Back
Poster Session D
Crystal arthropathies
Session: (1787–1829) Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
1811: Urate Lowering Therapy Initiation in Hospitalized Patients with Acute Gout Flares
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EF
Emily Fan, BS
University of Kansas School of Medicine
Kansas City, KS, United States
Abstract Poster Presenter(s)
Emily Fan1 and Megan Krause2, 1University of Kansas School of Medicine, Kansas City, KS, 2University of Kansas, Kansas City, KS
Background/Purpose: Identifying patients with gout who would benefit from urate lowering therapies (ULT) is of utmost importance to help limit both pain and functional pain. With the recent paradigm change of immediate initiation of ULT during acute gout flares in eligible patients as recommended by the most recent American College of Rheumatology (ACR) guidelines, this study sought to assess care of hospitalized patients with acute gout.
Methods: This retrospective cohort study utilized electronic medical records to identify individuals between January 1 to December 31, 2020 with an acute gout flare during inpatient hospitalization utilizing diagnosis codes. Each individual chart was then reviewed to confirm the diagnosis of acute gout flare by the presence of MSU crystals in joint fluid or by a clinical diagnosis of gout as defined by ACR criteria. The primary outcome of interest was the proportion of eligible patients who were started on ULT during a gout flare as defined by ACR. Additional factors abstracted included use of ULT prior to admission, whether treatment recommendation occurred in the inpatient or outpatient setting, if a rheumatologist was consulted for patient care, and did those who did not receive a recommendation for treatment have indications per ACR guidelines for ULT.
Results: Nine hundred nineteen patients were identified by diagnosis code with ninety-seven adult patients who had a confirmed diagnosis of an acute gout flare while hospitalized. The average age was 62.7 ± 14.6 years and 76 (78.4%) were male.Rheumatology was consulted for 40 (41.2%) of the total patients. Sixty-seven (69.1%) of the patients experiencing an acute flare were not on ULT prior to hospital admission and 25 (37.3%) out of these 67 received a rheumatology consult. Of the total patients who were not on ULT prior to admission, 17 (25.4%) were started on ULT during their gout flare, 7 (10.4%) were started on ULT at their follow-up appointment, and 43 (64.2%) were not offered ULT during their gout flare or after their hospitalization. 12/25 (48%) of patients with a rheumatologist on their care team received ULT while 12/42 (26.8%) of patients without a rheumatology consult received ULT. Out of the patients who did not receive ULT, 20 (46.5%) were eligible for therapy. The most common indication for initiating ULT in these patients was chronic kidney disease stage III or higher (13 [65%]), followed by two or more flares in one year (12 [60%]), and uric acid >9mg/dL (9 [45%]). Ten (50%) of the patients who were eligible for ULT but did not receive treatment had two or more indications for starting treatment.
Conclusion: This study identifies that most individuals, if started on ULT, do so after an acute flare and that there were individuals who could have been initiated on ULT but were not. The hospitalized setting is a potential opportunity to initiate more long term care plans for gout. Future interventions could include assessment of treatment algorithms in hospitalized patients.
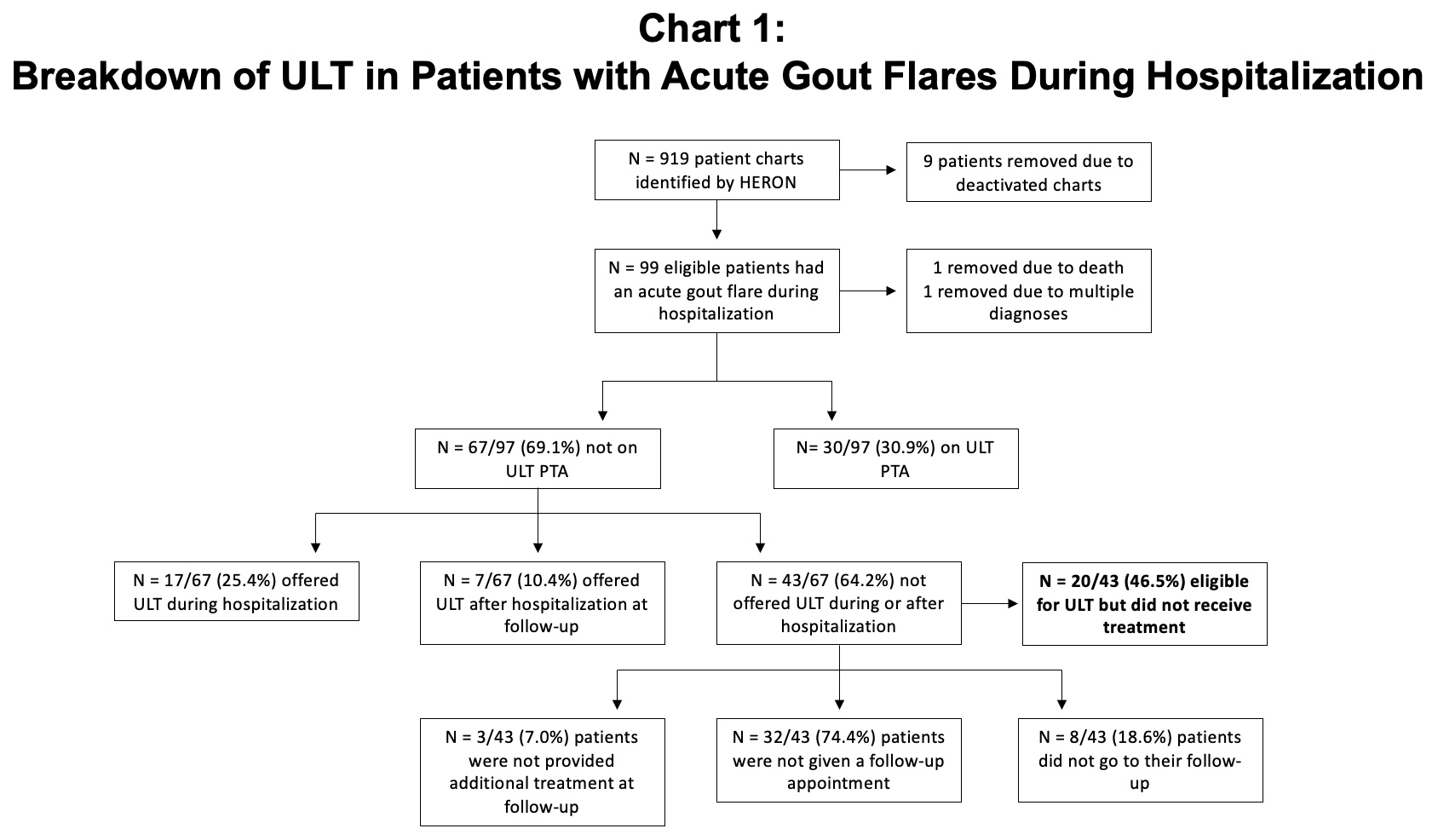 Chart 1: Breakdown of ULT in patients with acute gout flares during hospitalization
Chart 1: Breakdown of ULT in patients with acute gout flares during hospitalization
Disclosures: E. Fan, None; M. Krause, None.
Background/Purpose: Identifying patients with gout who would benefit from urate lowering therapies (ULT) is of utmost importance to help limit both pain and functional pain. With the recent paradigm change of immediate initiation of ULT during acute gout flares in eligible patients as recommended by the most recent American College of Rheumatology (ACR) guidelines, this study sought to assess care of hospitalized patients with acute gout.
Methods: This retrospective cohort study utilized electronic medical records to identify individuals between January 1 to December 31, 2020 with an acute gout flare during inpatient hospitalization utilizing diagnosis codes. Each individual chart was then reviewed to confirm the diagnosis of acute gout flare by the presence of MSU crystals in joint fluid or by a clinical diagnosis of gout as defined by ACR criteria. The primary outcome of interest was the proportion of eligible patients who were started on ULT during a gout flare as defined by ACR. Additional factors abstracted included use of ULT prior to admission, whether treatment recommendation occurred in the inpatient or outpatient setting, if a rheumatologist was consulted for patient care, and did those who did not receive a recommendation for treatment have indications per ACR guidelines for ULT.
Results: Nine hundred nineteen patients were identified by diagnosis code with ninety-seven adult patients who had a confirmed diagnosis of an acute gout flare while hospitalized. The average age was 62.7 ± 14.6 years and 76 (78.4%) were male.Rheumatology was consulted for 40 (41.2%) of the total patients. Sixty-seven (69.1%) of the patients experiencing an acute flare were not on ULT prior to hospital admission and 25 (37.3%) out of these 67 received a rheumatology consult. Of the total patients who were not on ULT prior to admission, 17 (25.4%) were started on ULT during their gout flare, 7 (10.4%) were started on ULT at their follow-up appointment, and 43 (64.2%) were not offered ULT during their gout flare or after their hospitalization. 12/25 (48%) of patients with a rheumatologist on their care team received ULT while 12/42 (26.8%) of patients without a rheumatology consult received ULT. Out of the patients who did not receive ULT, 20 (46.5%) were eligible for therapy. The most common indication for initiating ULT in these patients was chronic kidney disease stage III or higher (13 [65%]), followed by two or more flares in one year (12 [60%]), and uric acid >9mg/dL (9 [45%]). Ten (50%) of the patients who were eligible for ULT but did not receive treatment had two or more indications for starting treatment.
Conclusion: This study identifies that most individuals, if started on ULT, do so after an acute flare and that there were individuals who could have been initiated on ULT but were not. The hospitalized setting is a potential opportunity to initiate more long term care plans for gout. Future interventions could include assessment of treatment algorithms in hospitalized patients.
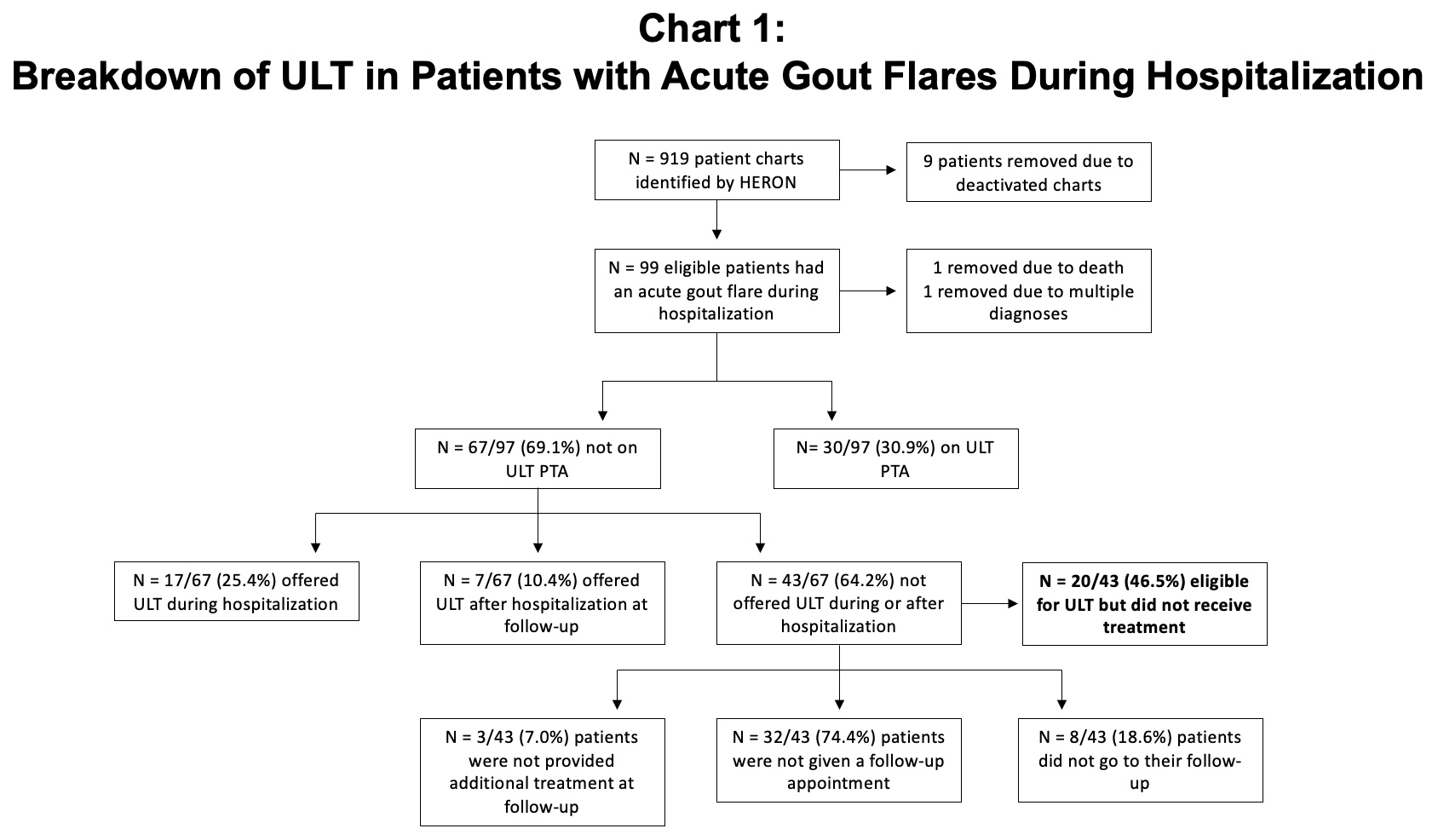 Chart 1: Breakdown of ULT in patients with acute gout flares during hospitalization
Chart 1: Breakdown of ULT in patients with acute gout flares during hospitalizationDisclosures: E. Fan, None; M. Krause, None.

