Back
Poster Session D
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1856–1887) Muscle Biology, Myositis and Myopathies Poster II
1880: Vaccine Hesitancy Among Patients with Idiopathic Inflammatory Myopathies and Rheumatic Diseases in 2021-2022: A Comparative Analysis of COVID-19 Vaccination in Autoimmune Diseases Surveys
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Naveen R, DM
Sanjay Gandhi Post graduate institute of medical sciences
Lucknow, Uttar Pradesh, India
Abstract Poster Presenter(s)
Naveen R1, Mrudula Joshi2, Parikshit Sen3, Vishwesh Agarwal4, Samuel Shinjo5, Sinan Kardes6, James B. Lilleker7, Hector Chinoy8, Ashima Makol9, Oliver Distler10, Minchul Kim11, Elena Nikiphorou12, Ai Lyn Tan13, Babur Salim14, Tamer A Gheita15, Nelly Ziade16, Tsvetelina Velikova17, Tulika Chatterjee11, Arvind Nune18, Marcin Milchert19, Ioannis Parodis20, Abraham Edgar Gracia-Ramos21, Albert Selva O’Callaghan22, Miguel Angel Saavedra Salinas23, Lorenzo Cavagna24, Masataka Kuwana25, Johannes Knitza26, Jessica Day27, Carlos Enrique Toro Gutiérrez28, Carlo Caballero29, Dzifa Dey30, Erick Zamora Tehozol31, Jorge Rojas Serrano32, Ignacio Garcia-De La Torre33, Iris Colunga34, Javier Merayo-Chalico35, John Pauling36, Chris Wincup37, Armen Yuri Gasparyan38, Vikas Agarwal1, Rohit Aggarwal39 and Latika Gupta40, 1Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, 2Byramjee Jeejeebhoy Government Medical College and Sassoon General Hospitals, Pune, India, 3Maulana Azad Medical College, New Delhi, India, 4Mahatma Gandhi Missions Medical College, Lucknow, India, 5Faculdade de Medicina FMUSP, Universidade de São Paulo, São Paulo, Brazil, 6Istanbul University, Istanbul, Turkey, 7The University of Manchester, Manchester, United Kingdom, 8The University of Manchester, Sale, United Kingdom, 9Mayo Clinic, Rochester, MN, Rochester, MN, 10Department of Rheumatology, University Hospital Zurich, University of Zurich, Zürich, Switzerland, 11University of Illinois College of Medicine Peoria, Peoria, IL, 12Leiden University Medical Center & King's College London, London, United Kingdom, 13University of Leeds, Leeds, United Kingdom, 14Fauji foundation hospital Rawalpindi, Rawalpindi, Pakistan, 15Rheumatology Department, Faculty of Medicine, Cairo University, Cairo, Egypt, 16Saint-Joseph University, Beirut, Lebanon, 17Sofia University St. Kliment Ohridski, Sofia, Bulgaria, 18Southport and Ormskirk Hospital NHS Trust, Southport, United Kingdom, 19Pomeranian Medical University in Szczecin, Szczecin, Poland, 20Karolinska Institutet, Stockholm, Sweden, 21Instituto Mexicano del Seguro Social, Ciudad de México, Mexico, 22Hospital Universitari Vall d'Hebron, Barcelona, Spain, 23IMSS, Ciudad de México, Mexico, 24Università di Pavia, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, Pavia, Italy, 25Nippon Medical School Graduate School of Medicine, Tokyo, Japan, 26Department of Internal Medicine 3 – Rheumatology and Immunology, Friedrich-Alexander-University Erlangen-Nürnberg and Universitätsklinikum Erlangen, 91054 Erlangen, Germany; Deutsches Zentrum Immuntherapie, Friedrich-Alexander-UniversityErlangen-Nürnberg and Universitätsklinikum Erlangen, Erlangen, Germany, 27Walter and Eliza Hall Institute, Melbourne, Australia, 28Internal Medicine and Rheumatology, Reference Center for Osteoporosis, Rheumatology & Dermatology. Pontificia Javeriana University, Calí, Colombia, 29Universidad del Norte, Barranquilla, Colombia, 30University of Ghana School of Medicine and Dentistry, Accra, Ghana, 31Centro Medico Pensiones, Merida, Mexico, 32Hospital Angeles Villahermosa, Ciudad de México, Mexico, 33Centro de Est. de Inv. Bas. y Clinica, S.C., Guadalajara, Mexico, 34Hospital Universitario UANL, Monterrey, Mexico, 35Instituto Nacional de Ciencias Medicas y Nutricion "Salvador Zubiran", Ciudad de México, Mexico, 36North Bristol NHS Trust, Bristol, United Kingdom, 37Rayne Institute, University College London, London, United Kingdom, 38Dudley Group NHS Foundation Trust, Dudley, United Kingdom, 39Division of Rheumatology and Clinical Immunology, Department of Medicine, University of Pittsburgh, Pittsburgh, PA, 40Royal Wolverhampton Trust, Wolverhampton/University of Manchester, United Kingdom
Background/Purpose: Patients with comorbidities and active rheumatic disease have increased morbidity and hospitalization following SARS-CoV-2 infection. While vaccination has decreased this, many unknown factors still influence COVID-19 vaccine hesitancy. The data on predictors of vaccine hesitancy is regional and scarce. We aimed to analyze the factors influencing vaccine hesitancy in 2022 and compare them with those in 2021 through multicentre international e-surveys (The COVID-19 Vaccination in Autoimmune Diseases Studies - COVAD study 1 and 2).
Methods: COVAD 1 and 2 are multi-centre international e-survey with 152 collaborators in 106 countries including patients with idiopathic inflammatory myopathies (IIM), autoimmune rheumatic diseases (AIRDs), other autoimmune diseases (AIDs), and healthy controls (HCs) conducted in March-December 2021 and February-June 2022 (ongoing), respectively. Descriptive and multivariable regression adjusting for age, gender, ethnicity, and stratified by country of residence was performed.
Results: Among the 18882 (2021) and 7666 complete responses (2022), and 3109 (16.5%) and 387 (5.1%) did not receive any COVID-19 vaccine, respectively. The prevalence of vaccine hesitancy has decreased [OR 0.26 (0.24-0.3), p< 0.001]. Among the 387 vaccine non-recipients in 2022, numbers were as follows: IIM 69 (17%), AIRDs 179 (46%), other AIDs 80 (20.6%), and HC 59 (15%). The reasons for vaccine hesitancy in 2022 included: doctor advising against it 47 (12%), don't believe in the science behind the vaccine 79 (21%), long-term safety concerns 152 (39%), awaiting more safety data 105 (27%), and not recommended due to recent infection 30 (7%).
Compared to AIRDs and HCs, IIM patients were more disbelievers of the science behind the vaccine [OR 1.8 (1.08-3.2), p=0.023 AIRDs, OR 4 (1.9-8.1), p< 0.001 HC], had more long-term safety concerns [OR 1.9 (1.2-2.9), p=0.001 AIRDs, OR 5.4 (3-9.6), p< 0.001 HC] and had more doctors recommending against the vaccine [OR 12.9 (2.8-59), p< 0.001 HC] (Figure 1).
Vaccine non-recipients had higher pain visual analog score (VAS) (p< 0.001), lower fatigue VAS (p=0.003), lower PROMIS10a physical health (p< 0.001), and mental health scores (p=0.015) (Table 1).
The factors predicting vaccine hesitancy in regression were lower PROMIS10a global physical health score [OR 0.9 (0.8-0.97), p=0.014] and Caucasian ethnicity [OR 4.2 (1.7-10.3), p=0.001].
Compared to 2021, doctor's advising against vaccination [OR 2.5 (1.8-3.6), p< 0.001] and long-term safety concerns [OR 3.6 (2.9-4.6), p< 0.001] were more frequent causes of vaccine hesitancy overall whereas vaccine non-availability [OR 0.05 (0.02-0.11), p< 0.001] and have scheduled the vaccination but not received [OR 0.1 (0.06-0.3), p< 0.001] were less frequent causes in 2022 (Figure 2).
Conclusion: Overall, the prevalence of COVID-19 vaccine hesitancy has decreased. Long-term safety concerns and the need for more safety data are now the major reasons for vaccine hesitancy. Caucasian ethnicity and lower physical health scores are predictors of vaccine hesitancy. The increase in physicians recommending against vaccination calls for more physician awareness to mitigate vaccine hesitancy.
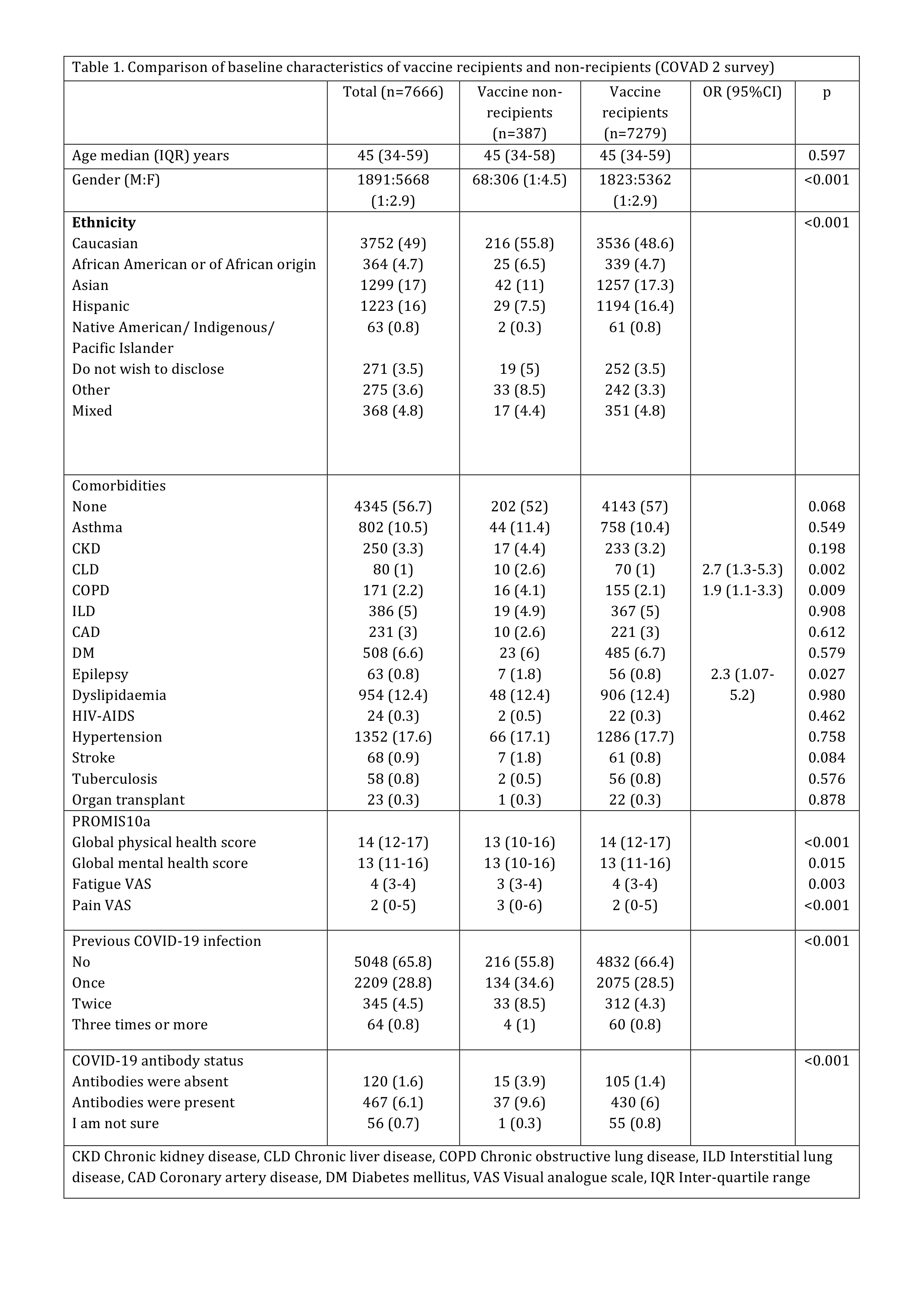 Table 1. Comparison of baseline characteristics of vaccine recipients and non-recipients (COVAD 2 survey)
Table 1. Comparison of baseline characteristics of vaccine recipients and non-recipients (COVAD 2 survey)
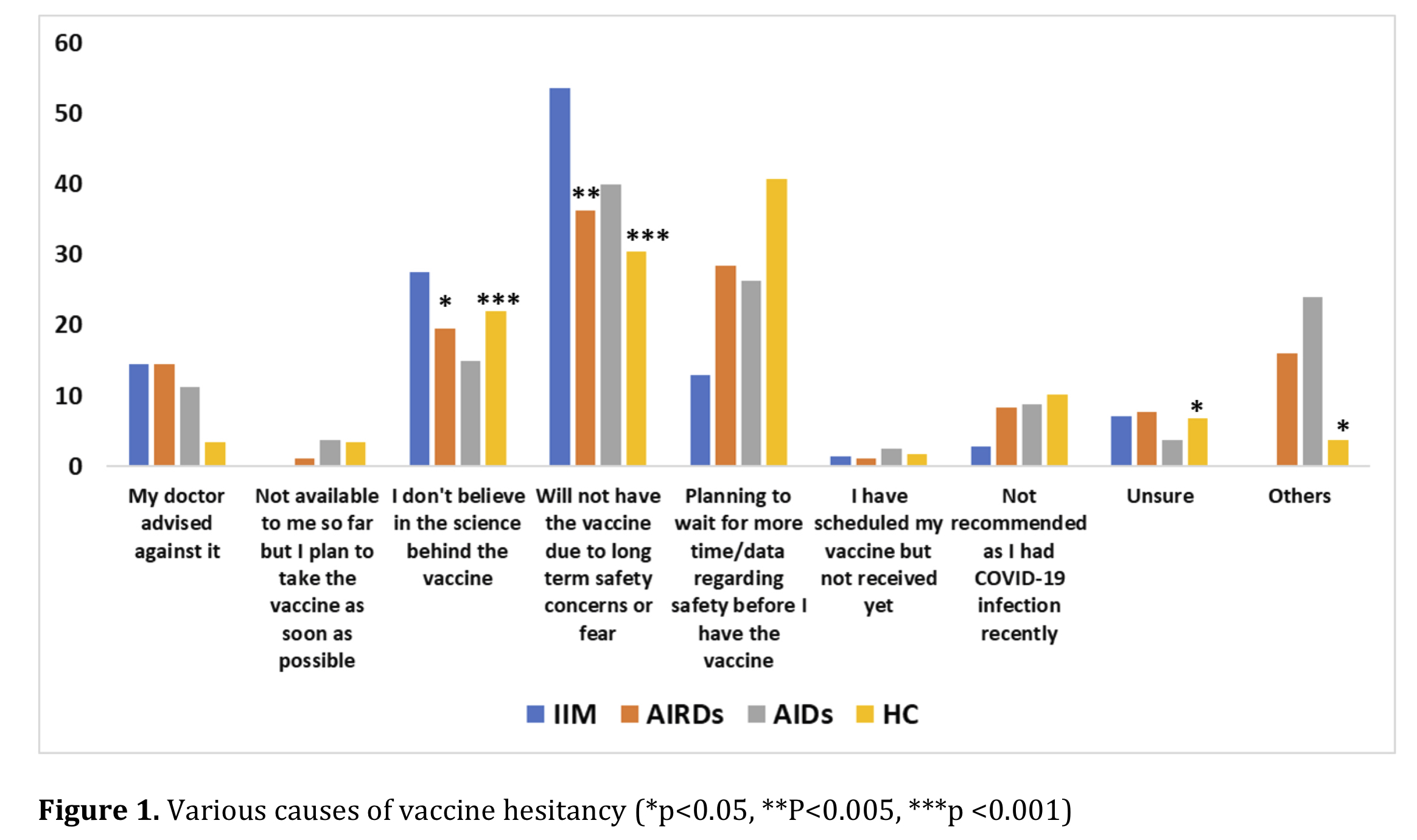 Figure 1. Various causes of vaccine hesitancy
Figure 1. Various causes of vaccine hesitancy
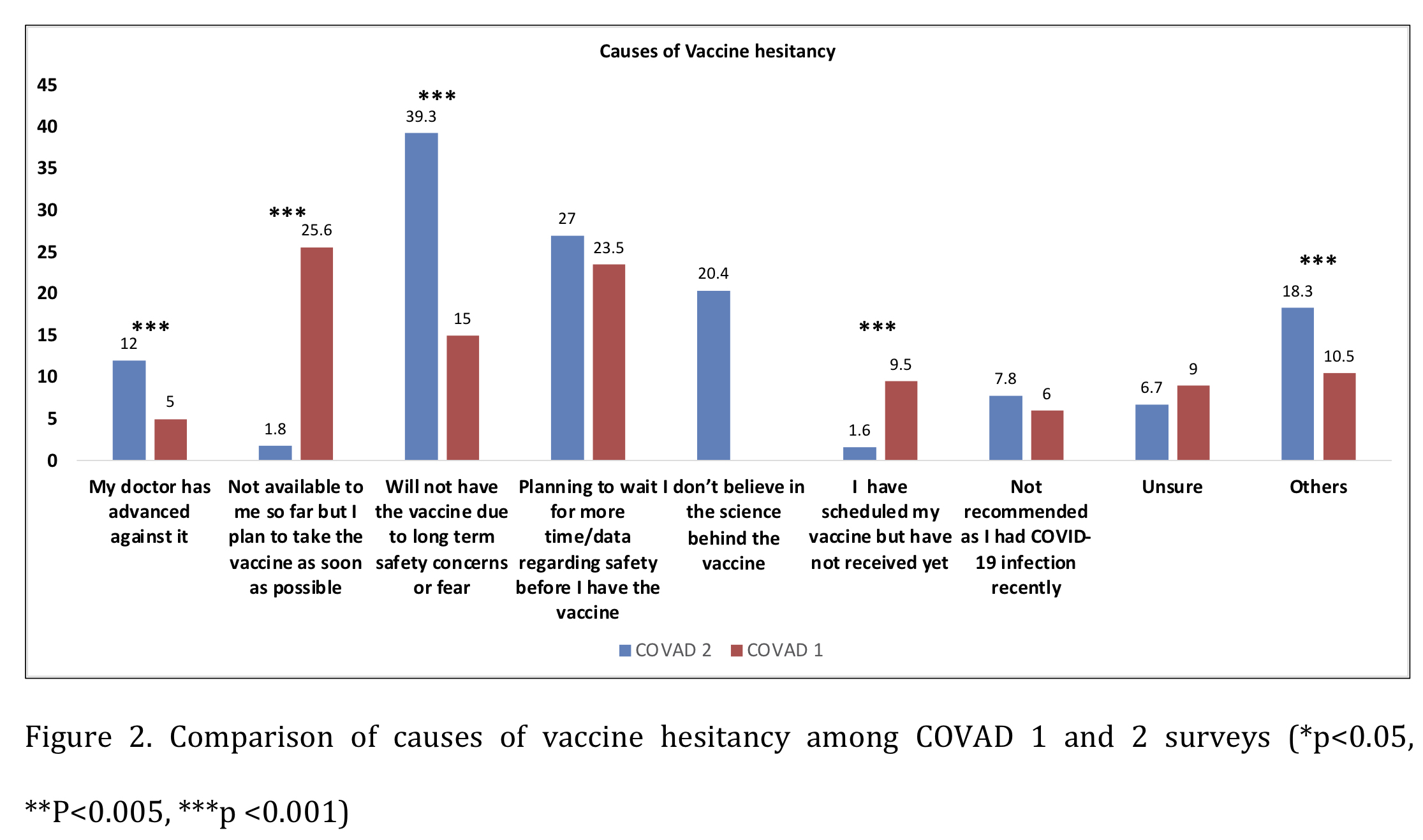 Figure 2. Comparison of causes of vaccine hesitancy among COVAD 1 and 2 surveys
Figure 2. Comparison of causes of vaccine hesitancy among COVAD 1 and 2 surveys
Disclosures: N. R, None; M. Joshi, None; P. Sen, None; V. Agarwal, None; S. Shinjo, None; S. Kardes, None; J. Lilleker, None; H. Chinoy, Eli Lilly, UCB; A. Makol, Boehringer-Ingelheim; O. Distler, AbbVie/Abbott, Amgen, GlaxoSmithKlein(GSK), Novartis, Roche, UCB, Kymera, Mitsubishi Tanabe, Boehringer Ingelheim, 4P-Pharma, Acceleron, Alcimed, Altavant Sciences, AnaMar, Arxx, AstraZeneca, Blade Therapeutics, Bayer, Corbus Pharmaceuticals, CSL Behring, Galapagos, Glenmark, Horizon, Inventiva, Lupin, Miltenyi Biotec, Merck/MSD, Prometheus Biosciences, Redx Pharma, Roivant, Sanofi, Topadur, Pfizer, Janssen, Medscape, Patent issued “mir-29 for the treatment of systemic sclerosis” (US8247389, EP2331143), FOREUM Foundation, ERS/EULAR Guidelines, EUSTAR, SCQM (Swiss Clinical Quality Management in Rheumatic Diseases), Swiss Academy of Medical Sciences (SAMW), Hartmann Müller Foundation; M. Kim, None; E. Nikiphorou, Pfizer, Celltrion, Sanofi, Gilead, Galapagos, AbbVie, Lilly, Fresenius; A. Tan, None; B. Salim, None; T. Gheita, None; N. Ziade, Pfizer, Roche, AbbVie/Abbott, Eli Lilly, Boehringer-Ingelheim, Janssen; T. Velikova, None; T. Chatterjee, None; A. Nune, None; M. Milchert, None; I. Parodis, GlaxoSmithKlein(GSK), Amgen, AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, Gilead, Janssen, Novartis, Roche; A. Gracia-Ramos, None; A. O’Callaghan, None; M. Saavedra Salinas, GlaxoSmithKlein(GSK), AbbVie/Abbott; L. Cavagna, None; M. Kuwana, Boehringer-Ingelheim, Ono pharmaceuticals, Mochida, AbbVie/Abbott, Astellas, Janssen, Bayer, Corbus, Horizon; J. Knitza, AbbVie, Novartis, ThermoFisher, UCB, ABATON, Sanofi, Medac, Lilly, BMS, Gilead, GSK, Werfen, Vila Health, Böhringer Ingelheim, Janssen, Galapagos, Chugai; J. Day, CSL; C. Toro Gutiérrez, AbbVie, Amgen, Biopas, Bristol-Myers Squibb(BMS), Boehringer-Ingelheim, Janssen, Pfizer, Roche, Novartis; C. Caballero, None; D. Dey, None; E. Zamora Tehozol, None; J. Rojas Serrano, None; I. Garcia-De La Torre, None; I. Colunga, None; J. Merayo-Chalico, Janssen, Sanofi; J. Pauling, None; C. Wincup, None; A. Gasparyan, None; V. Agarwal, None; R. Aggarwal, Mallinckrodt, Bristol Myers Squibb, EMD Serono, Pfizer, Octapharma, CSL Behring, Q32, Kezar, AstraZeneca, Alexion, Argenx, Boehringer Ingelheim, Corbus, Janssen, Kyverna, Roivant, AbbVie, Jubilant, Orphazyme, Genentech; L. Gupta, None.
Background/Purpose: Patients with comorbidities and active rheumatic disease have increased morbidity and hospitalization following SARS-CoV-2 infection. While vaccination has decreased this, many unknown factors still influence COVID-19 vaccine hesitancy. The data on predictors of vaccine hesitancy is regional and scarce. We aimed to analyze the factors influencing vaccine hesitancy in 2022 and compare them with those in 2021 through multicentre international e-surveys (The COVID-19 Vaccination in Autoimmune Diseases Studies - COVAD study 1 and 2).
Methods: COVAD 1 and 2 are multi-centre international e-survey with 152 collaborators in 106 countries including patients with idiopathic inflammatory myopathies (IIM), autoimmune rheumatic diseases (AIRDs), other autoimmune diseases (AIDs), and healthy controls (HCs) conducted in March-December 2021 and February-June 2022 (ongoing), respectively. Descriptive and multivariable regression adjusting for age, gender, ethnicity, and stratified by country of residence was performed.
Results: Among the 18882 (2021) and 7666 complete responses (2022), and 3109 (16.5%) and 387 (5.1%) did not receive any COVID-19 vaccine, respectively. The prevalence of vaccine hesitancy has decreased [OR 0.26 (0.24-0.3), p< 0.001]. Among the 387 vaccine non-recipients in 2022, numbers were as follows: IIM 69 (17%), AIRDs 179 (46%), other AIDs 80 (20.6%), and HC 59 (15%). The reasons for vaccine hesitancy in 2022 included: doctor advising against it 47 (12%), don't believe in the science behind the vaccine 79 (21%), long-term safety concerns 152 (39%), awaiting more safety data 105 (27%), and not recommended due to recent infection 30 (7%).
Compared to AIRDs and HCs, IIM patients were more disbelievers of the science behind the vaccine [OR 1.8 (1.08-3.2), p=0.023 AIRDs, OR 4 (1.9-8.1), p< 0.001 HC], had more long-term safety concerns [OR 1.9 (1.2-2.9), p=0.001 AIRDs, OR 5.4 (3-9.6), p< 0.001 HC] and had more doctors recommending against the vaccine [OR 12.9 (2.8-59), p< 0.001 HC] (Figure 1).
Vaccine non-recipients had higher pain visual analog score (VAS) (p< 0.001), lower fatigue VAS (p=0.003), lower PROMIS10a physical health (p< 0.001), and mental health scores (p=0.015) (Table 1).
The factors predicting vaccine hesitancy in regression were lower PROMIS10a global physical health score [OR 0.9 (0.8-0.97), p=0.014] and Caucasian ethnicity [OR 4.2 (1.7-10.3), p=0.001].
Compared to 2021, doctor's advising against vaccination [OR 2.5 (1.8-3.6), p< 0.001] and long-term safety concerns [OR 3.6 (2.9-4.6), p< 0.001] were more frequent causes of vaccine hesitancy overall whereas vaccine non-availability [OR 0.05 (0.02-0.11), p< 0.001] and have scheduled the vaccination but not received [OR 0.1 (0.06-0.3), p< 0.001] were less frequent causes in 2022 (Figure 2).
Conclusion: Overall, the prevalence of COVID-19 vaccine hesitancy has decreased. Long-term safety concerns and the need for more safety data are now the major reasons for vaccine hesitancy. Caucasian ethnicity and lower physical health scores are predictors of vaccine hesitancy. The increase in physicians recommending against vaccination calls for more physician awareness to mitigate vaccine hesitancy.
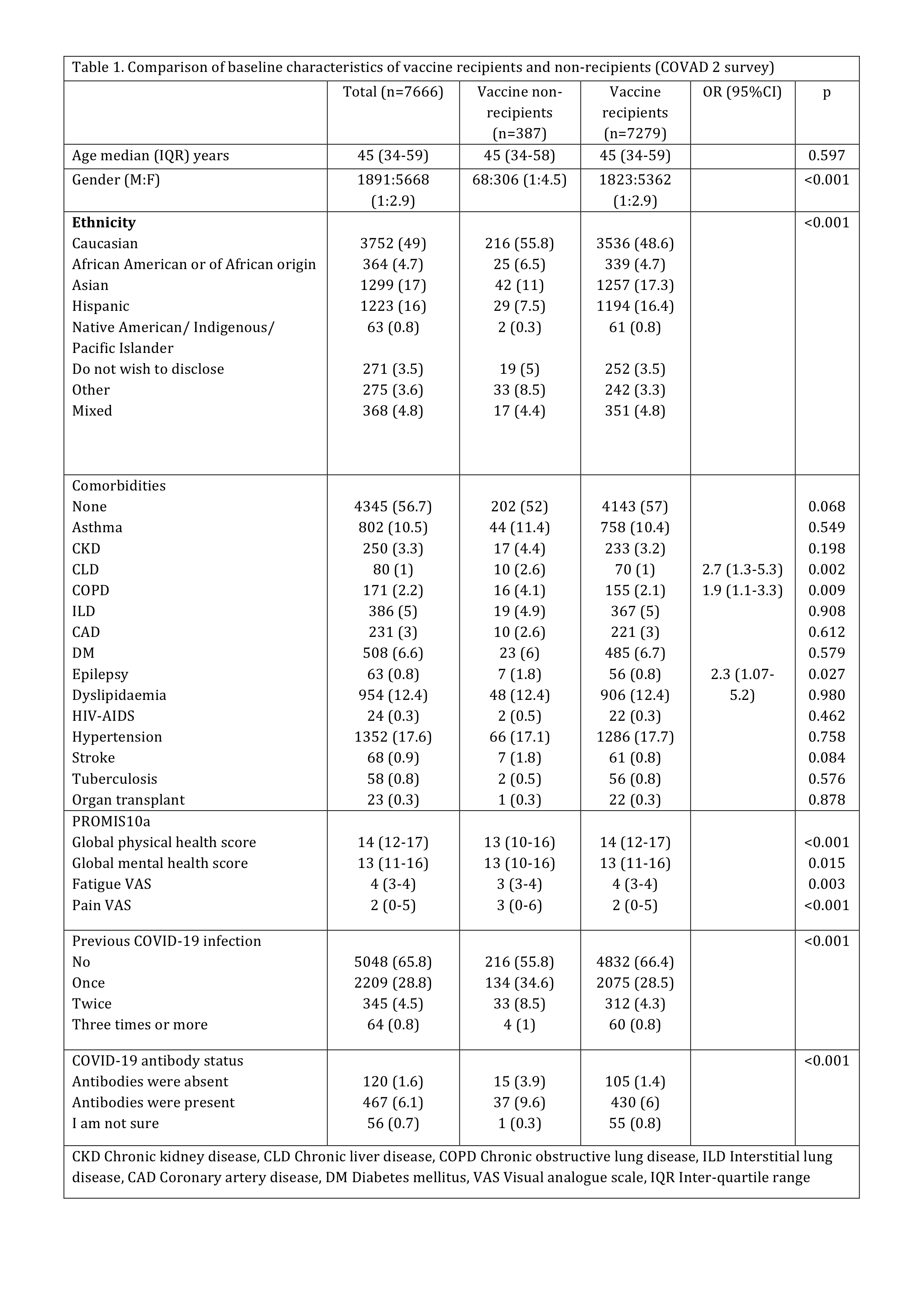 Table 1. Comparison of baseline characteristics of vaccine recipients and non-recipients (COVAD 2 survey)
Table 1. Comparison of baseline characteristics of vaccine recipients and non-recipients (COVAD 2 survey)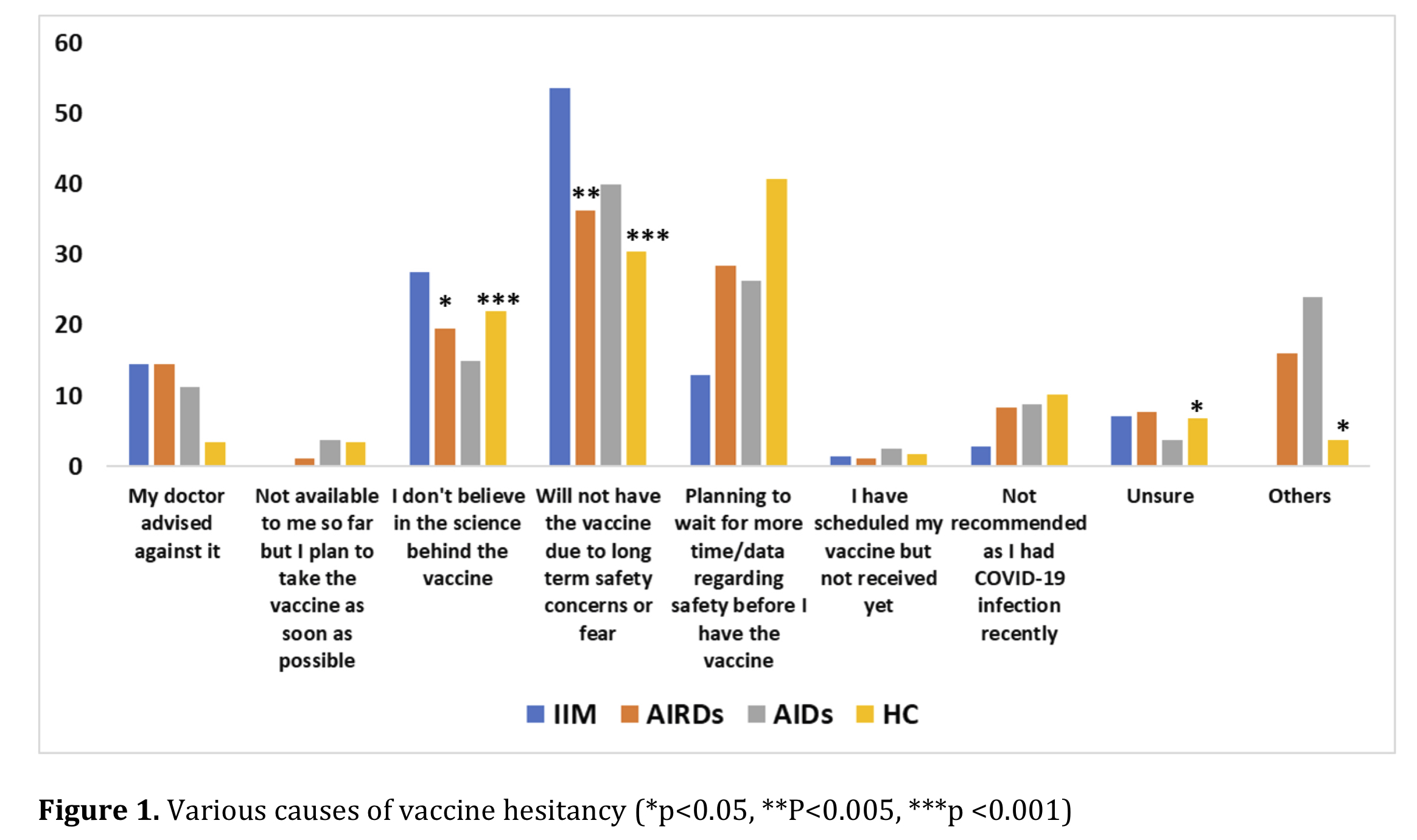 Figure 1. Various causes of vaccine hesitancy
Figure 1. Various causes of vaccine hesitancy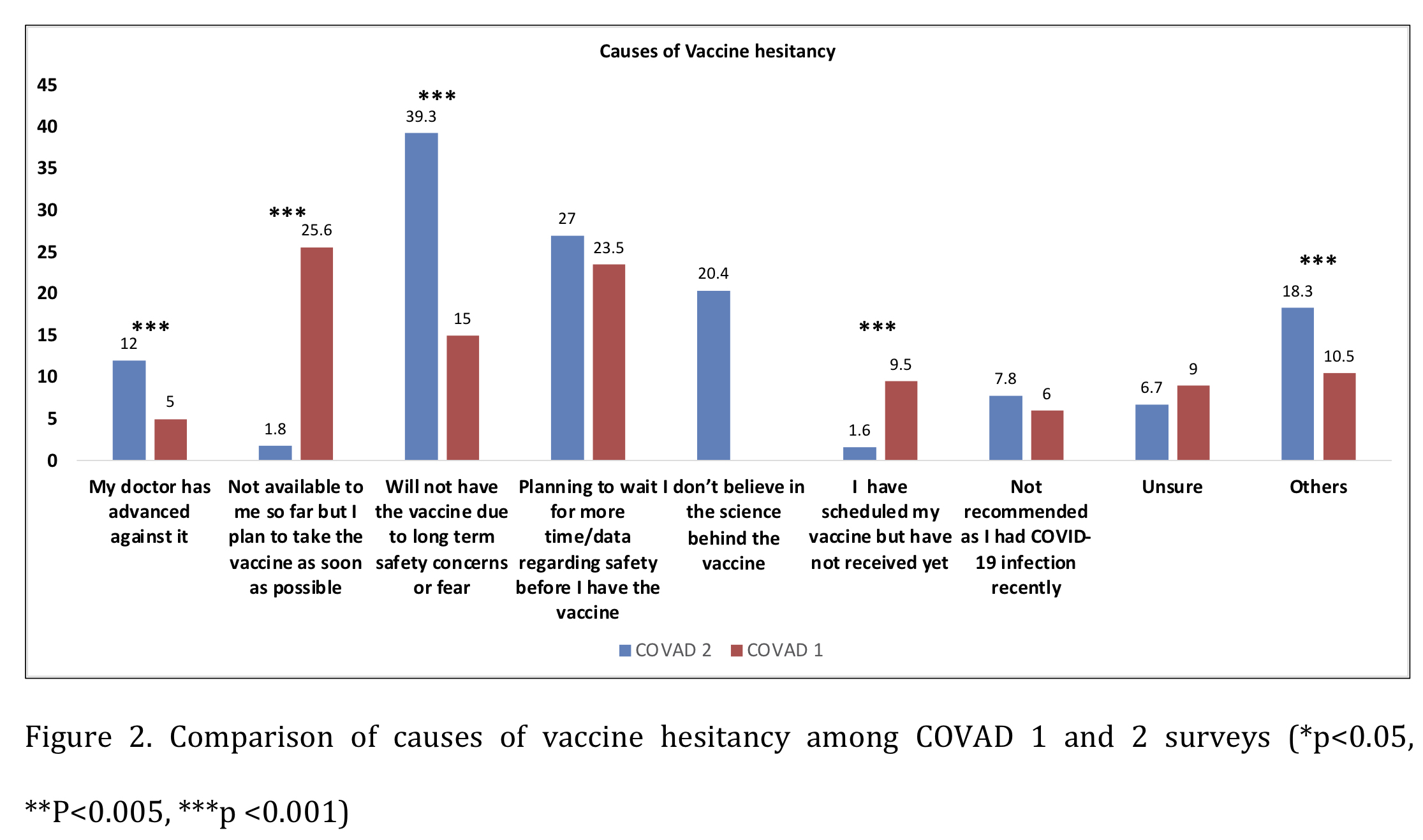 Figure 2. Comparison of causes of vaccine hesitancy among COVAD 1 and 2 surveys
Figure 2. Comparison of causes of vaccine hesitancy among COVAD 1 and 2 surveysDisclosures: N. R, None; M. Joshi, None; P. Sen, None; V. Agarwal, None; S. Shinjo, None; S. Kardes, None; J. Lilleker, None; H. Chinoy, Eli Lilly, UCB; A. Makol, Boehringer-Ingelheim; O. Distler, AbbVie/Abbott, Amgen, GlaxoSmithKlein(GSK), Novartis, Roche, UCB, Kymera, Mitsubishi Tanabe, Boehringer Ingelheim, 4P-Pharma, Acceleron, Alcimed, Altavant Sciences, AnaMar, Arxx, AstraZeneca, Blade Therapeutics, Bayer, Corbus Pharmaceuticals, CSL Behring, Galapagos, Glenmark, Horizon, Inventiva, Lupin, Miltenyi Biotec, Merck/MSD, Prometheus Biosciences, Redx Pharma, Roivant, Sanofi, Topadur, Pfizer, Janssen, Medscape, Patent issued “mir-29 for the treatment of systemic sclerosis” (US8247389, EP2331143), FOREUM Foundation, ERS/EULAR Guidelines, EUSTAR, SCQM (Swiss Clinical Quality Management in Rheumatic Diseases), Swiss Academy of Medical Sciences (SAMW), Hartmann Müller Foundation; M. Kim, None; E. Nikiphorou, Pfizer, Celltrion, Sanofi, Gilead, Galapagos, AbbVie, Lilly, Fresenius; A. Tan, None; B. Salim, None; T. Gheita, None; N. Ziade, Pfizer, Roche, AbbVie/Abbott, Eli Lilly, Boehringer-Ingelheim, Janssen; T. Velikova, None; T. Chatterjee, None; A. Nune, None; M. Milchert, None; I. Parodis, GlaxoSmithKlein(GSK), Amgen, AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, Gilead, Janssen, Novartis, Roche; A. Gracia-Ramos, None; A. O’Callaghan, None; M. Saavedra Salinas, GlaxoSmithKlein(GSK), AbbVie/Abbott; L. Cavagna, None; M. Kuwana, Boehringer-Ingelheim, Ono pharmaceuticals, Mochida, AbbVie/Abbott, Astellas, Janssen, Bayer, Corbus, Horizon; J. Knitza, AbbVie, Novartis, ThermoFisher, UCB, ABATON, Sanofi, Medac, Lilly, BMS, Gilead, GSK, Werfen, Vila Health, Böhringer Ingelheim, Janssen, Galapagos, Chugai; J. Day, CSL; C. Toro Gutiérrez, AbbVie, Amgen, Biopas, Bristol-Myers Squibb(BMS), Boehringer-Ingelheim, Janssen, Pfizer, Roche, Novartis; C. Caballero, None; D. Dey, None; E. Zamora Tehozol, None; J. Rojas Serrano, None; I. Garcia-De La Torre, None; I. Colunga, None; J. Merayo-Chalico, Janssen, Sanofi; J. Pauling, None; C. Wincup, None; A. Gasparyan, None; V. Agarwal, None; R. Aggarwal, Mallinckrodt, Bristol Myers Squibb, EMD Serono, Pfizer, Octapharma, CSL Behring, Q32, Kezar, AstraZeneca, Alexion, Argenx, Boehringer Ingelheim, Corbus, Janssen, Kyverna, Roivant, AbbVie, Jubilant, Orphazyme, Genentech; L. Gupta, None.

