Back
Abstract Session
Reproductive health
Session: Abstracts: Reproductive Issues in Rheumatic Disorders (1671–1674)
1673: Preconceptional NSAID Treatment Exposure Is Associated with a Significantly Longer Time-to-conception in Women with Spondyloarthritis: Analysis of the Prospective GR2 Cohort
Monday, November 14, 2022
11:00 AM – 11:10 AM Eastern Time
Location: Room 119
- SH
SABRINA HAMROUN, MMed
Rheumatology Department, University Hospital of Cochin, Paris
Paris, France
Presenting Author(s)
SABRINA HAMROUN1, Marion Couderc2, Rene-Marc Flipo3, Jérémie SELLAM4, Christophe Richez5, Emmanuelle Dernis6, Aline Frazier-Mironer7, Laure Gossec8, elisabeth gervais9, Hubert Marotte10, Laetitia Dunogeant11, Cédric Lukas12, Alban DEROUX13, Nathalie Costedoat-Chalumeau14 and Anna Molto15, 1Rheumatology Department, University Hospital of Cochin, Paris, Paris, France, 2University Hospital, Clermont-Ferrand, France, 3CHU Lille, Boulogne-Billancourt, France, 4Sorbonne Universite, AP-HP, Saint-Antoine hospital, Paris, France, 5Université de Bordeaux, Bordeaux, France, 6LE MANS general hospital, LE MANS, France, 7APHP Hôpital Lariboisire, Paris, France, 8Sorbonne Université, Paris, France, 9chu poitiers, Poitiers, France, 10INSERM 1059, Saint-Etienne, France, 11Hospital of Aix en Provence, Marseille, France, 12University Hospital Centre Montpellier, University of Montpellier, Montpellier, France, 13CHU Grenoble, Grenoble, France, 14Inserm DR Paris 5, Paris, France, 15Rheumatology Department, Cochin Hospital, APHP, Paris, France
Background/Purpose: Spondyloarthritis (SpA) is one of the most common chronic inflammatory diseases and regularly affects women of childbearing age. However, there is limited knowledge about the impact of the disease and its treatment on fertility. The aim of the study was to determine factors associated with time-to-conception in women with SpA.
Methods: We performed an analysis of SpA patients (diagnosis according to the rheumatologist) included in the national multicenter cohort GR2 from 2015 to June 2021. Patients could be included either with a pregnancy wish (i.e., preconceptional period) or because of a clinical pregnancy (< 12 weeks of gestation): for this analysis, only patients included preconceptionally were included. The main endpoint was time-to-conception, and the secondary endpoints were the number of subfertile patients (i.e., time-to-conception >12 months or non-achievement of pregnancy), as well as the number exposed to csDMARDs and biologics in the preconception period. We performed survival analyses, using a Cox model including a random effect for the center to account for heterogeneity of practices among participating centers. We used a multiple imputation to address missing data among the explanatory variables. Results are presented as a hazard ratio (HR) with confidence interval (CI) to assess associations between the factors studied and time-to-conception.
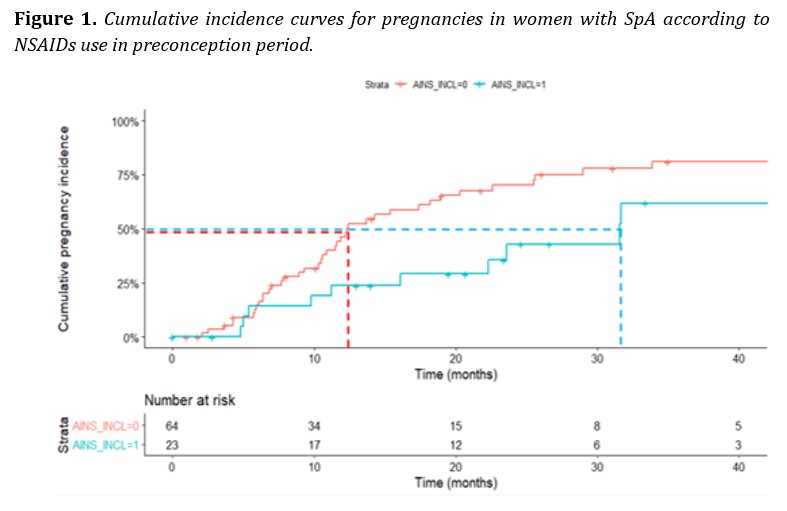
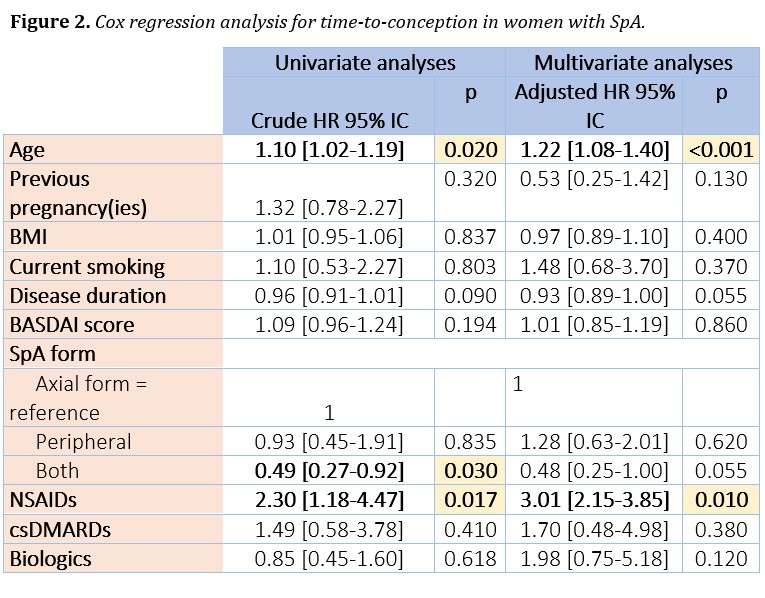
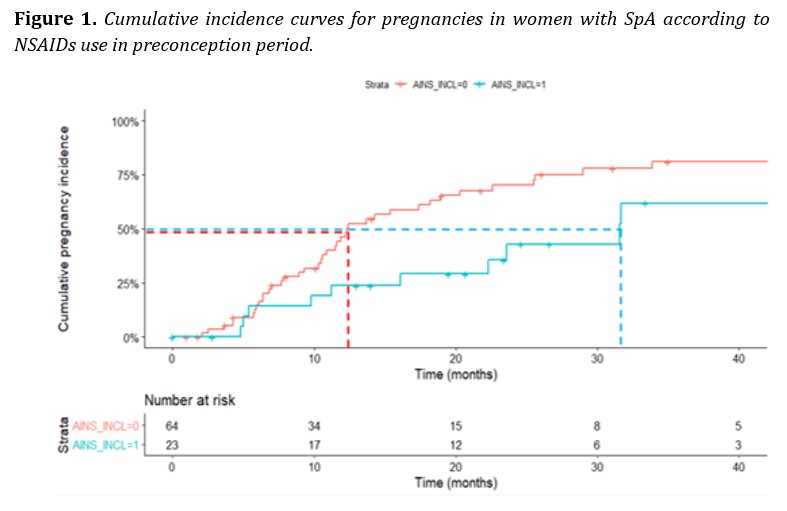
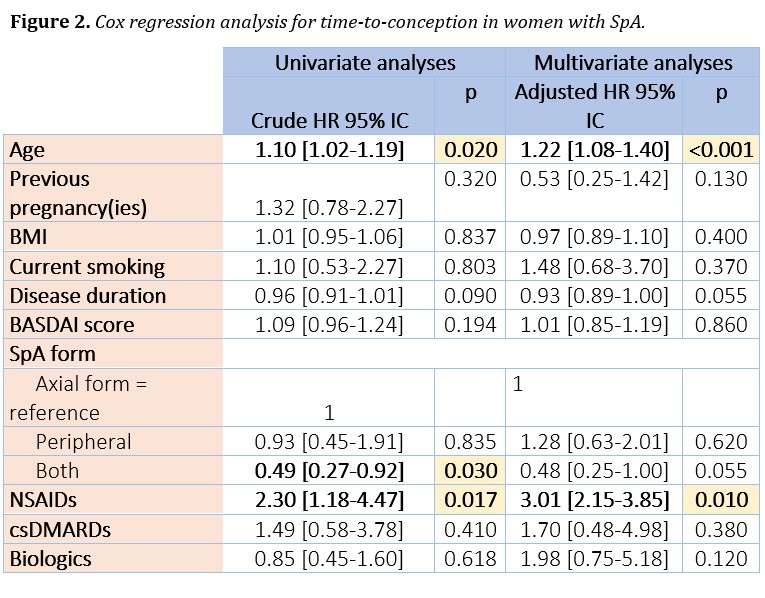
Results: Among the 207 patients with SpA included in the GR2 cohort, 88 were selected for analysis of time-to-conception (i.e., include preconceptionally). Of these, 56 (63.6%) had a clinical pregnancy during follow-up. Subfertility was observed in 40 (45.4%) women and the median time-to-conception was 16.1 months. The mean preconceptional BASDAI score was 2.9 (+/- 2.1). Patients were treated with NSAIDs, corticosteroids, csDMARDs and biotherapy in 23 (26.1%), 8 (9.1%), 12 (13.6%), and 61 (69.3%) cases, respectively. The multivariate model adjusted for age, BMI, nulligestity, BASDAI, disease duration, smoking, form of spondyloarthritis (axial, peripheral, or both), and exposure to NSAIDs, csDMARDs, and biotherapy in the preconception period found an association between longer time-to-conception and age (HR 1. 22 95% CI [1.08-1.40] p < 0.001), as well as the use of NSAIDs during preconception (HR 3.01 95% CI [2.15-3.85] p = 0.01).
Conclusion: This study provides original results on fertility in women with SpA. The factors associated with a longer time-to-conception were age and the NSAIDs use during the preconception period, which argues for their cautious use in case of pregnancy wish in patients needing continuous NSAID intake for the management of their disease.
Disclosures: S. HAMROUN, None; M. Couderc, None; R. Flipo, Merck/MSD, Novartis, Janssen; J. SELLAM, None; C. Richez, AbbVie/Abbott, Amgen, AstraZeneca, Biogen, Bristol-Myers Squibb(BMS), Galapados, GlaxoSmithKlein(GSK), Eli Lilly, Novartis, Pfizer; E. Dernis, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Janssen, Nordic Pharma France, Novartis, UCB; A. Frazier-Mironer, None; L. Gossec, Amgen, Lilly, Pfizer, Sandoz, UCB Pharma, AbbVie, Bristol Myers Squibb, Gilead, Janssen, Novartis, Samsung Bioepis, Sanofi-Aventis, Galapagos, GlaxoSmithKlein (GSK), Celltrion, MSD; e. gervais, None; H. Marotte, AbbVie/Abbott, Amgen, Biogen, Bristol-Myers Squibb(BMS), CellTrion HealthCare, Fresenius Kabi, HealthCare, Janssen, Eli Lilly, Nordic Pharma, Novartis, Medac, Pfizer, Merck/MSD, Galapagos, UCB; L. Dunogeant, None; C. Lukas, None; A. DEROUX, None; N. Costedoat-Chalumeau, UCB, Roche; A. Molto, None.
Background/Purpose: Spondyloarthritis (SpA) is one of the most common chronic inflammatory diseases and regularly affects women of childbearing age. However, there is limited knowledge about the impact of the disease and its treatment on fertility. The aim of the study was to determine factors associated with time-to-conception in women with SpA.
Methods: We performed an analysis of SpA patients (diagnosis according to the rheumatologist) included in the national multicenter cohort GR2 from 2015 to June 2021. Patients could be included either with a pregnancy wish (i.e., preconceptional period) or because of a clinical pregnancy (< 12 weeks of gestation): for this analysis, only patients included preconceptionally were included. The main endpoint was time-to-conception, and the secondary endpoints were the number of subfertile patients (i.e., time-to-conception >12 months or non-achievement of pregnancy), as well as the number exposed to csDMARDs and biologics in the preconception period. We performed survival analyses, using a Cox model including a random effect for the center to account for heterogeneity of practices among participating centers. We used a multiple imputation to address missing data among the explanatory variables. Results are presented as a hazard ratio (HR) with confidence interval (CI) to assess associations between the factors studied and time-to-conception.
Results: Among the 207 patients with SpA included in the GR2 cohort, 88 were selected for analysis of time-to-conception (i.e., include preconceptionally). Of these, 56 (63.6%) had a clinical pregnancy during follow-up. Subfertility was observed in 40 (45.4%) women and the median time-to-conception was 16.1 months. The mean preconceptional BASDAI score was 2.9 (+/- 2.1). Patients were treated with NSAIDs, corticosteroids, csDMARDs and biotherapy in 23 (26.1%), 8 (9.1%), 12 (13.6%), and 61 (69.3%) cases, respectively. The multivariate model adjusted for age, BMI, nulligestity, BASDAI, disease duration, smoking, form of spondyloarthritis (axial, peripheral, or both), and exposure to NSAIDs, csDMARDs, and biotherapy in the preconception period found an association between longer time-to-conception and age (HR 1. 22 95% CI [1.08-1.40] p < 0.001), as well as the use of NSAIDs during preconception (HR 3.01 95% CI [2.15-3.85] p = 0.01).
Conclusion: This study provides original results on fertility in women with SpA. The factors associated with a longer time-to-conception were age and the NSAIDs use during the preconception period, which argues for their cautious use in case of pregnancy wish in patients needing continuous NSAID intake for the management of their disease.
Disclosures: S. HAMROUN, None; M. Couderc, None; R. Flipo, Merck/MSD, Novartis, Janssen; J. SELLAM, None; C. Richez, AbbVie/Abbott, Amgen, AstraZeneca, Biogen, Bristol-Myers Squibb(BMS), Galapados, GlaxoSmithKlein(GSK), Eli Lilly, Novartis, Pfizer; E. Dernis, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Janssen, Nordic Pharma France, Novartis, UCB; A. Frazier-Mironer, None; L. Gossec, Amgen, Lilly, Pfizer, Sandoz, UCB Pharma, AbbVie, Bristol Myers Squibb, Gilead, Janssen, Novartis, Samsung Bioepis, Sanofi-Aventis, Galapagos, GlaxoSmithKlein (GSK), Celltrion, MSD; e. gervais, None; H. Marotte, AbbVie/Abbott, Amgen, Biogen, Bristol-Myers Squibb(BMS), CellTrion HealthCare, Fresenius Kabi, HealthCare, Janssen, Eli Lilly, Nordic Pharma, Novartis, Medac, Pfizer, Merck/MSD, Galapagos, UCB; L. Dunogeant, None; C. Lukas, None; A. DEROUX, None; N. Costedoat-Chalumeau, UCB, Roche; A. Molto, None.

