Back
Ignite Talk
Session: Ignite Session 1A
0912: Associations Between Fatty Acid Amide Hydrolase Variants and Response to Cannabis Use for Pain Management in Rheumatoid Arthritis
Saturday, November 12, 2022
1:00 PM – 1:05 PM Eastern Time
Location: Northern Liberties Stage

Kristin Wipfler, PhD
FORWARD, The National Databank for Rheumatic Diseases
Omaha, NE, United StatesDisclosure: Disclosure information not submitted.
Ignite Speaker(s)
Kristin Wipfler1, Joanna Zeiger2, Teresa Simon3, Stuart Kassan4 and Kaleb Michaud5, 1FORWARD, The National Databank for Rheumatic Diseases, Omaha, NE, 2Canna Research Foundation, Boulder, CO, 3Physicians Research Center Consultant to ForWard, Toms River, NJ, 4Colorado Arthritis Associates, Lakewood, CO, 5University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Fatty acid amide hydrolase (FAAH) is a serine hydrolase that breaks down the endocannabinoid/cannabinoid receptor agonist anandamide. Variants in the FAAH gene have been associated with pain susceptibility as well as with cannabis use. In addition, FAAH inhibition has been shown to have anti-arthritic and pain reduction effects in collagen-induced arthritis mouse models. The objective of this study was to examine relationships between FAAH variants and cannabis use as well as real-world effectiveness in pain management for individuals with rheumatoid arthritis (RA).
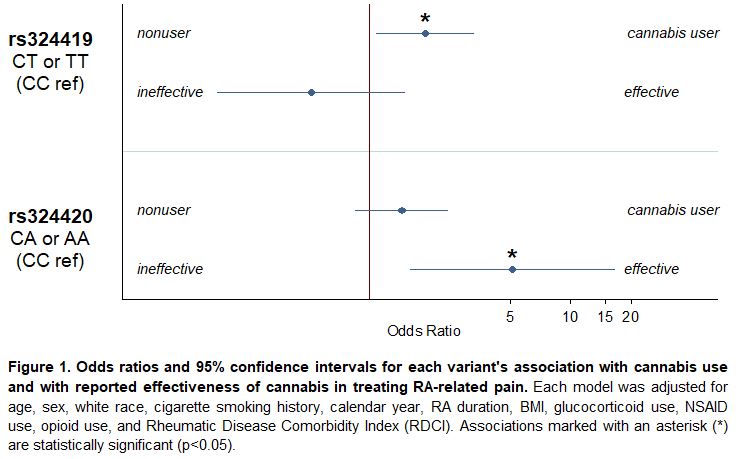
Methods: Data were provided by adults with RA participating in FORWARD, The National Databank for Rheumatic Diseases, who provided blood samples and answered questions about cannabis use (defined as use of products containing THC and/or CBD). Genotyping was performed with the Illumina Infinium Global Screening Array platform, and non-silent common FAAH variants (minor allele frequency >0.5; SNPs rs324419 and rs324420) were included in this analysis. Logistic regression models for cannabis use vs nonuse and for self-reported effectiveness in pain management (helpful vs not helpful) were generated for each variant by presence or absence of the minor allele. Models were adjusted for age, sex, white race, cigarette smoking history, calendar year, RA duration, BMI, glucocorticoid use, NSAID use, opioid use, and Rheumatic Disease Comorbidity Index (RDCI).
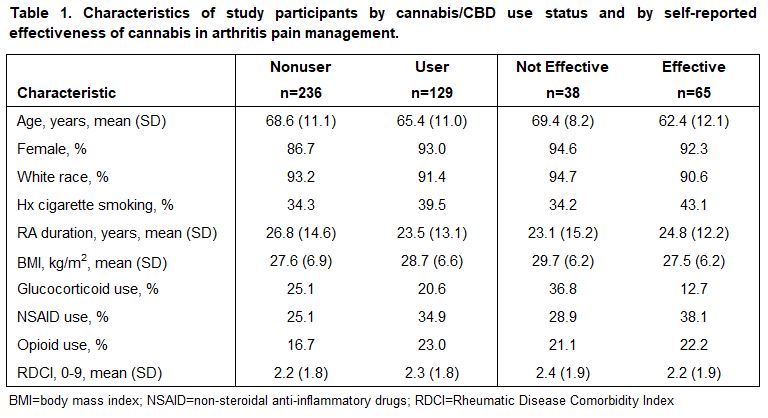
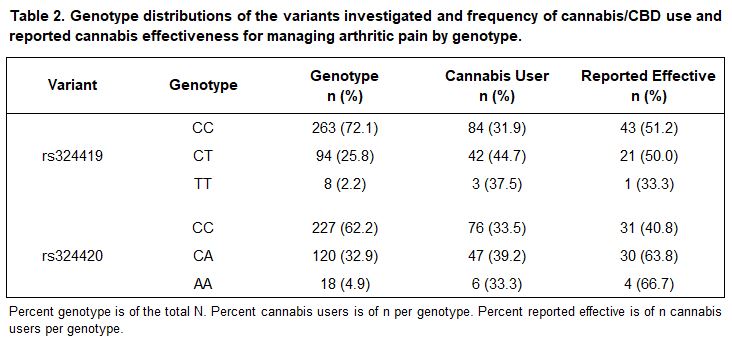
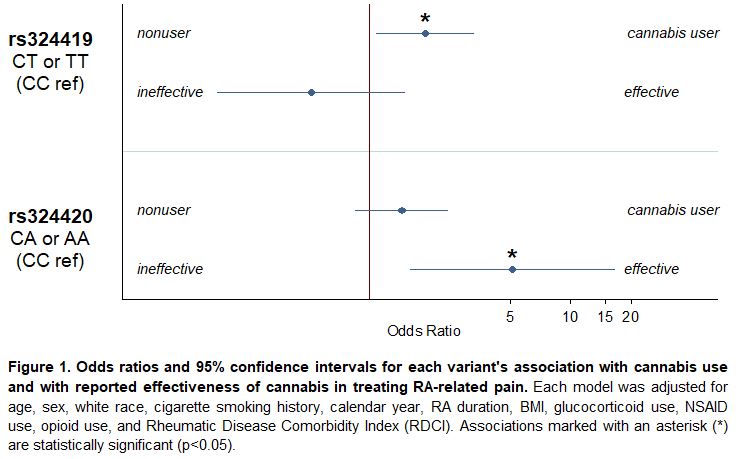
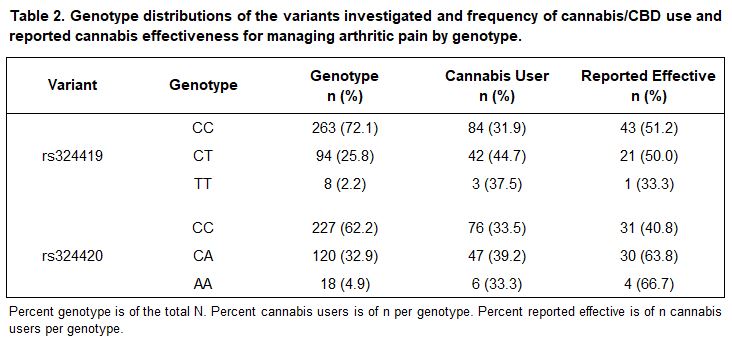
Results: A total of 365 participants met inclusion criteria, 129 (35.3%) of whom reported cannabis use as a treatment for arthritic pain. Among users, 52% reported that cannabis was helpful in reducing their pain, 30% reported that it was not helpful, and 18% reported that they were not sure (Table 1). Genotype distributions of both variants are presented in Table 2. In multivariable models for each of the two variants that met inclusion criteria (Figure 1), one (rs324419 C >T) was associated with cannabis use (OR [95% CI] 1.9 [1.1, 3.3]; p=0.03) and the other (rs324420 C >A) was associated with self-reported effectiveness (5.2 [1.6, 16.7]; p< 0.01).
Conclusion: Our results indicate that individuals with RA and the genotype CT or TT at rs324419 are twice as likely to use cannabis for arthritis pain management, and cannabis users with RA and the genotype CA or AA at rs324420 have five times greater odds of finding cannabis effective in reducing their pain. FAAH has previously been implicated separately in pain perception, in cannabis use, and in reduction of arthritis severity in mouse models, but this is the first study linking FAAH with cannabis use and real-world pain management in rheumatoid arthritis.
Disclosures: K. Wipfler, None; J. Zeiger, None; T. Simon, Janssen, Bristol-Myers Squibb(BMS); S. Kassan, None; K. Michaud, None.
Background/Purpose: Fatty acid amide hydrolase (FAAH) is a serine hydrolase that breaks down the endocannabinoid/cannabinoid receptor agonist anandamide. Variants in the FAAH gene have been associated with pain susceptibility as well as with cannabis use. In addition, FAAH inhibition has been shown to have anti-arthritic and pain reduction effects in collagen-induced arthritis mouse models. The objective of this study was to examine relationships between FAAH variants and cannabis use as well as real-world effectiveness in pain management for individuals with rheumatoid arthritis (RA).
Methods: Data were provided by adults with RA participating in FORWARD, The National Databank for Rheumatic Diseases, who provided blood samples and answered questions about cannabis use (defined as use of products containing THC and/or CBD). Genotyping was performed with the Illumina Infinium Global Screening Array platform, and non-silent common FAAH variants (minor allele frequency >0.5; SNPs rs324419 and rs324420) were included in this analysis. Logistic regression models for cannabis use vs nonuse and for self-reported effectiveness in pain management (helpful vs not helpful) were generated for each variant by presence or absence of the minor allele. Models were adjusted for age, sex, white race, cigarette smoking history, calendar year, RA duration, BMI, glucocorticoid use, NSAID use, opioid use, and Rheumatic Disease Comorbidity Index (RDCI).
Results: A total of 365 participants met inclusion criteria, 129 (35.3%) of whom reported cannabis use as a treatment for arthritic pain. Among users, 52% reported that cannabis was helpful in reducing their pain, 30% reported that it was not helpful, and 18% reported that they were not sure (Table 1). Genotype distributions of both variants are presented in Table 2. In multivariable models for each of the two variants that met inclusion criteria (Figure 1), one (rs324419 C >T) was associated with cannabis use (OR [95% CI] 1.9 [1.1, 3.3]; p=0.03) and the other (rs324420 C >A) was associated with self-reported effectiveness (5.2 [1.6, 16.7]; p< 0.01).
Conclusion: Our results indicate that individuals with RA and the genotype CT or TT at rs324419 are twice as likely to use cannabis for arthritis pain management, and cannabis users with RA and the genotype CA or AA at rs324420 have five times greater odds of finding cannabis effective in reducing their pain. FAAH has previously been implicated separately in pain perception, in cannabis use, and in reduction of arthritis severity in mouse models, but this is the first study linking FAAH with cannabis use and real-world pain management in rheumatoid arthritis.
Disclosures: K. Wipfler, None; J. Zeiger, None; T. Simon, Janssen, Bristol-Myers Squibb(BMS); S. Kassan, None; K. Michaud, None.

