Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0101: Twenty-five Years of Mortality Data in Those with Lower Extremity Osteoarthritis: The Role of Socioeconomic Status
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CM
Cara Murphy, MD
UNC
Chapel Hill, NC, United States
Abstract Poster Presenter(s)
Cara Murphy1, Rebecca Cleveland1, Amanda Nelson2, Yvonne Golightly3 and Leigh Callahan4, 1University of North Carolina, Chapel Hill, NC, 2University of North Carolina at Chapel Hill, Chapel Hill, NC, 3University of Nebraska Medical Center, Omaha, NE, 4University of North Carolina Thurston Arthritis Research Center, Chapel Hill, NC
Background/Purpose: The purpose of this study is to explore the relationship between socioeconomic status (SES) measures (income, professional employment, block group poverty level, education level, and home ownership) and mortality among individuals with lower extremity osteoarthritis (OA).
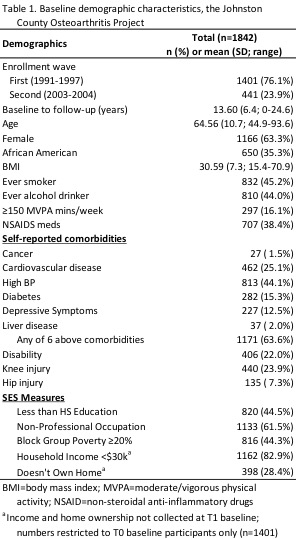
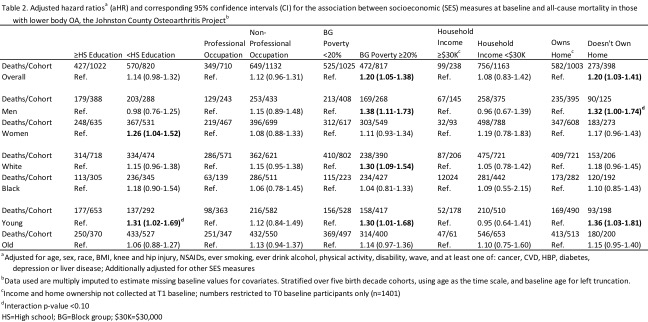
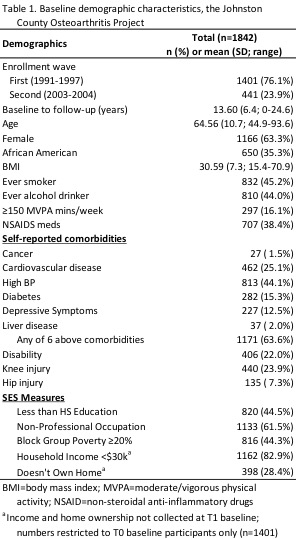
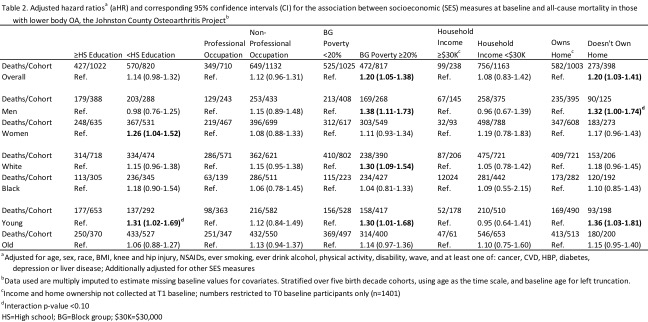
Methods: We analyzed data from 1,842 participants in a cohort of community dwelling Black and White persons aged ≥ 45 years with lower body OA. OA was radiographically confirmed in the hip and/or knee, as defined by a Kellgren-Lawrence grade ≥ 2 in at least one hip/knee joint. We examined baseline SES measures including the individual measures of high school (HS) education (no HS diploma vs. ≥ HS diploma), longest held occupation (non-professional PRO vs PRO occupation), and home ownership (no vs yes), as well as area of residence block group poverty (BGP; ≥ 20% BGP vs < 20%). Multiple imputation was used to impute missing values of covariates. Mortality was determined through 2015, and follow-up time was calculated from baseline until death or censoring which took place when a participant was lost to follow-up or reached the end of the study period. Cox proportional hazards regression was used to estimate adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for all-cause mortality, adjusted for baseline covariates (see Table 2 footnote). Additional analyses included stratification by sex, race, and age.
Results: Mean follow-up time was 13.6 years during which 997 deaths occurred. Baseline demographic characteristics are found in Table 1. Living in an area with BGP ≥ 20% and lack of home ownership were found to independently confer higher hazards of death (aHR=1.20, 95% CI=1.05-1.38; aHR=1.20, 95% CI=1.03-1.14 respectively) (Table 2). Further, in a fully adjusted model, those with < HS education had increased, but not statistically significant, hazard ratios of death (aHR 1.14, 95% CI 0.98-1.32). When stratified by race, sex, and age, additional notable findings were observed. Comparing those with < HS education to those with ≥ HS education, women had a 26% increased hazard of mortality and those < 65 years of age had a 31% increased hazard of mortality. Additionally, increased hazards for mortality were found in stratified analyses for BGP (among men, Whites, and those < 65 years of age) and home ownership (among men and those < 65 years of age) (Table 2).
Conclusion: Previous research has revealed that individual-level and community-level SES measures influence health outcomes. Additionally OA has been associated with increased mortality. To our knowledge, SES measures have not before been directly linked to increased mortality among those with OA. Our study highlights the complex connection between SES and health outcomes, specifically mortality. Results suggest that those with lack of home ownership and those who live in communities with increased poverty may need more intensive guidance from clinicians in addition to certain groups (women and non-elderly) who lack a HS education. People with OA have increased risk of death, as do those with health disparities; thus treatment of OA must consider addressing SES barriers in order to provide successful care especially for high risk patients.
Disclosures: C. Murphy, None; R. Cleveland, None; A. Nelson, None; Y. Golightly, None; L. Callahan, None.
Background/Purpose: The purpose of this study is to explore the relationship between socioeconomic status (SES) measures (income, professional employment, block group poverty level, education level, and home ownership) and mortality among individuals with lower extremity osteoarthritis (OA).
Methods: We analyzed data from 1,842 participants in a cohort of community dwelling Black and White persons aged ≥ 45 years with lower body OA. OA was radiographically confirmed in the hip and/or knee, as defined by a Kellgren-Lawrence grade ≥ 2 in at least one hip/knee joint. We examined baseline SES measures including the individual measures of high school (HS) education (no HS diploma vs. ≥ HS diploma), longest held occupation (non-professional PRO vs PRO occupation), and home ownership (no vs yes), as well as area of residence block group poverty (BGP; ≥ 20% BGP vs < 20%). Multiple imputation was used to impute missing values of covariates. Mortality was determined through 2015, and follow-up time was calculated from baseline until death or censoring which took place when a participant was lost to follow-up or reached the end of the study period. Cox proportional hazards regression was used to estimate adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for all-cause mortality, adjusted for baseline covariates (see Table 2 footnote). Additional analyses included stratification by sex, race, and age.
Results: Mean follow-up time was 13.6 years during which 997 deaths occurred. Baseline demographic characteristics are found in Table 1. Living in an area with BGP ≥ 20% and lack of home ownership were found to independently confer higher hazards of death (aHR=1.20, 95% CI=1.05-1.38; aHR=1.20, 95% CI=1.03-1.14 respectively) (Table 2). Further, in a fully adjusted model, those with < HS education had increased, but not statistically significant, hazard ratios of death (aHR 1.14, 95% CI 0.98-1.32). When stratified by race, sex, and age, additional notable findings were observed. Comparing those with < HS education to those with ≥ HS education, women had a 26% increased hazard of mortality and those < 65 years of age had a 31% increased hazard of mortality. Additionally, increased hazards for mortality were found in stratified analyses for BGP (among men, Whites, and those < 65 years of age) and home ownership (among men and those < 65 years of age) (Table 2).
Conclusion: Previous research has revealed that individual-level and community-level SES measures influence health outcomes. Additionally OA has been associated with increased mortality. To our knowledge, SES measures have not before been directly linked to increased mortality among those with OA. Our study highlights the complex connection between SES and health outcomes, specifically mortality. Results suggest that those with lack of home ownership and those who live in communities with increased poverty may need more intensive guidance from clinicians in addition to certain groups (women and non-elderly) who lack a HS education. People with OA have increased risk of death, as do those with health disparities; thus treatment of OA must consider addressing SES barriers in order to provide successful care especially for high risk patients.
Disclosures: C. Murphy, None; R. Cleveland, None; A. Nelson, None; Y. Golightly, None; L. Callahan, None.

