Back
Abstract Session
Osteoarthritis (OA) and related disorders
Session: Abstracts: Osteoarthritis – Clinical (1639–1644)
1644: Effect of a Lifestyle Program Based on a Whole Food Plant-based Diet, Physical Activity, and Stress Management in Patients with Metabolic Syndrome-Associated Osteoarthritis: A Randomized Controlled Trial
Monday, November 14, 2022
10:15 AM – 10:25 AM Eastern Time
Location: Room 120
- WW
Wendy Walrabenstein, MA
Amsterdam UMC
Amsterdam, Netherlands
Presenting Author(s)
Wendy Walrabenstein1, Carlijn Wagenaar1, Marike van der Leeden2, Martijn Gerritsen1, Martin van der Esch1 and Dirkjan van Schaardenburg2, 1Reade Rheumatology Center, Amsterdam, Netherlands, 2Amsterdam UMC, Amsterdam, Netherlands
Background/Purpose: Metabolic syndrome with low grade inflammation is associated with chronic diseases including osteoarthritis (OA) (1). A combination of an intensive diet with exercise produced better results in people with osteoarthritis (OA) than either intervention alone (2). We further developed the concept of an integrated lifestyle intervention in people with metabolic syndrome-associated osteoarthritis (MSOA) by combining a whole food plant-based diet (WFPD) with physical activity and stress management and aimed to determine the effect of this program on pain, stiffness, and physical function in patients with MSOA.
Methods: In the "Plants for Joints" (PFJ) parallel-arm, randomized clinical trial, patients with MSOA were assigned to the PFJ group or the control group. Patients with metabolic syndrome (according to NCEP criteria) and OA in the knee and/or hip (according to clinical ACR criteria) were eligible for participation. The PFJ group followed a 16-week lifestyle program based on a WFPD, physical activity, and stress management in addition to usual care. The control group received usual care.
It was hypothesized that the lifestyle program would reduce pain and stiffness and improve physical function, based on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score (primary outcome). Secondary outcomes included anthropometric and metabolic markers. An intention-to-treat analysis with a linear mixed model, adjusted for baseline values was used to analyze the between-group differences of primary and secondary continuous outcomes.
Results: Of the 92 people screened, 66 were randomized and 64 completed the study (PFJ group: n = 32). Participants were 84% female, had a mean (SD) age of 63 (6) and a mean (SD) BMI of 33 (5) kg/m2. After 16 weeks the PFJ group had a mean 11-point lower (favorable) total WOMAC score (range 0-96) over time (95% CI 6 to 16; p = 0.0001) with significant improvements in all three components pain, stiffness, and physical function compared to the control group (Figure 1). Also, compared to the control group, the PFJ group lost more body weight, fat mass and waist circumference. HbA1c, fasting glucose and LDL improved in the PFJ versus control group, while HDL, triglycerides and blood pressure remained unchanged (Table 1).
Conclusion: The 16-week "Plants for Joints" lifestyle program substantially reduced pain and stiffness and improved physical function in people with metabolic syndrome associated osteoarthritis of hip and/or knee. In addition, following the lifestyle program resulted in improved anthropometric and metabolic outcomes in comparison with usual care.
Reference:
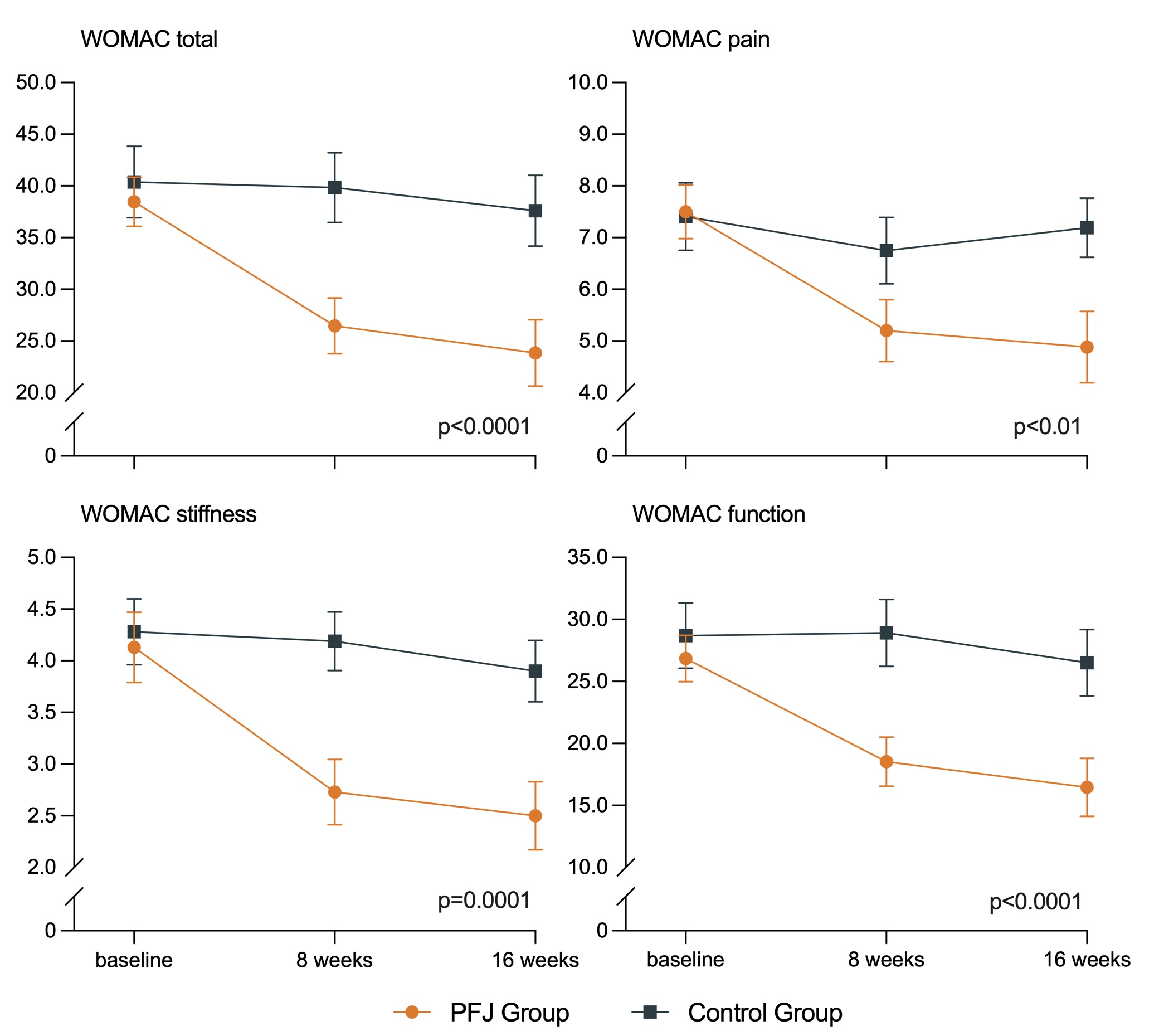 Figure 1. Change in Western Ontario and McMaster Universities Arthritis Index (WOMAC) total score (p = 0.0001) and WOMAC component scores for pain (p = 0.04), stiffness (p < 0.001) and function (p = 0.0001) for the Plants for Joints group (n = 32) when compared with the control group (n = 32). Graphs present mean ± standard error.
Figure 1. Change in Western Ontario and McMaster Universities Arthritis Index (WOMAC) total score (p = 0.0001) and WOMAC component scores for pain (p = 0.04), stiffness (p < 0.001) and function (p = 0.0001) for the Plants for Joints group (n = 32) when compared with the control group (n = 32). Graphs present mean ± standard error.
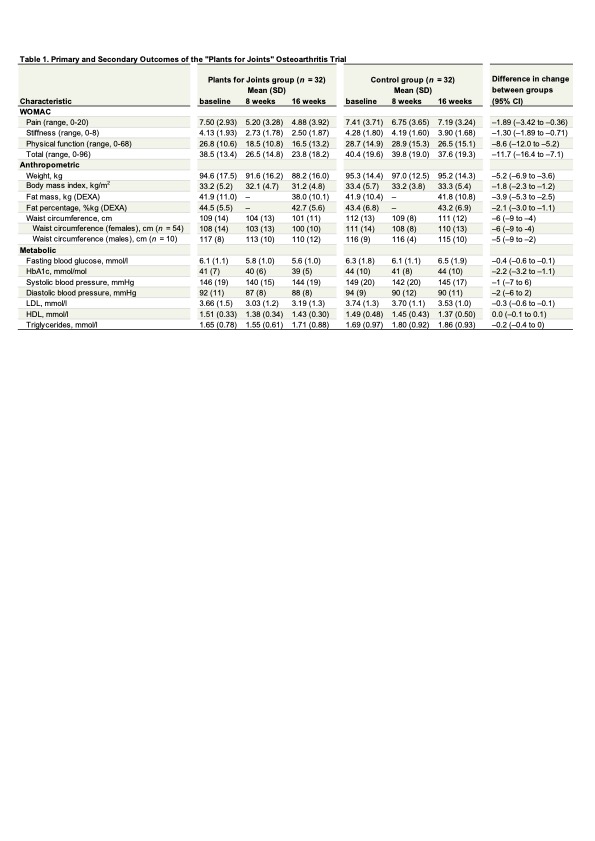 All values for the total group (n = 64), Western Ontario and McMaster Universities Arthritis Index (WOMAC), DEXA = Dual-energy X-ray absorptiometry, SD = standard deviation. Differences in change between group are based on a linear mixed model with random effect for subjects for between group analyses, adjusted for baseline values. Additional adjustment for covariates (sex, age and BMI) did not change outcomes.
All values for the total group (n = 64), Western Ontario and McMaster Universities Arthritis Index (WOMAC), DEXA = Dual-energy X-ray absorptiometry, SD = standard deviation. Differences in change between group are based on a linear mixed model with random effect for subjects for between group analyses, adjusted for baseline values. Additional adjustment for covariates (sex, age and BMI) did not change outcomes.
Disclosures: W. Walrabenstein, None; C. Wagenaar, None; M. van der Leeden, None; M. Gerritsen, None; M. van der Esch, None; D. van Schaardenburg, None.
Background/Purpose: Metabolic syndrome with low grade inflammation is associated with chronic diseases including osteoarthritis (OA) (1). A combination of an intensive diet with exercise produced better results in people with osteoarthritis (OA) than either intervention alone (2). We further developed the concept of an integrated lifestyle intervention in people with metabolic syndrome-associated osteoarthritis (MSOA) by combining a whole food plant-based diet (WFPD) with physical activity and stress management and aimed to determine the effect of this program on pain, stiffness, and physical function in patients with MSOA.
Methods: In the "Plants for Joints" (PFJ) parallel-arm, randomized clinical trial, patients with MSOA were assigned to the PFJ group or the control group. Patients with metabolic syndrome (according to NCEP criteria) and OA in the knee and/or hip (according to clinical ACR criteria) were eligible for participation. The PFJ group followed a 16-week lifestyle program based on a WFPD, physical activity, and stress management in addition to usual care. The control group received usual care.
It was hypothesized that the lifestyle program would reduce pain and stiffness and improve physical function, based on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score (primary outcome). Secondary outcomes included anthropometric and metabolic markers. An intention-to-treat analysis with a linear mixed model, adjusted for baseline values was used to analyze the between-group differences of primary and secondary continuous outcomes.
Results: Of the 92 people screened, 66 were randomized and 64 completed the study (PFJ group: n = 32). Participants were 84% female, had a mean (SD) age of 63 (6) and a mean (SD) BMI of 33 (5) kg/m2. After 16 weeks the PFJ group had a mean 11-point lower (favorable) total WOMAC score (range 0-96) over time (95% CI 6 to 16; p = 0.0001) with significant improvements in all three components pain, stiffness, and physical function compared to the control group (Figure 1). Also, compared to the control group, the PFJ group lost more body weight, fat mass and waist circumference. HbA1c, fasting glucose and LDL improved in the PFJ versus control group, while HDL, triglycerides and blood pressure remained unchanged (Table 1).
Conclusion: The 16-week "Plants for Joints" lifestyle program substantially reduced pain and stiffness and improved physical function in people with metabolic syndrome associated osteoarthritis of hip and/or knee. In addition, following the lifestyle program resulted in improved anthropometric and metabolic outcomes in comparison with usual care.
Reference:
1. Furman et al. 2019, Nat Med.
2. Messier et al. 2013, JAMA
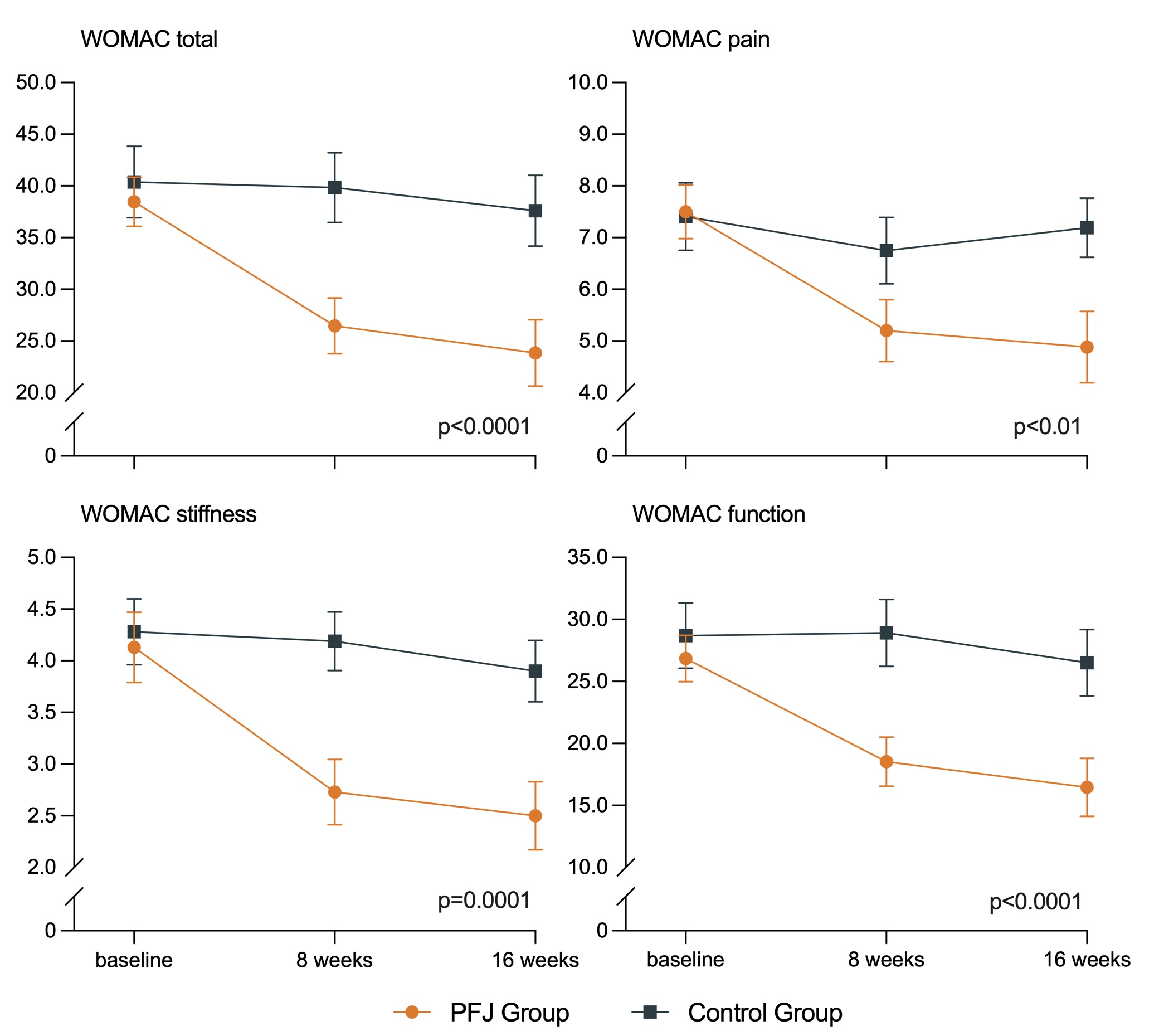 Figure 1. Change in Western Ontario and McMaster Universities Arthritis Index (WOMAC) total score (p = 0.0001) and WOMAC component scores for pain (p = 0.04), stiffness (p < 0.001) and function (p = 0.0001) for the Plants for Joints group (n = 32) when compared with the control group (n = 32). Graphs present mean ± standard error.
Figure 1. Change in Western Ontario and McMaster Universities Arthritis Index (WOMAC) total score (p = 0.0001) and WOMAC component scores for pain (p = 0.04), stiffness (p < 0.001) and function (p = 0.0001) for the Plants for Joints group (n = 32) when compared with the control group (n = 32). Graphs present mean ± standard error. 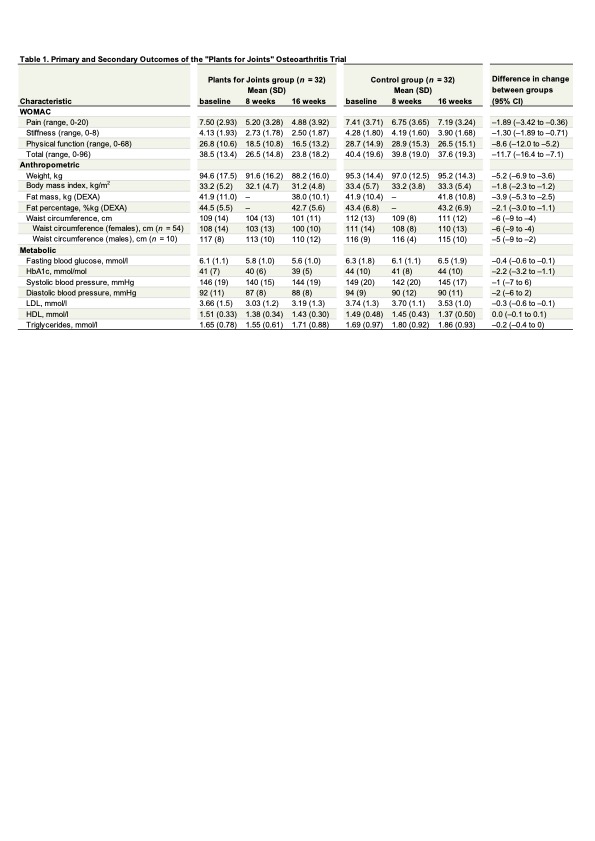 All values for the total group (n = 64), Western Ontario and McMaster Universities Arthritis Index (WOMAC), DEXA = Dual-energy X-ray absorptiometry, SD = standard deviation. Differences in change between group are based on a linear mixed model with random effect for subjects for between group analyses, adjusted for baseline values. Additional adjustment for covariates (sex, age and BMI) did not change outcomes.
All values for the total group (n = 64), Western Ontario and McMaster Universities Arthritis Index (WOMAC), DEXA = Dual-energy X-ray absorptiometry, SD = standard deviation. Differences in change between group are based on a linear mixed model with random effect for subjects for between group analyses, adjusted for baseline values. Additional adjustment for covariates (sex, age and BMI) did not change outcomes.Disclosures: W. Walrabenstein, None; C. Wagenaar, None; M. van der Leeden, None; M. Gerritsen, None; M. van der Esch, None; D. van Schaardenburg, None.

