Back
Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes II: Cardiovascular and Other Comorbidities (1646–1650)
1650: Systemic Immune Inflammation Index Predict All-Cause and Cardiovascular Mortality in Rheumatoid Arthritis
Monday, November 14, 2022
9:45 AM – 9:55 AM Eastern Time
Location: Terrace Ballroom IV
Jose Felix Restrepo, MD
University of Texas Health Science center at San Antonio
San Antonio, TX, United States
Presenting Author(s)
Jose felix Restrepo Suarez1, Inmaculada Del Rincon1, Carlos Lorenzo2 and Agustin Escalante3, 1University of Texas Health Science center at San Antonio, San Antonio, TX, 2University of Texas Health Sciences Center San Antonio, San antonio, TX, 3University of Texas Health Science Center at San Antonio, San Antonio, TX
Background/Purpose: The systemic immune inflammation index (SII) is an inflammation-based biomarker that is an influential prognostic factor in diseases with an inflammation-related etiology. This index is the product of the counts of neutrophils X platelets divided by lymphocytes (nxp/l). Rheumatoid arthritis (RA) is characterized by systemic inflammation affecting joints and other tissues and organs. This severe inflammation has been associated with premature all-cause and cardiovascular (CV) mortality. Therefore, we aimed to study the ability of SII to predict mortality in a cohort of Rheumatoid arthritis.
Methods: We studied 1211 RA patients. First, we examined demographic characteristics stratified by all-cause or cardiovascular mortality. Then, we included the following covariables in the analysis: age, sex, lipid profile, smoking status, glucose level, CBC, and SII. We next divided the SII into two quantiles after establishing a cut-point between positive and negative SII predictors in the logistic regression. Finally, we analyze the data through logistic regression to establish an association between SII and mortality.
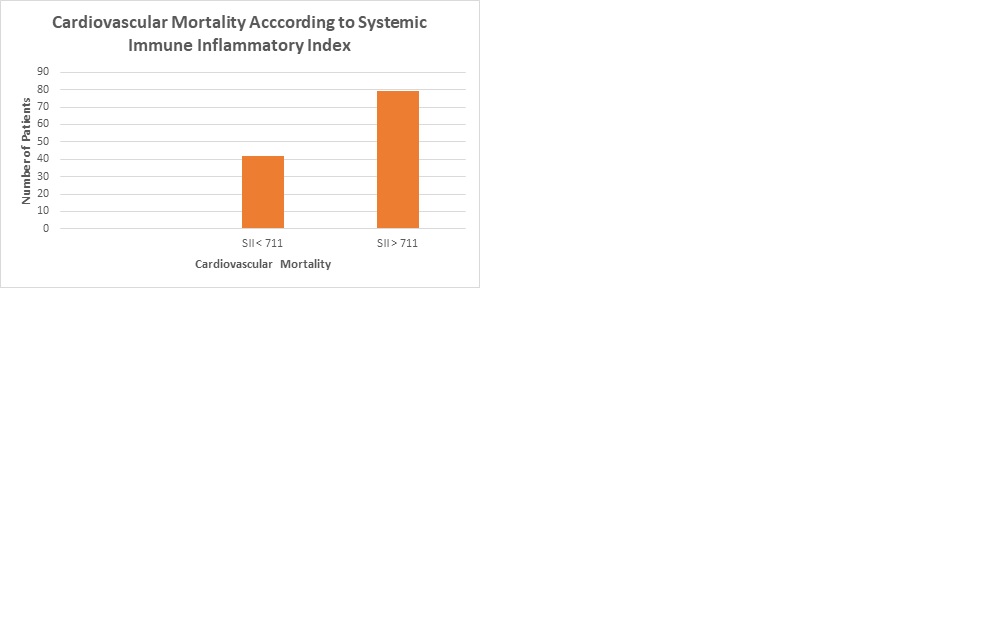
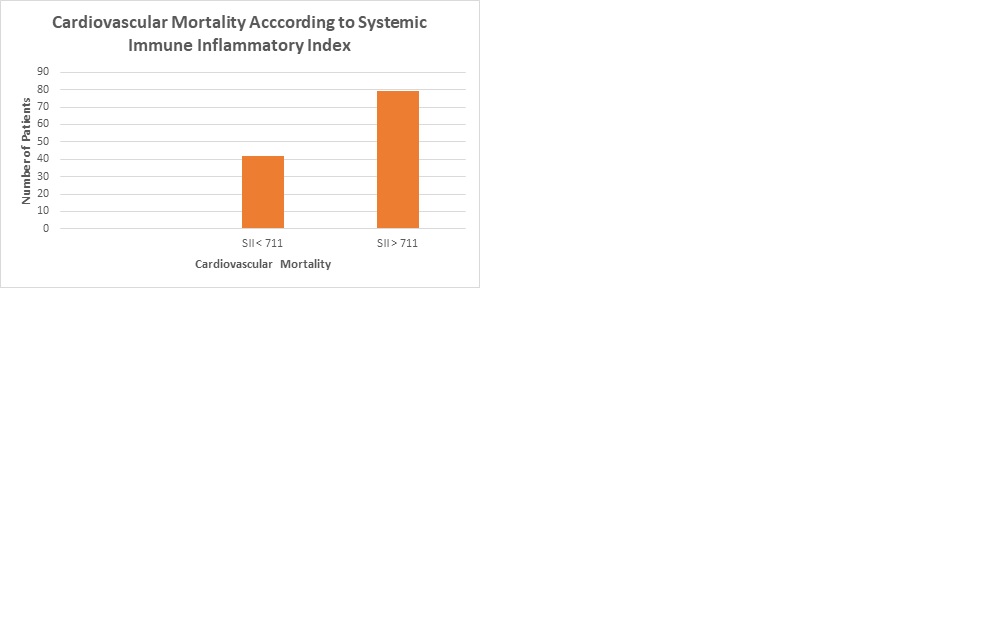
Results: We studied 1211 patients [906 (75%) women]. The mean follow-up time was 9.9 person-years with 278 deaths (2.7 per 100 person-years) for all-cause mortality. The mean follow-up time for CV mortality was 8745 person-years with 121 death (0.3 per 100 person-years). The cut-point for SII was 710.99. There were 180 all-cause deaths in the group with SII > 711 vs. 98 in the group with SII < 711. Similarly, there was 79 cardiovascular deaths vs. 42 in the same groups, respectively. The logistic regression analysis, crude and multivariable, showed that SII predicts all-cause (OR 2.64, 95% CI 1.81, 3.85 p < 0.0001) and CV-mortality (OR 3.03 955 CI 1.76, 5,21, p < 0001 ). (Figures)
Conclusion: SII is a biomarker derived from variables that are ubiquitous in clinical practice and that can be obtained with a hand-held calculator. Our findings suggest that it is an efficient survival predictor, accounting for both all-cause and CV mortality in patients with RA. Further research to examine the performance of the SII as a predictor of other important RA outcomes would be of considerable interest.
.jpg)
Disclosures: J. Restrepo Suarez, None; I. Del Rincon, None; C. Lorenzo, None; A. Escalante, None.
Background/Purpose: The systemic immune inflammation index (SII) is an inflammation-based biomarker that is an influential prognostic factor in diseases with an inflammation-related etiology. This index is the product of the counts of neutrophils X platelets divided by lymphocytes (nxp/l). Rheumatoid arthritis (RA) is characterized by systemic inflammation affecting joints and other tissues and organs. This severe inflammation has been associated with premature all-cause and cardiovascular (CV) mortality. Therefore, we aimed to study the ability of SII to predict mortality in a cohort of Rheumatoid arthritis.
Methods: We studied 1211 RA patients. First, we examined demographic characteristics stratified by all-cause or cardiovascular mortality. Then, we included the following covariables in the analysis: age, sex, lipid profile, smoking status, glucose level, CBC, and SII. We next divided the SII into two quantiles after establishing a cut-point between positive and negative SII predictors in the logistic regression. Finally, we analyze the data through logistic regression to establish an association between SII and mortality.
Results: We studied 1211 patients [906 (75%) women]. The mean follow-up time was 9.9 person-years with 278 deaths (2.7 per 100 person-years) for all-cause mortality. The mean follow-up time for CV mortality was 8745 person-years with 121 death (0.3 per 100 person-years). The cut-point for SII was 710.99. There were 180 all-cause deaths in the group with SII > 711 vs. 98 in the group with SII < 711. Similarly, there was 79 cardiovascular deaths vs. 42 in the same groups, respectively. The logistic regression analysis, crude and multivariable, showed that SII predicts all-cause (OR 2.64, 95% CI 1.81, 3.85 p < 0.0001) and CV-mortality (OR 3.03 955 CI 1.76, 5,21, p < 0001 ). (Figures)
Conclusion: SII is a biomarker derived from variables that are ubiquitous in clinical practice and that can be obtained with a hand-held calculator. Our findings suggest that it is an efficient survival predictor, accounting for both all-cause and CV mortality in patients with RA. Further research to examine the performance of the SII as a predictor of other important RA outcomes would be of considerable interest.
.jpg)
Disclosures: J. Restrepo Suarez, None; I. Del Rincon, None; C. Lorenzo, None; A. Escalante, None.

