Back
Poster Session D
Crystal arthropathies
Session: (1787–1829) Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
1828: Urate-lowering Therapy Reduces Non-Episodic Foot Pain in Patients Who Fail to Meet ACR/EULAR 2015 Gout Classification Criteria: An Effect Predicted by Ultrasound
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- RF
Rachael Flood, MD
Tallaght University Hospital
DUBLIN, Dublin, Ireland
Abstract Poster Presenter(s)
Rachael Flood1, Colm Kirby1, yousef Alammari2, David Kane1 and Ronan Mullan1, 1Tallaght University Hospital, Dublin, Ireland, 2Imam Mohammad Ibn Saud Islamic University, RIYADH, Ar Riyad, Saudi Arabia
Background/Purpose: Emerging evidence that joints of asymptomatic hyperuricaemic individuals contain monosodium urate (MSU) deposits and that alternative presentations of foot pain occur in hyperuricaemia suggests that preclinical phases may occur prior to a first episodic gout attack.
This case–control study evaluates urate deposition in hyperuricaemic individuals not fulfilling the ACR/EULAR 2015 gout classification criteria, as well as a potential therapeutic role for urate lowering therapy (ULT).
Methods: Following consent, hyperuricaemic individuals with persistent, non-episodic foot pain (N=68) not fulfilling ACR/EULAR 2015 gout classification criteria, were compared with asymptomatic hyperuricaemic controls (N=28). Ultrasound (US) of bilateral first metatarsophalangeal (MTP) joints and features of MSU deposition including double contour (DC) sign, tophus and erosions were recorded. Cases were treated with ULT daily for 6 months. Serum urate, 24-hour and 7-day visual analogue score (VAS) 0–100 mm pain scales the Manchester Foot Pain and Disability Index (MFPDI) and MTP US were recorded before treatment and after 3 and 6 months.
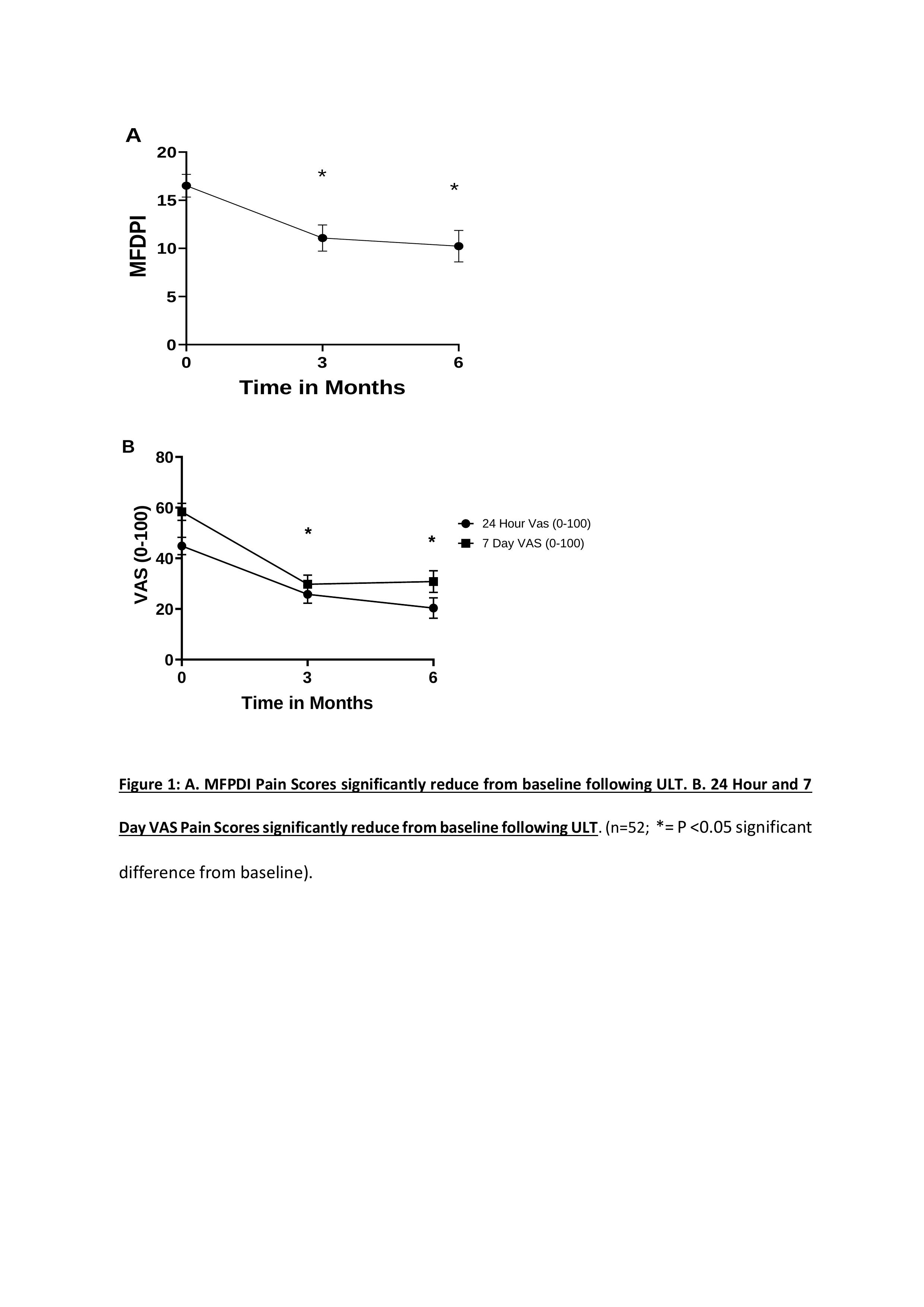
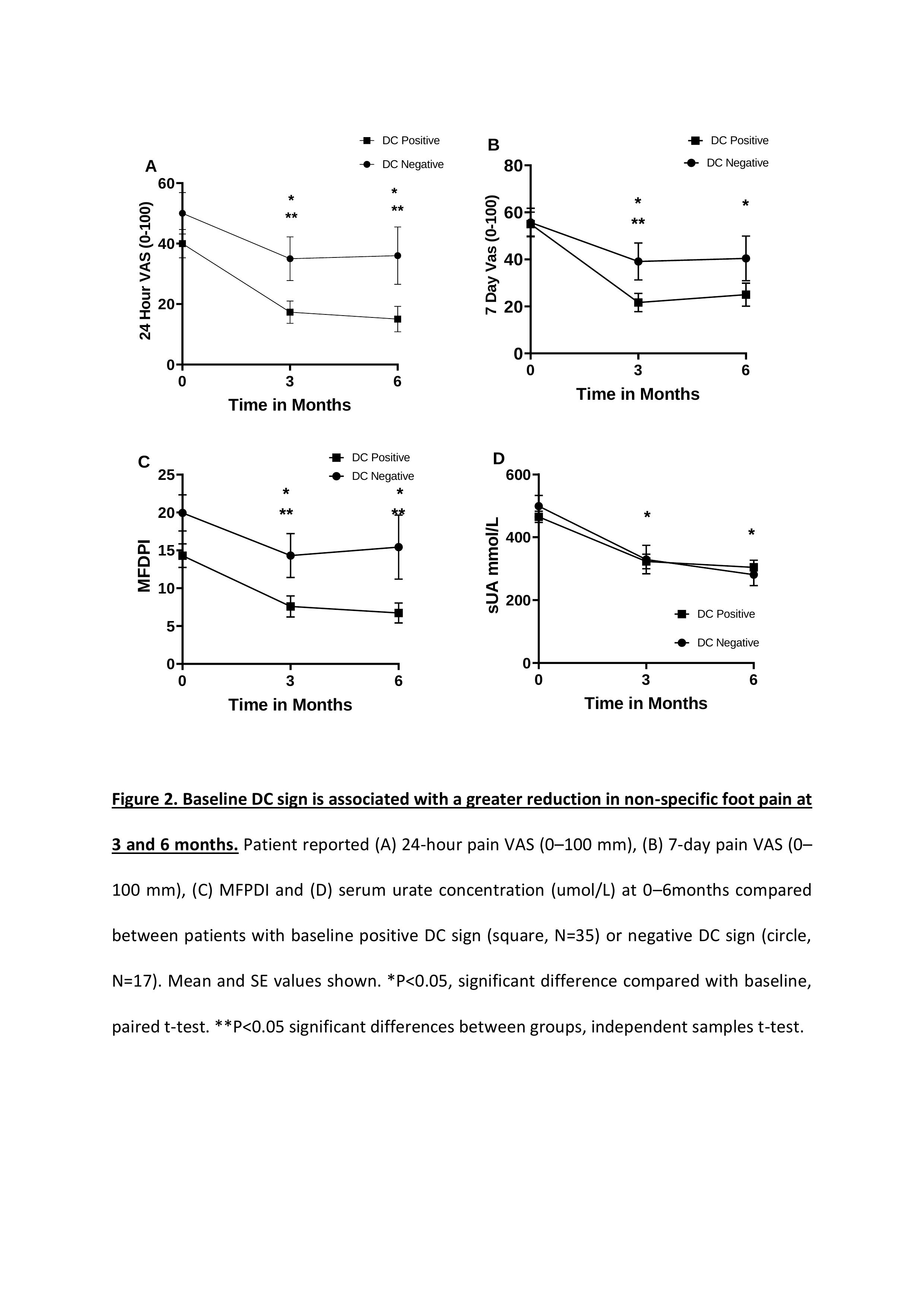
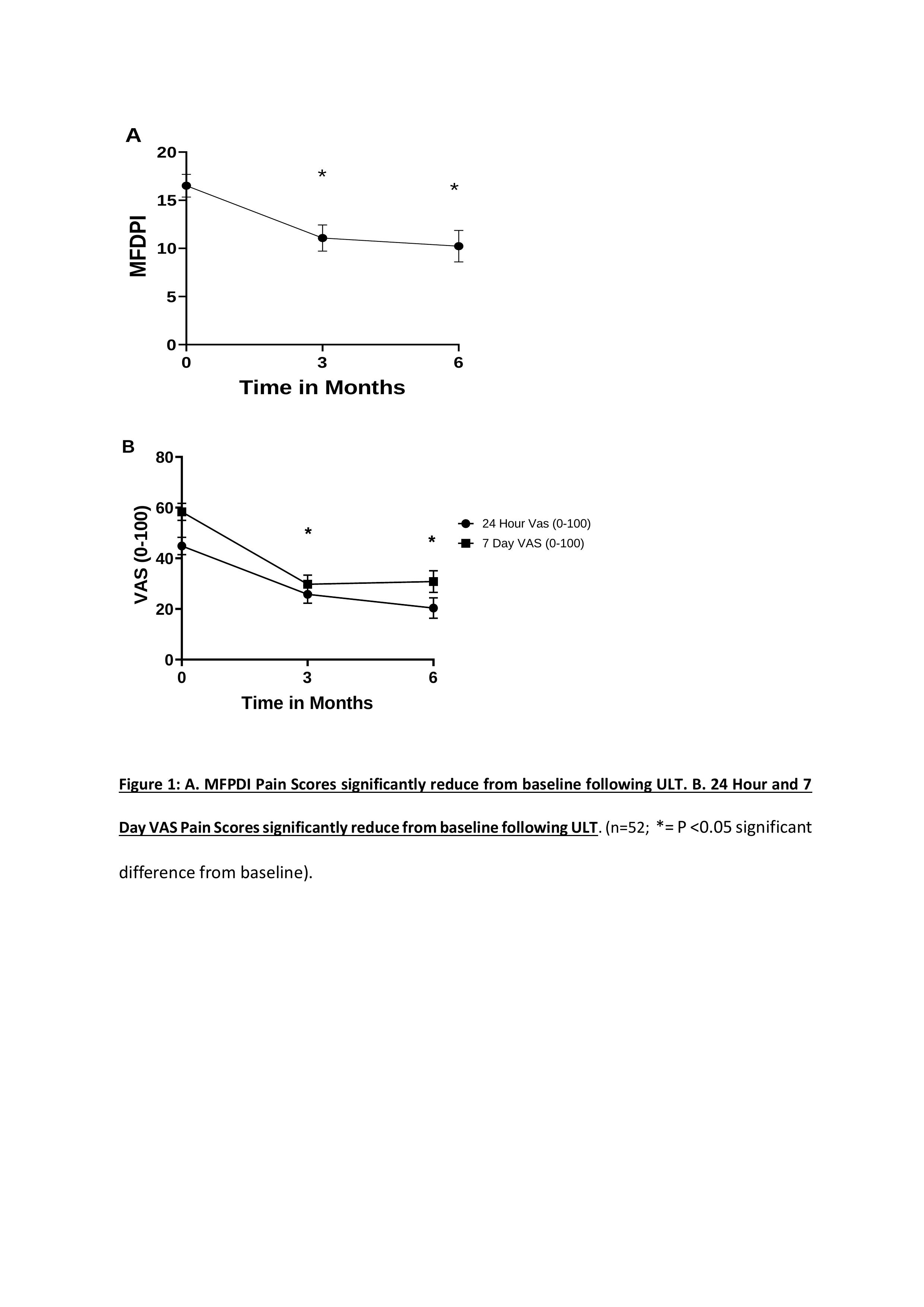
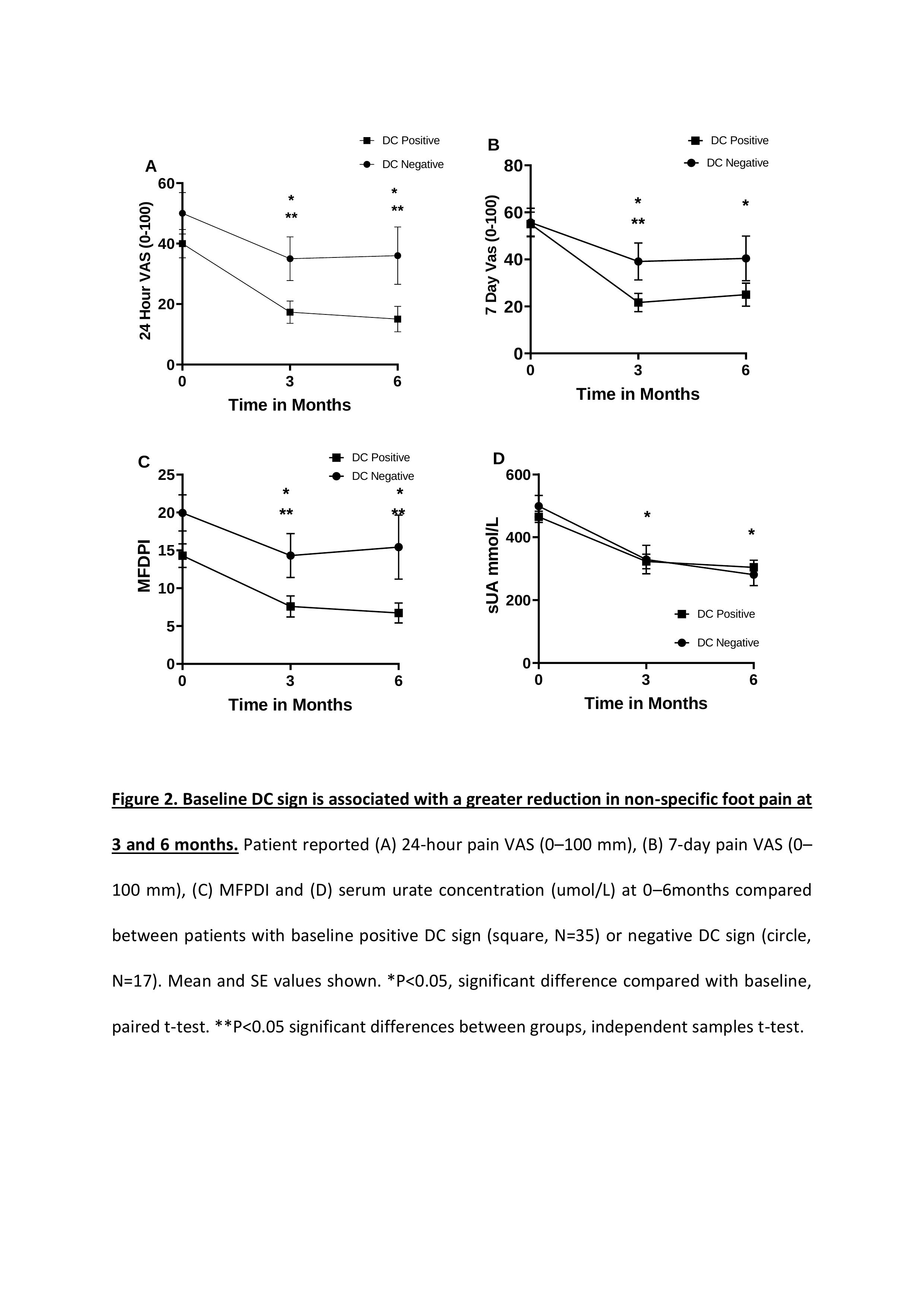
Results: 68 hyperuricaemic individuals with persistent, non-episodic foot pain were recruited, 52 cases completed the study protocol.(Table 1) At baseline MTP US DC sign, erosion and tophus occurred in 67.3%, 30.7% and 61.5% of cases, respectively. 1 control had evidence of tophus and DC sign on US examination. Baseline serum urate was higher in cases (474±12.7 mg/dL) versus controls (413±16.74; p=< 0.05). Serum urate in cases fell at 3 months (327±20; p< 0.01) and 6 months (298±18; p< 0.01). For cases, baseline 24-hour pain VAS (44±3.4) reduced at 3 months (25±3.5; p< 0.05) and 6 months (20±4.1; p< 0.05) of ULT. The 7-day pain VAS (58±3.4) decreased at 3 months (29±3.6; p< 0.05) 6 months (30±4.2; P< 0.05). MFPDI (17±1.2) decreased at 3 month (11±1.4; p=< 0.05) 6 months (10±1.6; p=< 0.05).(Figure1) When cases were grouped according to presence (N=35) or absence (N=17) of DC sign on baseline US, no differences were observed for baseline pain scores. Following ULT however, 24-hour pain VAS were significantly lower in DC positive patients at 3 months (17±3.6 DC positive vs 35±7.2 DC negative; p< 0.05) and 6 months (15.04±4.2 vs 36.00±9.5 P=< 0.05)(Figure2). Tophus but not erosion was also associated with a greater reduction in pain scores following ULT.
Conclusion: These findings indicate that persistent, non-episodic foot pain in hyperuricaemia is both associated with US features of MSU deposition and is responsive to ULT.
.jpg)
Disclosures: R. Flood, None; C. Kirby, None; y. Alammari, None; D. Kane, AbbVie/Abbott; R. Mullan, None.
Background/Purpose: Emerging evidence that joints of asymptomatic hyperuricaemic individuals contain monosodium urate (MSU) deposits and that alternative presentations of foot pain occur in hyperuricaemia suggests that preclinical phases may occur prior to a first episodic gout attack.
This case–control study evaluates urate deposition in hyperuricaemic individuals not fulfilling the ACR/EULAR 2015 gout classification criteria, as well as a potential therapeutic role for urate lowering therapy (ULT).
Methods: Following consent, hyperuricaemic individuals with persistent, non-episodic foot pain (N=68) not fulfilling ACR/EULAR 2015 gout classification criteria, were compared with asymptomatic hyperuricaemic controls (N=28). Ultrasound (US) of bilateral first metatarsophalangeal (MTP) joints and features of MSU deposition including double contour (DC) sign, tophus and erosions were recorded. Cases were treated with ULT daily for 6 months. Serum urate, 24-hour and 7-day visual analogue score (VAS) 0–100 mm pain scales the Manchester Foot Pain and Disability Index (MFPDI) and MTP US were recorded before treatment and after 3 and 6 months.
Results: 68 hyperuricaemic individuals with persistent, non-episodic foot pain were recruited, 52 cases completed the study protocol.(Table 1) At baseline MTP US DC sign, erosion and tophus occurred in 67.3%, 30.7% and 61.5% of cases, respectively. 1 control had evidence of tophus and DC sign on US examination. Baseline serum urate was higher in cases (474±12.7 mg/dL) versus controls (413±16.74; p=< 0.05). Serum urate in cases fell at 3 months (327±20; p< 0.01) and 6 months (298±18; p< 0.01). For cases, baseline 24-hour pain VAS (44±3.4) reduced at 3 months (25±3.5; p< 0.05) and 6 months (20±4.1; p< 0.05) of ULT. The 7-day pain VAS (58±3.4) decreased at 3 months (29±3.6; p< 0.05) 6 months (30±4.2; P< 0.05). MFPDI (17±1.2) decreased at 3 month (11±1.4; p=< 0.05) 6 months (10±1.6; p=< 0.05).(Figure1) When cases were grouped according to presence (N=35) or absence (N=17) of DC sign on baseline US, no differences were observed for baseline pain scores. Following ULT however, 24-hour pain VAS were significantly lower in DC positive patients at 3 months (17±3.6 DC positive vs 35±7.2 DC negative; p< 0.05) and 6 months (15.04±4.2 vs 36.00±9.5 P=< 0.05)(Figure2). Tophus but not erosion was also associated with a greater reduction in pain scores following ULT.
Conclusion: These findings indicate that persistent, non-episodic foot pain in hyperuricaemia is both associated with US features of MSU deposition and is responsive to ULT.
.jpg)
Disclosures: R. Flood, None; C. Kirby, None; y. Alammari, None; D. Kane, AbbVie/Abbott; R. Mullan, None.

