Back
Plenary Session
Session: Plenary III
1675: Effectiveness of Intensive Diet and Exercise on Knee Pain Among Communities with Knee Osteoarthritis, Overweight, and Obesity: The WE-CAN Pragmatic Randomized Clinical Trial
Monday, November 14, 2022
11:30 AM – 11:40 AM Eastern Time
Location: Exhibit Hall A
- SM
Stephen Messier, PhD
Wake Forest University
Winston-Salem, NC, United States
Presenting Author(s)
Stephen Messier1, Daniel Beavers2, Kate Queen3, Shannon Mihalko1, Gary Miller1, Elena Losina4, Jeffrey Katz4, Richard Loeser5, Paul DeVita6, David Hunter7, Jovita Newman1, Sara Quandt8, Mary Lyles2, Joanne Jordan9 and Leigh Callahan10, 1Wake Forest University, Winston-Salem, NC, 2Wake Forest University School of Medicine, Winston-Salem, NC, 3Haywood Regional Medical Center, Waynesville, NC, 4Brigham and Women's Hospital, Boston, MA, 5University of North Carolina, Chapel Hill, NC, 6East Carolina University, Greenville, NC, 7University of Sydney, Sydney, Australia, 8Wake Forest School of Medicine, Winston-Salem, NC, 9University of North Carolina School of Medicine, Chapel Hill, NC, 10University of North Carolina Thurston Arthritis Research Center, Chapel Hill, NC
Background/Purpose: Many health systems that treat people with knee osteoarthritis (OA) have no infrastructure in place to implement weight loss and exercise treatments. The policy relevant and clinically important question is whether the success of weight loss and exercise programs documented in academic, center-based trials can be replicated in community settings.
Methods: We conducted a pragmatic, assessor-blinded, randomized controlled trial in community-dwelling, men and women aged ≥ 50 years with knee OA and overweight and obesity (BMI≥27 kg/m2). Participants were randomly assigned to either an 18-month diet and exercise (D+E) intervention or an attention control (C). The primary endpoint was the between group difference in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain (0 best–20 worst) at 18-months tested using a repeated measures mixed linear model with adjustments for covariates (P≤.05). Secondary endpoints include WOMAC function (0 best–68 worst), 6 minute walk distance, and SF-36 health-related quality of life.
Results: Among the 823 randomized participants (mean age, 64.6 years; 637(77%) women), 658(80%) completed the trial.
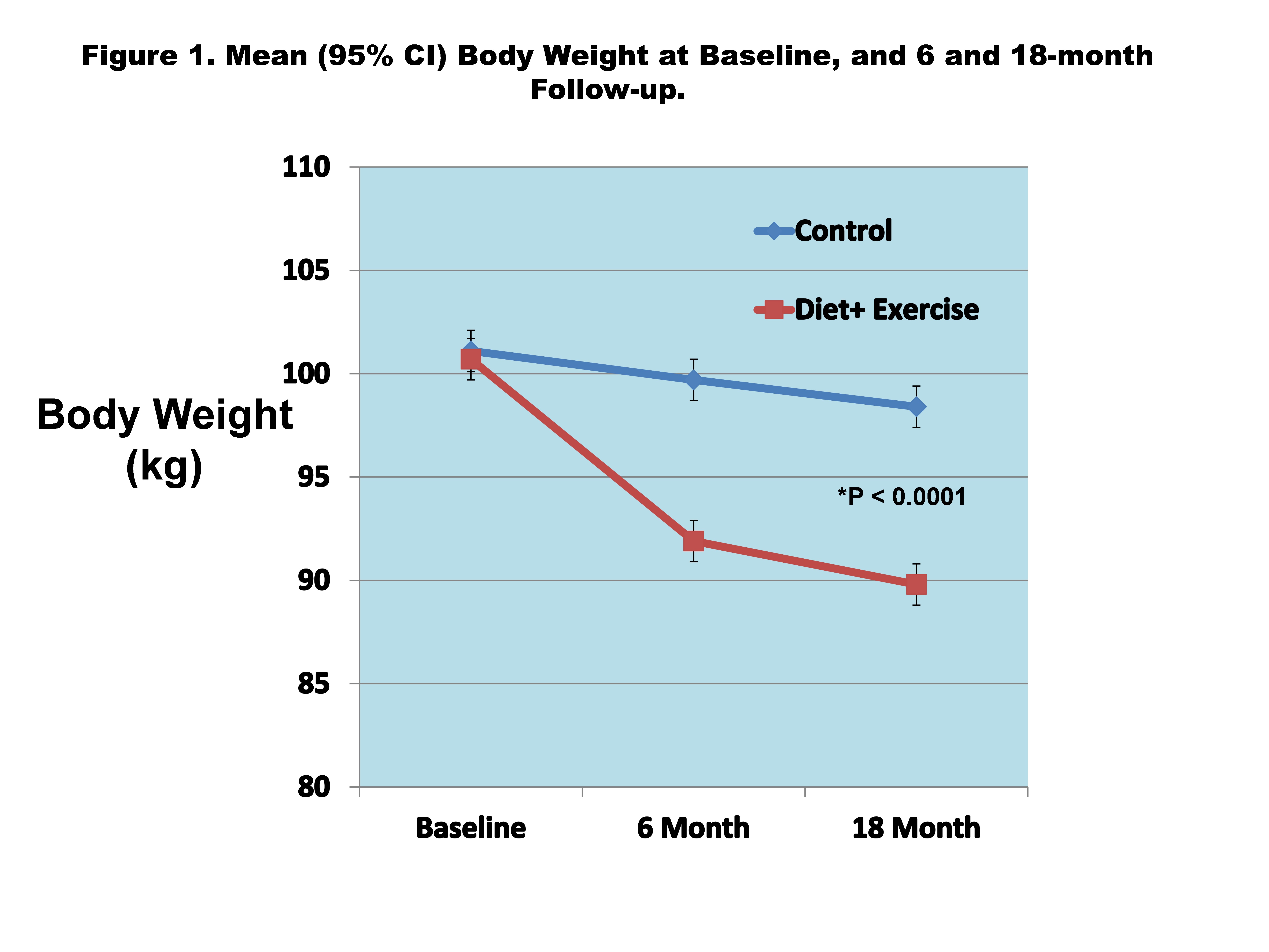
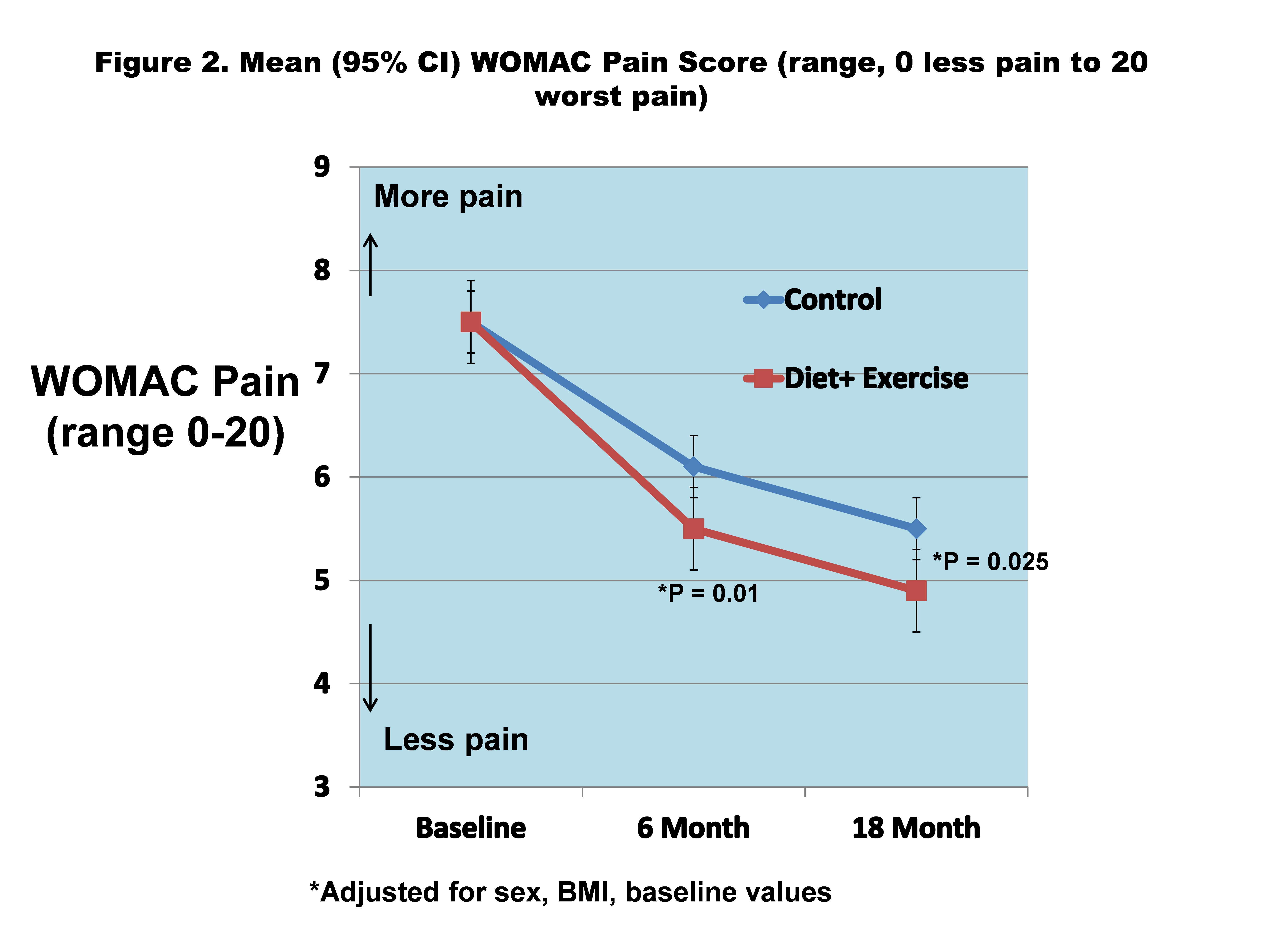
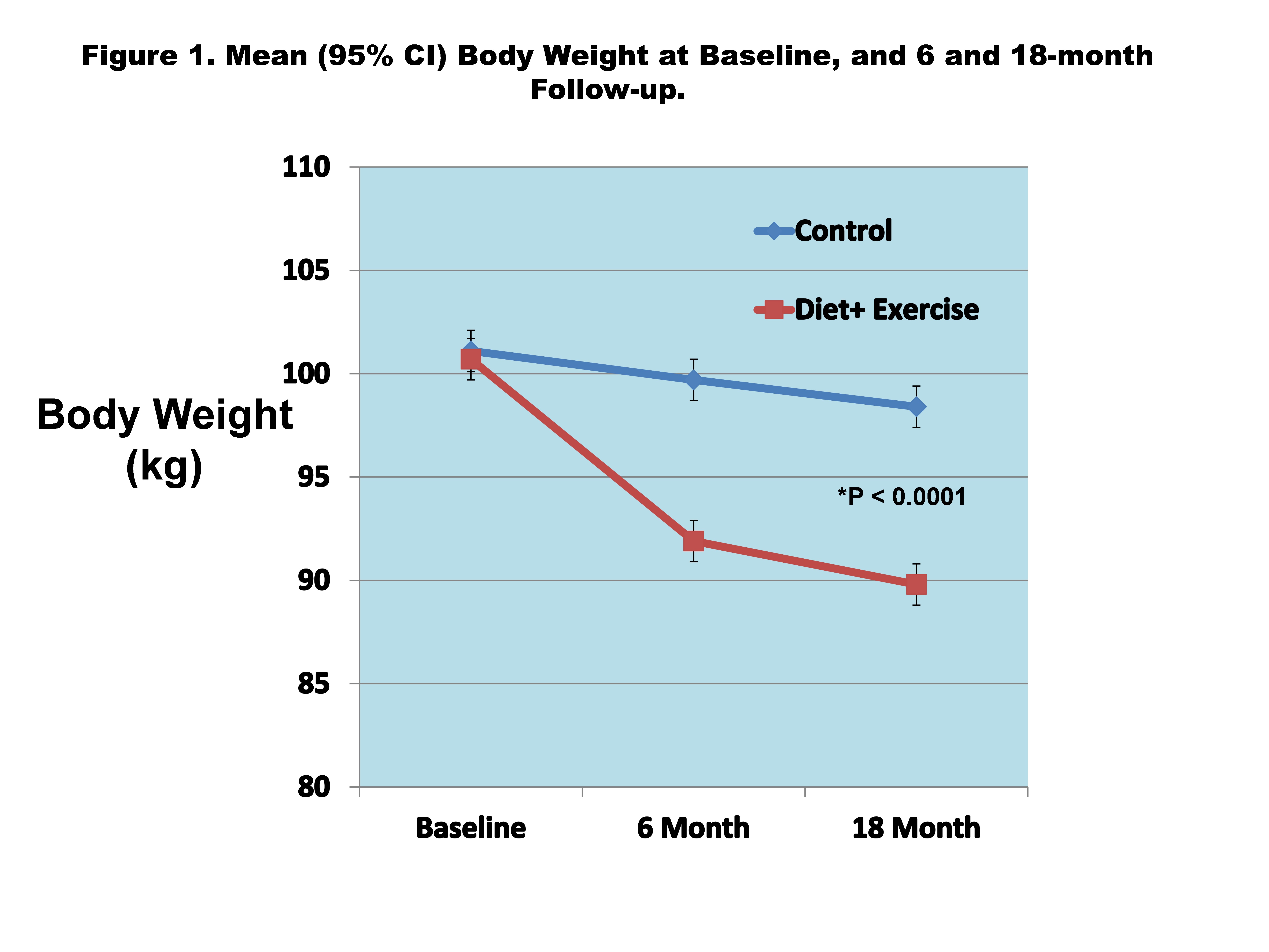
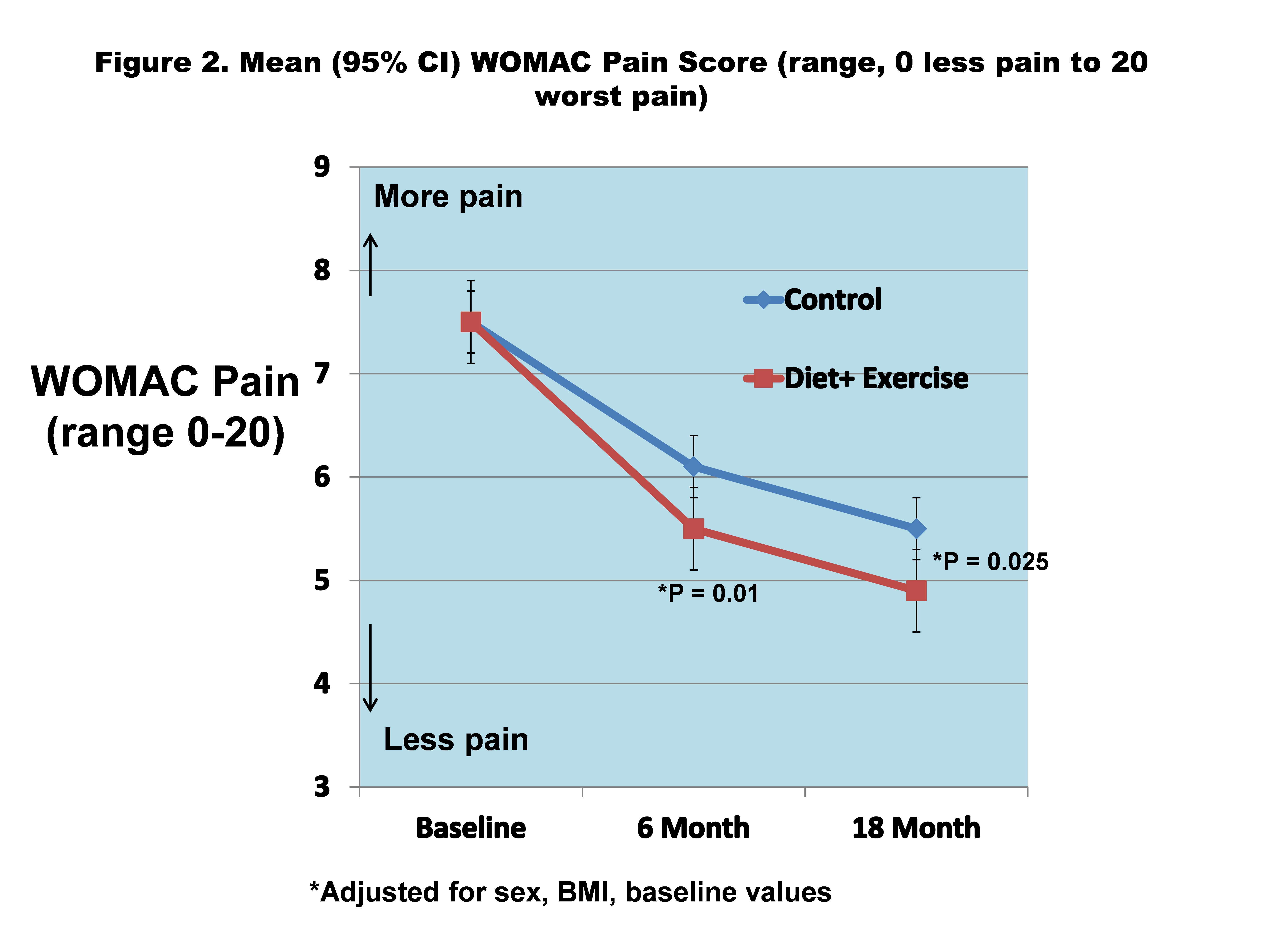
The difference in mean 18-month body weight between D+E and C was 10.9 kg(10.8%) vs 2.7 kg(2.7%), difference, 8.6; 95%CI, 5.4 to 11.9, P< .0001 (Figure 1). Mean 18-month WOMAC pain was significantly less for D+E vs C (4.9 vs 5.5; adjusted difference, -0.6; 95%CI, -1.0 to -0.1; P=.025) (Figure 2). D+E also had significantly improved WOMAC function (16.4 vs 19.7; adjusted difference, -3.3; 95%CI, -4.9 to -1.7; P< .0001), greater 6-minute walk distance (419 m vs 376 m; adjusted difference, 43; 95%CI, 31 to 55; P< .0001), and greater SF-36 physical health related quality of life compared to the C group (41.3 vs 37.5, adjusted difference, 3.8; 95% CI, 2.5 to 5.2, P< .0001).
Conclusion: Among participants with knee OA, overweight, and obesity, 18-months of diet and exercise delivered in community settings significantly reduced WOMAC knee pain compared to an attention control group. This community-based trial, which had few exclusion criteria due to its pragmatic design, resulted in reductions in weight and knee pain that were similar to previous academic, center-based efficacy trials of knee OA and weight loss. This study provides a blueprint for the implementation of a successful treatment for a pervasive public health problem in clinical and community settings.
Disclosures: S. Messier, None; D. Beavers, None; K. Queen, None; S. Mihalko, None; G. Miller, None; E. Losina, None; J. Katz, None; R. Loeser, None; P. DeVita, None; D. Hunter, Pfizer, Eli Lilly, Merck/MSD, TLCBio, Kolon Tissuegene, Novartis; J. Newman, None; S. Quandt, None; M. Lyles, None; J. Jordan, None; L. Callahan, None.
Background/Purpose: Many health systems that treat people with knee osteoarthritis (OA) have no infrastructure in place to implement weight loss and exercise treatments. The policy relevant and clinically important question is whether the success of weight loss and exercise programs documented in academic, center-based trials can be replicated in community settings.
Methods: We conducted a pragmatic, assessor-blinded, randomized controlled trial in community-dwelling, men and women aged ≥ 50 years with knee OA and overweight and obesity (BMI≥27 kg/m2). Participants were randomly assigned to either an 18-month diet and exercise (D+E) intervention or an attention control (C). The primary endpoint was the between group difference in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee pain (0 best–20 worst) at 18-months tested using a repeated measures mixed linear model with adjustments for covariates (P≤.05). Secondary endpoints include WOMAC function (0 best–68 worst), 6 minute walk distance, and SF-36 health-related quality of life.
Results: Among the 823 randomized participants (mean age, 64.6 years; 637(77%) women), 658(80%) completed the trial.
The difference in mean 18-month body weight between D+E and C was 10.9 kg(10.8%) vs 2.7 kg(2.7%), difference, 8.6; 95%CI, 5.4 to 11.9, P< .0001 (Figure 1). Mean 18-month WOMAC pain was significantly less for D+E vs C (4.9 vs 5.5; adjusted difference, -0.6; 95%CI, -1.0 to -0.1; P=.025) (Figure 2). D+E also had significantly improved WOMAC function (16.4 vs 19.7; adjusted difference, -3.3; 95%CI, -4.9 to -1.7; P< .0001), greater 6-minute walk distance (419 m vs 376 m; adjusted difference, 43; 95%CI, 31 to 55; P< .0001), and greater SF-36 physical health related quality of life compared to the C group (41.3 vs 37.5, adjusted difference, 3.8; 95% CI, 2.5 to 5.2, P< .0001).
Conclusion: Among participants with knee OA, overweight, and obesity, 18-months of diet and exercise delivered in community settings significantly reduced WOMAC knee pain compared to an attention control group. This community-based trial, which had few exclusion criteria due to its pragmatic design, resulted in reductions in weight and knee pain that were similar to previous academic, center-based efficacy trials of knee OA and weight loss. This study provides a blueprint for the implementation of a successful treatment for a pervasive public health problem in clinical and community settings.
Disclosures: S. Messier, None; D. Beavers, None; K. Queen, None; S. Mihalko, None; G. Miller, None; E. Losina, None; J. Katz, None; R. Loeser, None; P. DeVita, None; D. Hunter, Pfizer, Eli Lilly, Merck/MSD, TLCBio, Kolon Tissuegene, Novartis; J. Newman, None; S. Quandt, None; M. Lyles, None; J. Jordan, None; L. Callahan, None.

