Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0107: Short-, Intermediate- and Long-Term Renal Outcomes in Hispanics from Puerto Rico with Lupus Nephritis: Induction Therapy with Cyclophosphamide vs. Mycophenolate Mofetil
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SM
Suheiry Marquez, MD
University of Puerto Rico, Medical Science Campus
Trujillo Alto, PR, United States
Abstract Poster Presenter(s)
Suheiry Márquez, Dahima Cintrón and Luis Vilá, University of Puerto Rico Medical Sciences Campus, San Juan, PR
Background/Purpose: The American College of Rheumatology (ACR) guidelines for the treatment of class III and class IV lupus nephritis (LN) recommend induction therapy with mycophenolate mofetil (MMF) over cyclophosphamide (CYC) for Hispanics. These guidelines were derived from studies that mainly included Hispanics from Mexican ancestry. However, it is uncertain if these recommendations can be generalized to all Hispanic populations as there are considerable genetic, sociodemographic, and clinical disparities among Hispanics with lupus. Thus, we sought to determine the short-, intermediate- and long-term renal outcomes among Hispanics from Puerto Rico with LN receiving these treatment modalities.
Methods: A cohort of adult Puerto Ricans with LN was studied. LN was defined as the presence of proteinuria >0.5 g per day, urinary cellular casts, and/or a renal biopsy consistent with LN. Demographic features, clinical manifestations, comorbidities, disease activity (per Systemic Lupus Erythematosus Disease Activity Index ([SLEDAI]), disease damage (per Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index [SDI]), and pharmacologic treatment were gathered at LN onset (baseline). Renal response, chronic kidney disease staging (per National Kidney Foundation), progression to end-stage renal disease (ESRD), and mortality were ascertained at 6 monts,12 months and last study visit. Renal outcomes between patients treated with CYC and MMF were compared using Chi-square test, Fisher's exact test, or Mann-Whitney test, as appropriate.
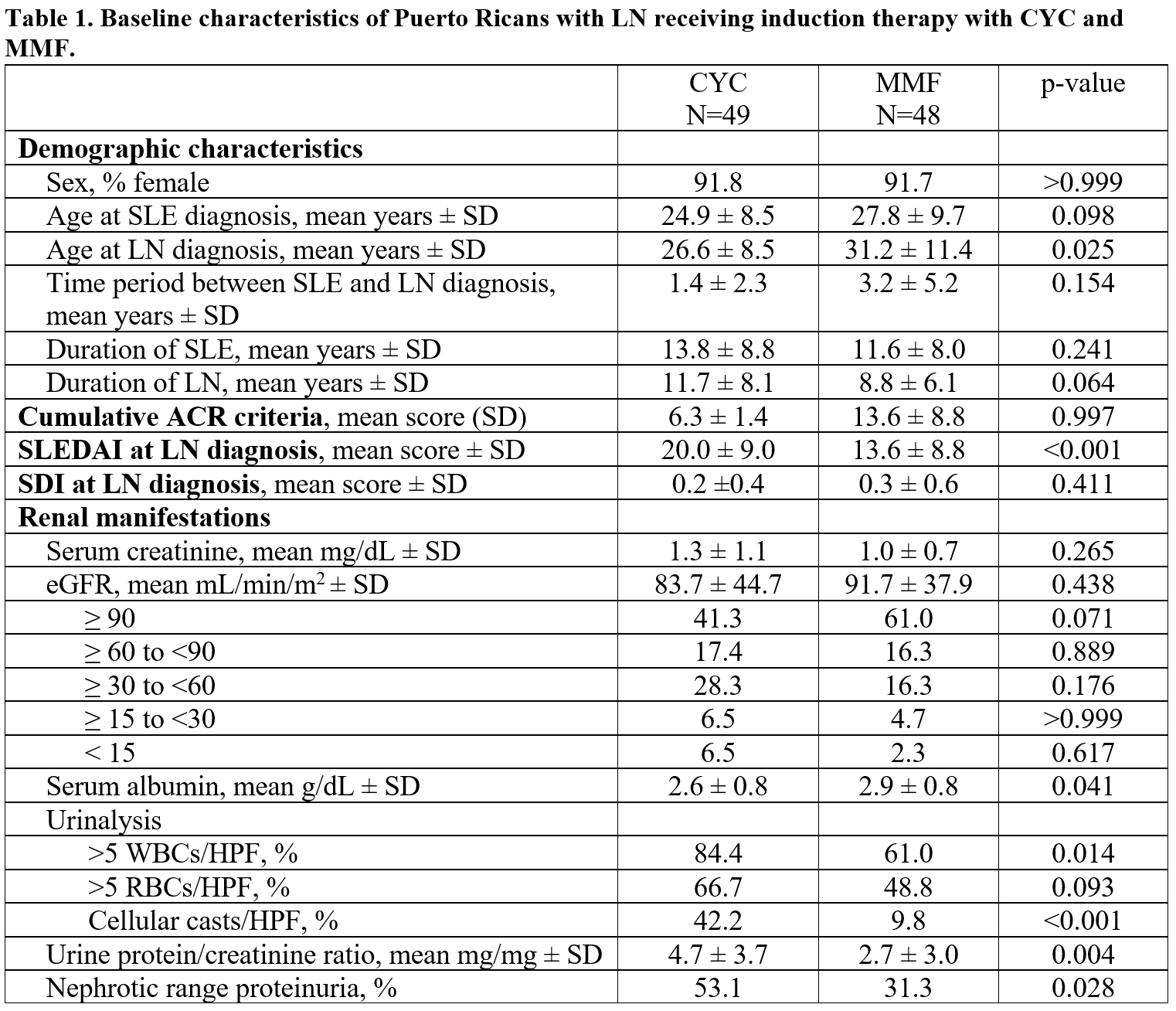
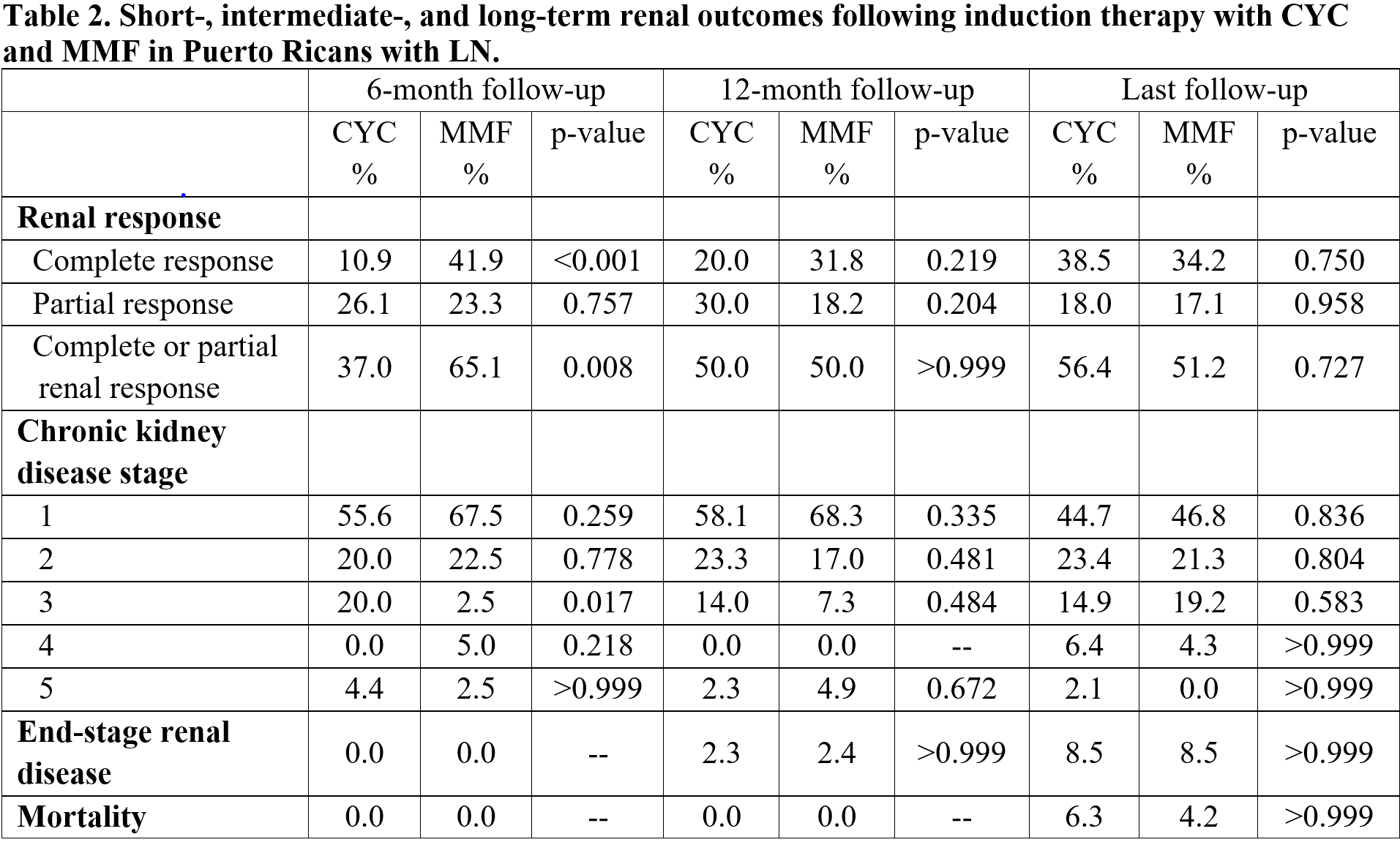
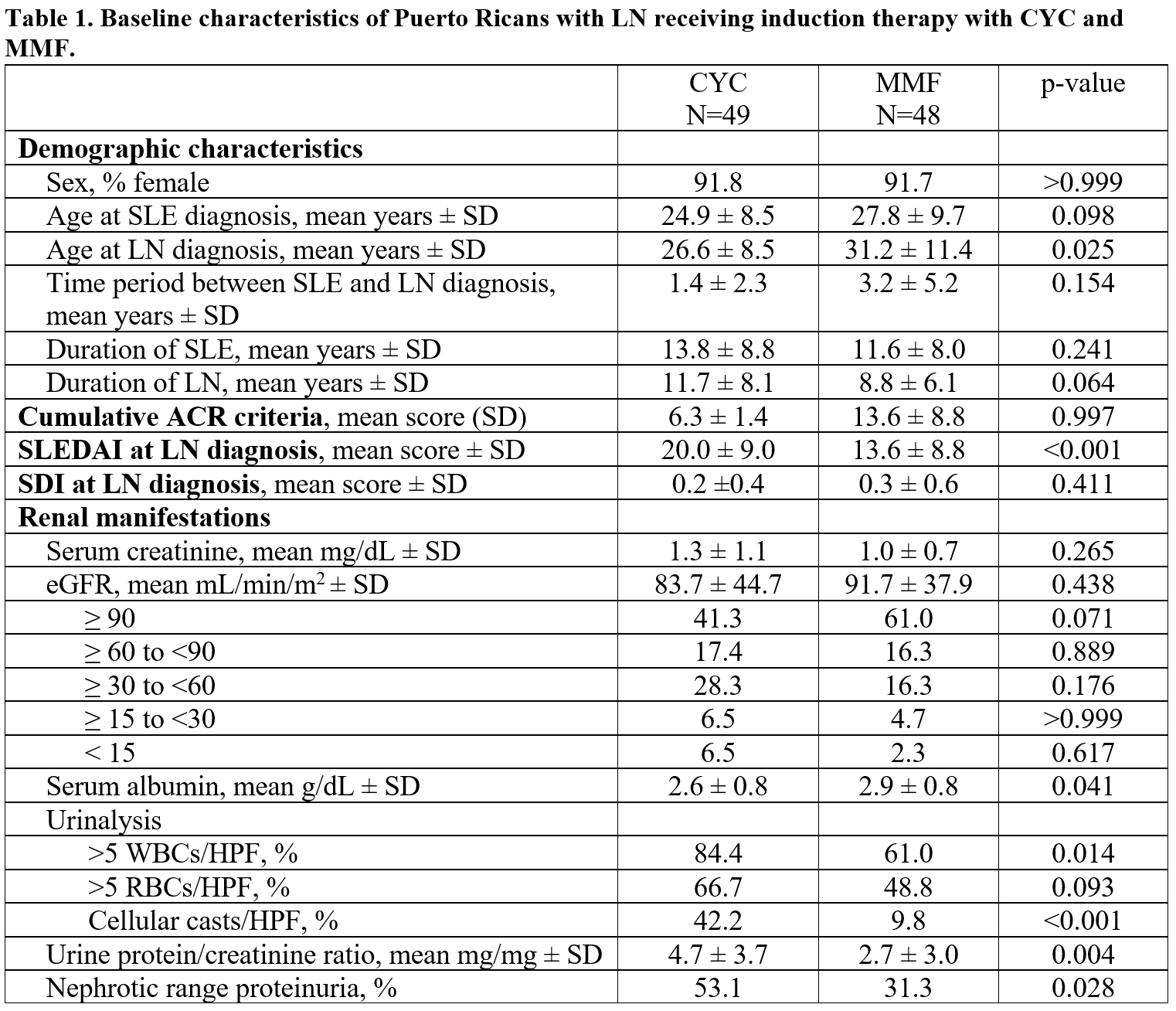
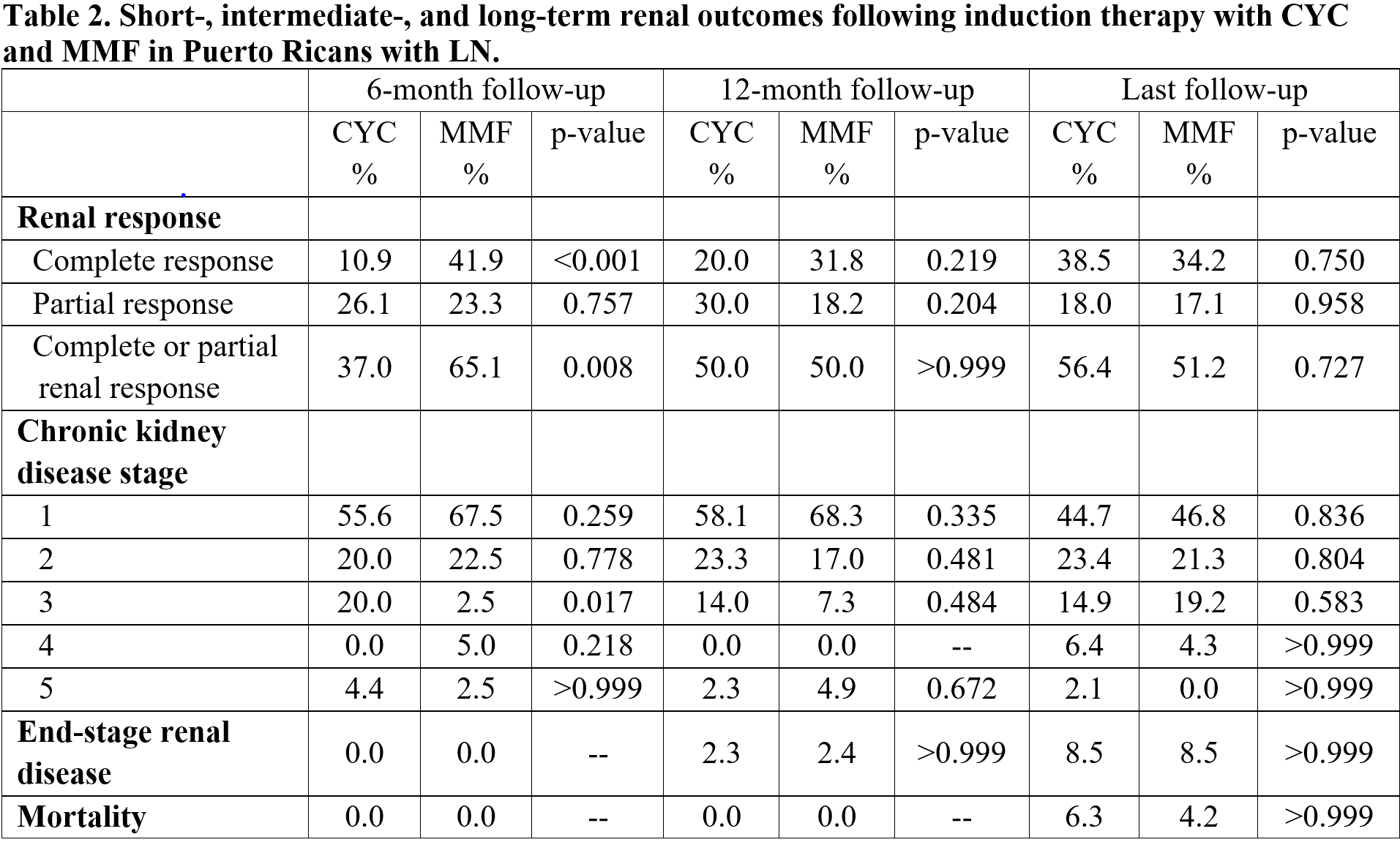
Results: The total LN cohort consisted of 154 patients of which 97 received induction therapy with CYC (n=49) or MMF (n=48). Table 1 shows the baseline features of both treatment groups. Patients treated with CYC had statistically significant higher disease activity, lower albumin levels, and more pyuria and proteinuria than those treated with MMF. Table 2 depicts the renal outcomes at 6 months, 12 months, and last visit. Six-months after induction therapy the overall renal response (complete or partial) was higher in patients treated with MMF compared to CYC. At 12-months and at last visit, no differences were found for all outcome measures. Among patients treated with CYC, 51% of patients were started on MMF after the induction phase. Conversely, in those initially treated with MMF 92% remained on MMF. A sub-analysis in patients with class III and class IV LN showed similar results.
Conclusion: In this group of Puerto Ricans with LN, MMF induction therapy was superior to CYC at 6 months. However, at 12 months and at last study visit, renal outcomes were similar between these treatment groups. Half of patients in the CYC group were started on MMF after CYC therapy. Thus, the intermediate- and long-term efficacy observed for the CYC group could be in part attributed to MMF therapy. Our results are consistent with ACR recommendations favoring MMF over CYC for the induction therapy of LN in Hispanics.
Disclosures: S. Márquez, None; D. Cintrón, None; L. Vilá, None.
Background/Purpose: The American College of Rheumatology (ACR) guidelines for the treatment of class III and class IV lupus nephritis (LN) recommend induction therapy with mycophenolate mofetil (MMF) over cyclophosphamide (CYC) for Hispanics. These guidelines were derived from studies that mainly included Hispanics from Mexican ancestry. However, it is uncertain if these recommendations can be generalized to all Hispanic populations as there are considerable genetic, sociodemographic, and clinical disparities among Hispanics with lupus. Thus, we sought to determine the short-, intermediate- and long-term renal outcomes among Hispanics from Puerto Rico with LN receiving these treatment modalities.
Methods: A cohort of adult Puerto Ricans with LN was studied. LN was defined as the presence of proteinuria >0.5 g per day, urinary cellular casts, and/or a renal biopsy consistent with LN. Demographic features, clinical manifestations, comorbidities, disease activity (per Systemic Lupus Erythematosus Disease Activity Index ([SLEDAI]), disease damage (per Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index [SDI]), and pharmacologic treatment were gathered at LN onset (baseline). Renal response, chronic kidney disease staging (per National Kidney Foundation), progression to end-stage renal disease (ESRD), and mortality were ascertained at 6 monts,12 months and last study visit. Renal outcomes between patients treated with CYC and MMF were compared using Chi-square test, Fisher's exact test, or Mann-Whitney test, as appropriate.
Results: The total LN cohort consisted of 154 patients of which 97 received induction therapy with CYC (n=49) or MMF (n=48). Table 1 shows the baseline features of both treatment groups. Patients treated with CYC had statistically significant higher disease activity, lower albumin levels, and more pyuria and proteinuria than those treated with MMF. Table 2 depicts the renal outcomes at 6 months, 12 months, and last visit. Six-months after induction therapy the overall renal response (complete or partial) was higher in patients treated with MMF compared to CYC. At 12-months and at last visit, no differences were found for all outcome measures. Among patients treated with CYC, 51% of patients were started on MMF after the induction phase. Conversely, in those initially treated with MMF 92% remained on MMF. A sub-analysis in patients with class III and class IV LN showed similar results.
Conclusion: In this group of Puerto Ricans with LN, MMF induction therapy was superior to CYC at 6 months. However, at 12 months and at last study visit, renal outcomes were similar between these treatment groups. Half of patients in the CYC group were started on MMF after CYC therapy. Thus, the intermediate- and long-term efficacy observed for the CYC group could be in part attributed to MMF therapy. Our results are consistent with ACR recommendations favoring MMF over CYC for the induction therapy of LN in Hispanics.
Disclosures: S. Márquez, None; D. Cintrón, None; L. Vilá, None.

