Back
Abstract Session
Epidemiology, health policy and outcomes
Session: Abstracts: Epidemiology and Public Health I: Risk Factors and Outcomes (1633–1638)
1638: Epidemiology of Rheumatoid Arthritis and Rheumatoid Arthritis-Interstitial Lung Disease in the Veterans Health Administration from 2004 to 2018
Monday, November 14, 2022
10:15 AM – 10:25 AM Eastern Time
Location: Room 204
.png)
Bryant England, MD, PhD, RhMSUS
University of Nebraska Medical Center
Omaha, NE, United States
Presenting Author(s)
Benjamin Fletcher1, Punyasha Roul2, Yangyuna Yang3, Brian Sauer4, Jorge Rojas5, Grant Cannon6, Joshua Baker7, Ted Mikuls8 and Bryant England3, 1University of Nebraska Medical Center, Omaha, 2UNMC, Omaha, NE, 3University of Nebraska Medical Center, Omaha, NE, 4Salt Lake City VA/University of Utah, Salt Lake City, UT, 5George E. Wahlen Department of Veterans Affairs Salt Lake City Health Care System, Salt Lake City, UT, 6Salt Lake City VA, Salt Lake city, 7University of Pennsylvania and Corporal Michael J. Crescenz VA Medical Center, Philadelphia, 8Division of Rheumatology, University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Epidemiologic studies estimating RA prevalence and incidence have primarily been conducted in populations where the majority of RA patients are women. Because of phenotypic differences in RA between men and women that include a higher frequency of extra-articular features (e.g. RA-interstitial lung disease [RA-ILD]) in men, precise epidemiologic estimates in male predominant populations are also needed. The Veterans Health Administration (VHA) is the largest integrated healthcare system in the U.S. and serves a male predominant population. The purpose of this study was to characterize the epidemiology of RA and RA-ILD within the VHA from 2004 to 2018.
Methods: We queried national VHA data within the Corporate Data Warehouse from 2000 through 2018 for RA and ILD diagnostic codes, provider specialty and specialty diagnoses, DMARD fills, and RA autoantibody status. Previously validated prevalent and incident RA algorithms ( >90% PPV) as well as ILD algorithms ( >75% PPV) were applied to national VHA data to estimate the epidemiology of RA and RA-ILD between 2004-2018, excluding the years 2000-2003 to avoid misclassification of incident/prevalent disease due to recent adoption of the electronic health record. The incidence and prevalence of RA among individuals receiving VHA care as well as the incidence and prevalence of ILD among RA patients were estimated annually with 95% CI calculated using the Wald interval. Using 2018 data, estimates were performed among subgroups defined by gender, age, race, and ethnicity. In sensitivity analyses, we estimated the prevalence of RA and RA-ILD using variations of RA and RA-ILD algorithms with greater sensitivity.
Results: During our study window, we identified 68,280 patients with RA and 4,301 patients with RA-ILD. From 2004 to 2018, the annual RA prevalence in the VHA increased from 0.41% to 0.67% while disease incidence remained stable (range 54 to 75 per 100,000 person-years) (Figure 1A-B). Among RA patients, RA-ILD annual prevalence increased from 1.71% to 4.48% and incidence similarly increased from 34 to 97 cases per 10,000 person-years over the same period (Figure 1C-D). Sensitivity analyses with more sensitive RA and RA-ILD algorithms estimated a modestly higher disease prevalence (0.76% RA, 4.88% RA-ILD) in 2018. In subgroup analyses, RA prevalence was higher in females than males (0.95% vs 0.64%) and highest amongst patients aged 60-79 years (0.93%) and reporting White non-Hispanic race and ethnicity (0.72%) (Table 1). RA-ILD was more prevalent in males than females (4.81% vs 2.53%) and among patients over the age of 60 years (Table 1).
Conclusion: Within the VHA from 2004 to 2018 the incidence of RA was stable while prevalence gradually increased, perhaps reflecting improvements in survival that have been reported in RA cohorts. The estimated prevalence of RA in males was higher in the VHA than other RA cohorts and may be related to differences in environmental exposures (e.g. smoking, military related). While the rising prevalence and incidence of RA-ILD could result from improved disease awareness and screening, it also indicates that the burden of RA-ILD likely remains underestimated in this population.
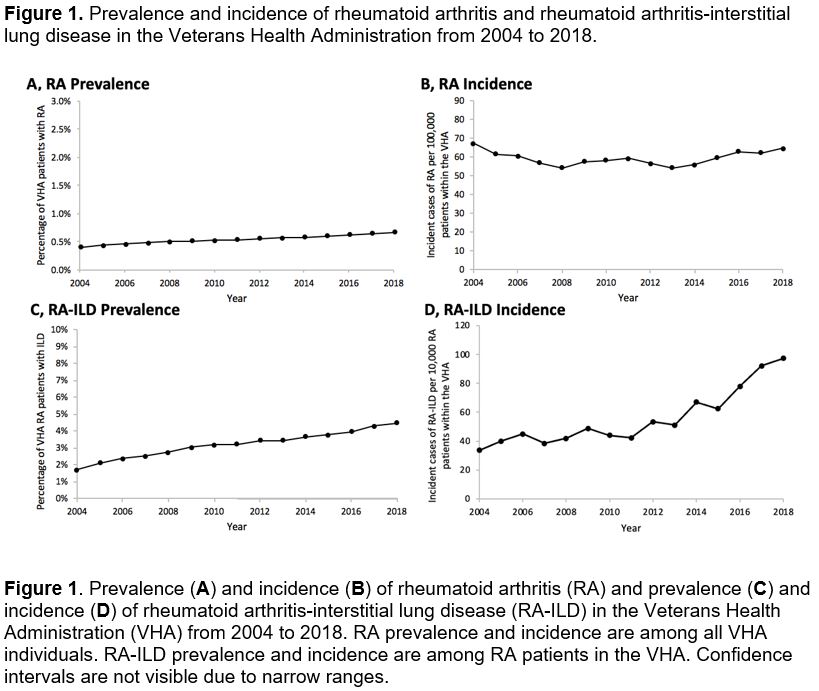 Figure 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-interstitial lung disease in the Veterans Health Administration from 2004 to 2018.
Figure 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-interstitial lung disease in the Veterans Health Administration from 2004 to 2018.
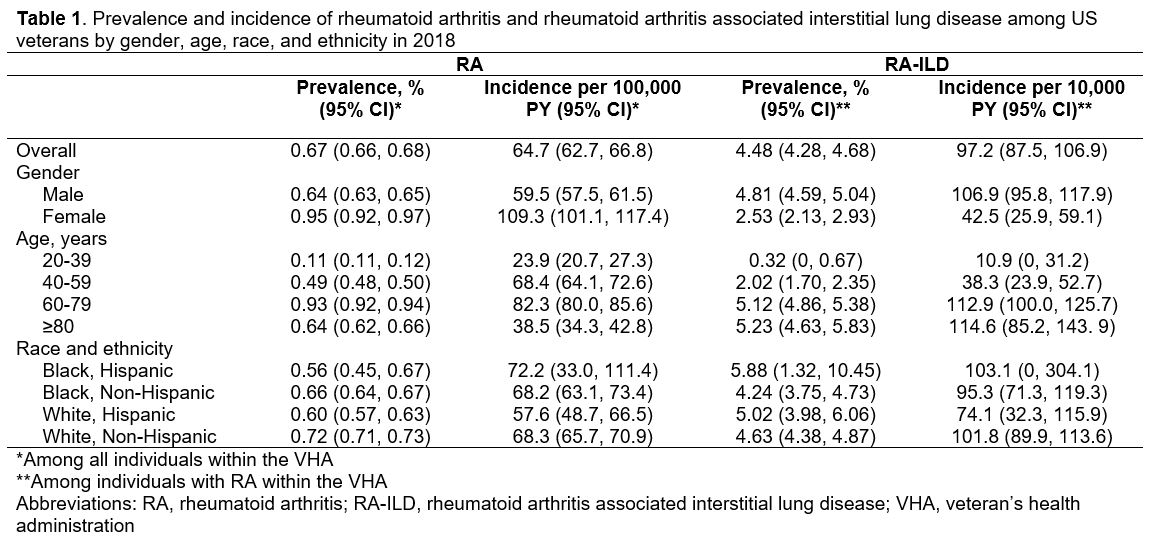 Table 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-associated interstitial lung disease among US veterans by gender, age, race, and ethnicity in 2018
Table 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-associated interstitial lung disease among US veterans by gender, age, race, and ethnicity in 2018
Disclosures: B. Fletcher, None; P. Roul, None; Y. Yang, None; B. Sauer, None; J. Rojas, None; G. Cannon, None; J. Baker, Bristol Myers Squibb, Pfizer, CorEvitas LLC, Burns-White, LLC, RediTrex; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.
Background/Purpose: Epidemiologic studies estimating RA prevalence and incidence have primarily been conducted in populations where the majority of RA patients are women. Because of phenotypic differences in RA between men and women that include a higher frequency of extra-articular features (e.g. RA-interstitial lung disease [RA-ILD]) in men, precise epidemiologic estimates in male predominant populations are also needed. The Veterans Health Administration (VHA) is the largest integrated healthcare system in the U.S. and serves a male predominant population. The purpose of this study was to characterize the epidemiology of RA and RA-ILD within the VHA from 2004 to 2018.
Methods: We queried national VHA data within the Corporate Data Warehouse from 2000 through 2018 for RA and ILD diagnostic codes, provider specialty and specialty diagnoses, DMARD fills, and RA autoantibody status. Previously validated prevalent and incident RA algorithms ( >90% PPV) as well as ILD algorithms ( >75% PPV) were applied to national VHA data to estimate the epidemiology of RA and RA-ILD between 2004-2018, excluding the years 2000-2003 to avoid misclassification of incident/prevalent disease due to recent adoption of the electronic health record. The incidence and prevalence of RA among individuals receiving VHA care as well as the incidence and prevalence of ILD among RA patients were estimated annually with 95% CI calculated using the Wald interval. Using 2018 data, estimates were performed among subgroups defined by gender, age, race, and ethnicity. In sensitivity analyses, we estimated the prevalence of RA and RA-ILD using variations of RA and RA-ILD algorithms with greater sensitivity.
Results: During our study window, we identified 68,280 patients with RA and 4,301 patients with RA-ILD. From 2004 to 2018, the annual RA prevalence in the VHA increased from 0.41% to 0.67% while disease incidence remained stable (range 54 to 75 per 100,000 person-years) (Figure 1A-B). Among RA patients, RA-ILD annual prevalence increased from 1.71% to 4.48% and incidence similarly increased from 34 to 97 cases per 10,000 person-years over the same period (Figure 1C-D). Sensitivity analyses with more sensitive RA and RA-ILD algorithms estimated a modestly higher disease prevalence (0.76% RA, 4.88% RA-ILD) in 2018. In subgroup analyses, RA prevalence was higher in females than males (0.95% vs 0.64%) and highest amongst patients aged 60-79 years (0.93%) and reporting White non-Hispanic race and ethnicity (0.72%) (Table 1). RA-ILD was more prevalent in males than females (4.81% vs 2.53%) and among patients over the age of 60 years (Table 1).
Conclusion: Within the VHA from 2004 to 2018 the incidence of RA was stable while prevalence gradually increased, perhaps reflecting improvements in survival that have been reported in RA cohorts. The estimated prevalence of RA in males was higher in the VHA than other RA cohorts and may be related to differences in environmental exposures (e.g. smoking, military related). While the rising prevalence and incidence of RA-ILD could result from improved disease awareness and screening, it also indicates that the burden of RA-ILD likely remains underestimated in this population.
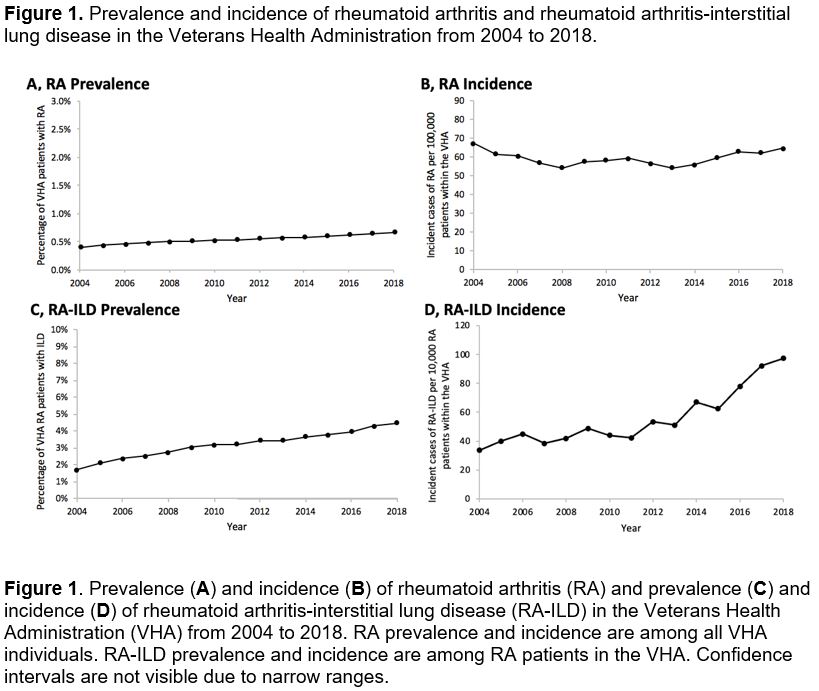 Figure 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-interstitial lung disease in the Veterans Health Administration from 2004 to 2018.
Figure 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-interstitial lung disease in the Veterans Health Administration from 2004 to 2018.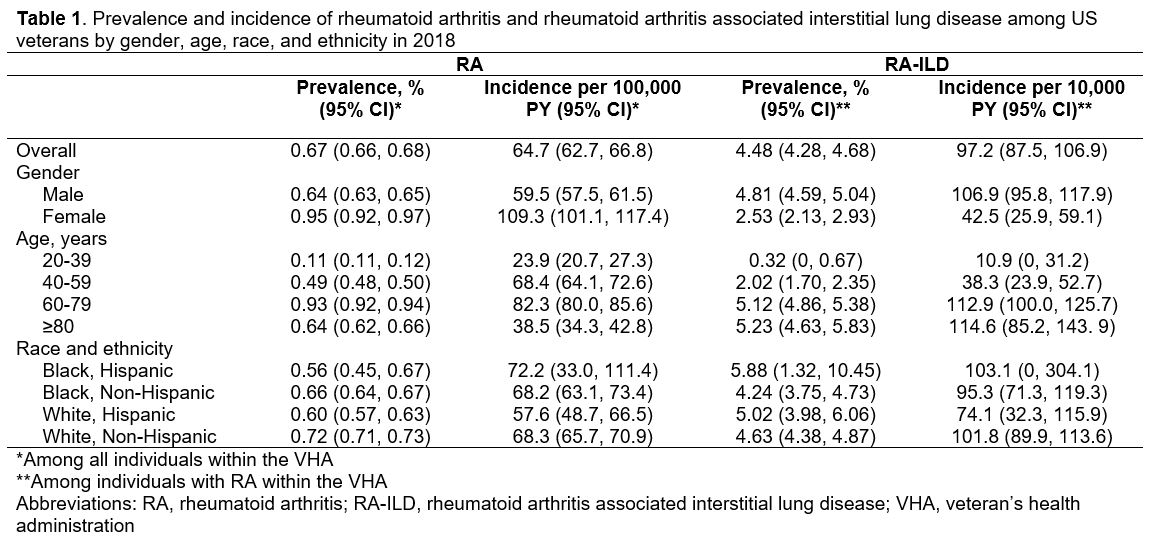 Table 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-associated interstitial lung disease among US veterans by gender, age, race, and ethnicity in 2018
Table 1. Prevalence and incidence of rheumatoid arthritis and rheumatoid arthritis-associated interstitial lung disease among US veterans by gender, age, race, and ethnicity in 2018Disclosures: B. Fletcher, None; P. Roul, None; Y. Yang, None; B. Sauer, None; J. Rojas, None; G. Cannon, None; J. Baker, Bristol Myers Squibb, Pfizer, CorEvitas LLC, Burns-White, LLC, RediTrex; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.

