd; p. Cornelisse, Idorsia Pharmaceuticals Ltd; D. D'Cruz, GlaxoSmithKlein(GSK), UCB, Vifor, Eli Lilly, Idorsia; K. Kalunian, AbbVie/Abbott, Amgen, AstraZeneca, Aurinia, Biogen, Bristol Myers Squibb (BMS), Eli Lilly, Equillium, Genentech, Gilead, Janssen, Roche, Lupus Research Alliance, Pfizer, Sanford Consortium, Viela, Nektar; J. Merrill, UCB, GlaxoSmithKline, AbbVie, EMD Serono, Remegen, Celgene/Bristol Myers Squibb, AstraZeneca, Amgen, Janssen, Lilly, Genentech, Aurinia, Astellas, Alexion, Sanofi, Zenas, Proventio; M. Pozzobon, Idorsia Pharmaceuticals Ltd; S. Navarra, Biogen, Astellas, Janssen, Novartis, Pfizer, Boehringer-Ingelheim, GlaxoSmithKline (GSK).

