Back
Poster Session A
Session: (0123–0149) Miscellaneous Rheumatic and Inflammatory Diseases Poster I
0132: Pleuroparenchymal Fibroelastosis: A Special Clinical Situation in Patients with Interstitial Lung Disease Associated with Connective Tissue Diseases. Descriptive Study from a Referral Centre
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BA
Belen Atienza-Mateo, MD, PhD
Hospital Universitario Marqués de Valdecilla
Santander, Cantabria, Spain
Abstract Poster Presenter(s)
Belén Atienza-Mateo1, Sara Remuzgo-Martinez1, Diego Ferrer2, Gerardo Blanco Rodríguez3, Sheila Izquierdo Cuervo2, Víctor M. Mora-Cuesta1, David Iturbe-Fernández1, Ricardo Blanco4, José M. Cifrián1 and Miguel Ángel González-Gay5, 1Research Group on Genetic Epidemiology and Atherosclerosis in Systemic Diseases and in Metabolic Bone Diseases of the Musculoskeletal System, IDIVAL; and Department of Rheumatology, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 2Department of Pneumology, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 3Department of Radiology, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 4Hospital Universitario Marqués de Valdecilla, IDIVAL, Santander, Spain, 5Department of Medicine and Psychiatry, Universidad de Cantabria; Rheumatology Division, Hospital Universitario Marqués de Valdecilla; Research group on genetic epidemiology and atherosclerosis in systemic diseases and in metabolic diseases of the musculoskeletal system, IDIVAL, Santander, Spain. Cardiovascular Pathophysiology and Genomics Research Unit, School of Physiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Background/Purpose: Pleuroparenchymal fibroelastosis (PPFE) is a rare interstitial lung disease (ILD) that can be idiopathic or associated with a variety of different conditions, including connective tissue diseases (CTD) [Ann Am Thorac Soc. 2019 Nov;16(11):1351-1359, Eur Respir J. 2020 Jul 9;56(1):1902135]. In this regard, the presence of PPFE has been reported as an independent predictor of worse prognosis in CTD-ILD patients [Eur Respir J. 2020 Jul 9;56(1):1902135, Rheumatology (Oxford). 2020 Dec 1;59(12):3645-3656]. Consequently, the aim of this study was to determine the prevalence of PPFE in a cohort of Spanish patients with CTD-ILD as well as to compare the characteristics between CTD-ILD patients with and without PPFE.
Methods: A total of 99 patients with CTD-ILD (31 rheumatoid arthritis (RA), 31 systemic sclerosis (SSc), 21 idiopathic inflammatory myositis (IIM), 6 primary Sjögren's syndrome (SS), 4 systemic lupus erythematosus (SLE) and 6 with other CTDs) from the Hospital Universitario Marqués de Valdecilla (Santander, Spain) were included in this study. The presence of PPFE was confirmed by experienced radiologists evaluating chest high-resolution computed tomography images from all patients. In addition, demographic, clinical and radiological characteristics were collected.
Results: The presence of PPFE was found in 9 (9.1%) of the 99 CTD-ILD patients, whereas the remaining 90.9% had no signs of PPFE. In particular, it was confirmed in 4 patients with RA (12.9%), 2 with SSc (6.5%), 1 with IIM (4.8%), 1 with primary SS (16.7%) and 1 with SLE (25.0%) (Figure). The prevalence of bronchial dilation was statistically higher in CTD-ILD patients with PPFE compared to those without PPFE (44.4% versus 6.74%, respectively, p=0.006, Table). There were no significant differences in age at CTD or ILD diagnosis, sex, smoking history, body mass index and pulmonary function tests at ILD diagnosis between both groups (Table).
Conclusion: We provide the prevalence and clinical data of PPFE in patients with CTD-ILD from a national referral centre. Approximately 1 out of 10 of our patients presented associated PPFE, closely correlated to bronchial dilation. The identification of this condition in CTD-ILD patients should be considered routinely since it may worsen their prognosis.
Acknowledgements: Personal funds, SR-M: RD16/0012/0009 (ISCIII-ERDF).
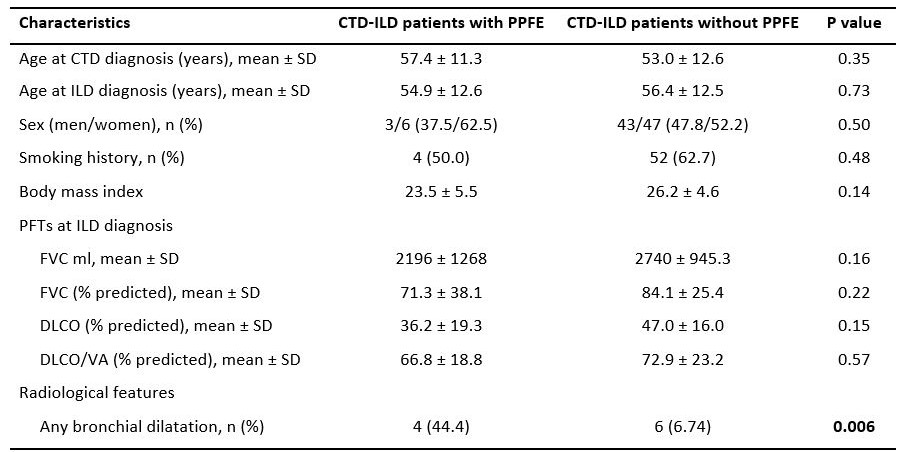 Table. Demographic, clinical and radiological characteristics between CTD-ILD patients with and without PPFE.
Table. Demographic, clinical and radiological characteristics between CTD-ILD patients with and without PPFE.
CTD: connective-tissue disease; DLCO: diffusing capacity of the lung for carbon monoxide; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; ILD: interstitial lung disease; PFTs: pulmonary function tests; PPFE: pleuroparenchymal fibroelastosis; SD: standard deviation; VA: alveolar volume.
Significant results are highlighted in bold.
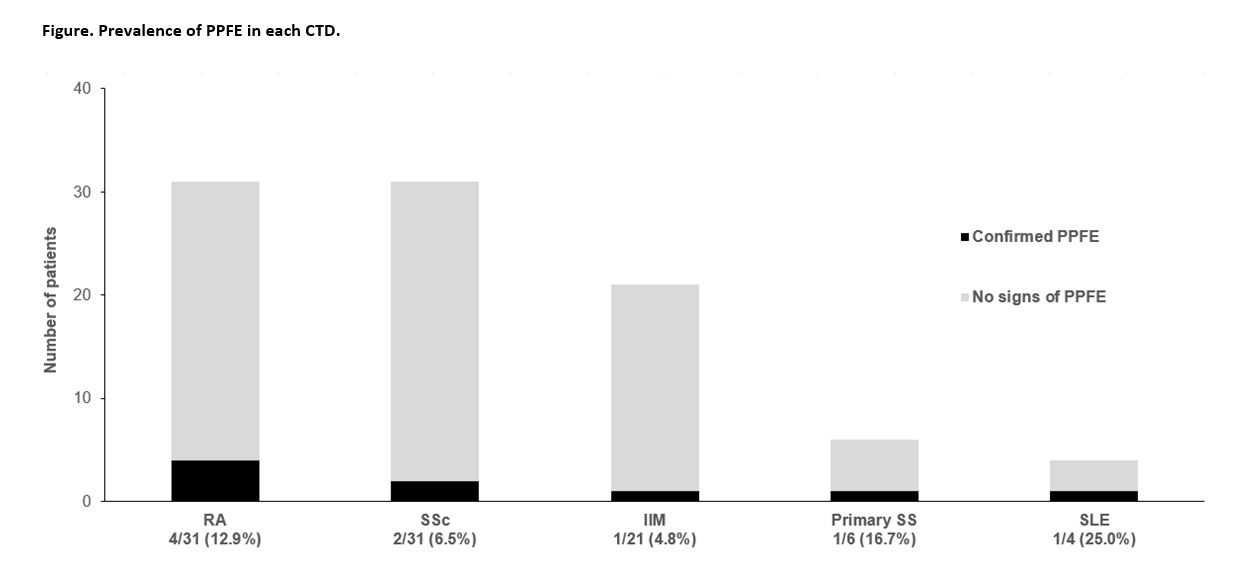 Figure. Prevalence of PPFE in each CTD-ILD.
Figure. Prevalence of PPFE in each CTD-ILD.
Disclosures: B. Atienza-Mateo, AbbVie/Abbott, Roche, Pfizer, Celgene, Novartis, Janssen, UCB, Eli Lilly; S. Remuzgo-Martinez, None; D. Ferrer, None; G. Blanco Rodríguez, None; S. Izquierdo Cuervo, None; V. Mora-Cuesta, None; D. Iturbe-Fernández, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi; J. Cifrián, None; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD.
Background/Purpose: Pleuroparenchymal fibroelastosis (PPFE) is a rare interstitial lung disease (ILD) that can be idiopathic or associated with a variety of different conditions, including connective tissue diseases (CTD) [Ann Am Thorac Soc. 2019 Nov;16(11):1351-1359, Eur Respir J. 2020 Jul 9;56(1):1902135]. In this regard, the presence of PPFE has been reported as an independent predictor of worse prognosis in CTD-ILD patients [Eur Respir J. 2020 Jul 9;56(1):1902135, Rheumatology (Oxford). 2020 Dec 1;59(12):3645-3656]. Consequently, the aim of this study was to determine the prevalence of PPFE in a cohort of Spanish patients with CTD-ILD as well as to compare the characteristics between CTD-ILD patients with and without PPFE.
Methods: A total of 99 patients with CTD-ILD (31 rheumatoid arthritis (RA), 31 systemic sclerosis (SSc), 21 idiopathic inflammatory myositis (IIM), 6 primary Sjögren's syndrome (SS), 4 systemic lupus erythematosus (SLE) and 6 with other CTDs) from the Hospital Universitario Marqués de Valdecilla (Santander, Spain) were included in this study. The presence of PPFE was confirmed by experienced radiologists evaluating chest high-resolution computed tomography images from all patients. In addition, demographic, clinical and radiological characteristics were collected.
Results: The presence of PPFE was found in 9 (9.1%) of the 99 CTD-ILD patients, whereas the remaining 90.9% had no signs of PPFE. In particular, it was confirmed in 4 patients with RA (12.9%), 2 with SSc (6.5%), 1 with IIM (4.8%), 1 with primary SS (16.7%) and 1 with SLE (25.0%) (Figure). The prevalence of bronchial dilation was statistically higher in CTD-ILD patients with PPFE compared to those without PPFE (44.4% versus 6.74%, respectively, p=0.006, Table). There were no significant differences in age at CTD or ILD diagnosis, sex, smoking history, body mass index and pulmonary function tests at ILD diagnosis between both groups (Table).
Conclusion: We provide the prevalence and clinical data of PPFE in patients with CTD-ILD from a national referral centre. Approximately 1 out of 10 of our patients presented associated PPFE, closely correlated to bronchial dilation. The identification of this condition in CTD-ILD patients should be considered routinely since it may worsen their prognosis.
Acknowledgements: Personal funds, SR-M: RD16/0012/0009 (ISCIII-ERDF).
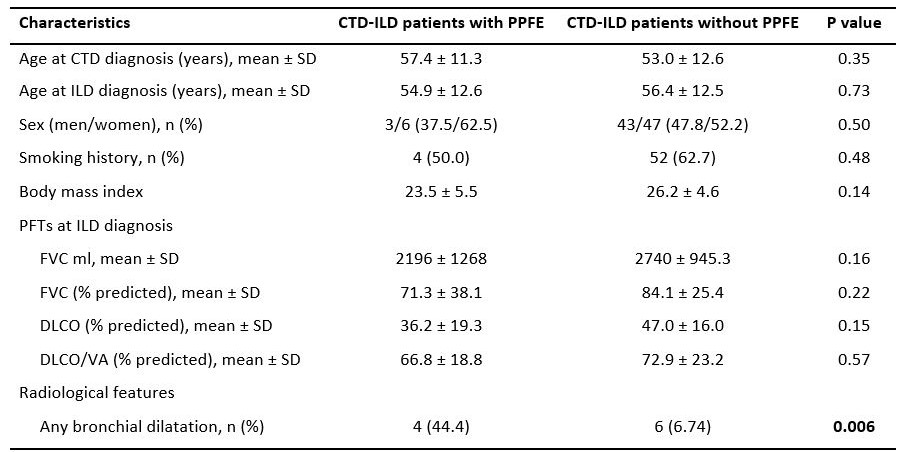 Table. Demographic, clinical and radiological characteristics between CTD-ILD patients with and without PPFE.
Table. Demographic, clinical and radiological characteristics between CTD-ILD patients with and without PPFE. CTD: connective-tissue disease; DLCO: diffusing capacity of the lung for carbon monoxide; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; ILD: interstitial lung disease; PFTs: pulmonary function tests; PPFE: pleuroparenchymal fibroelastosis; SD: standard deviation; VA: alveolar volume.
Significant results are highlighted in bold.
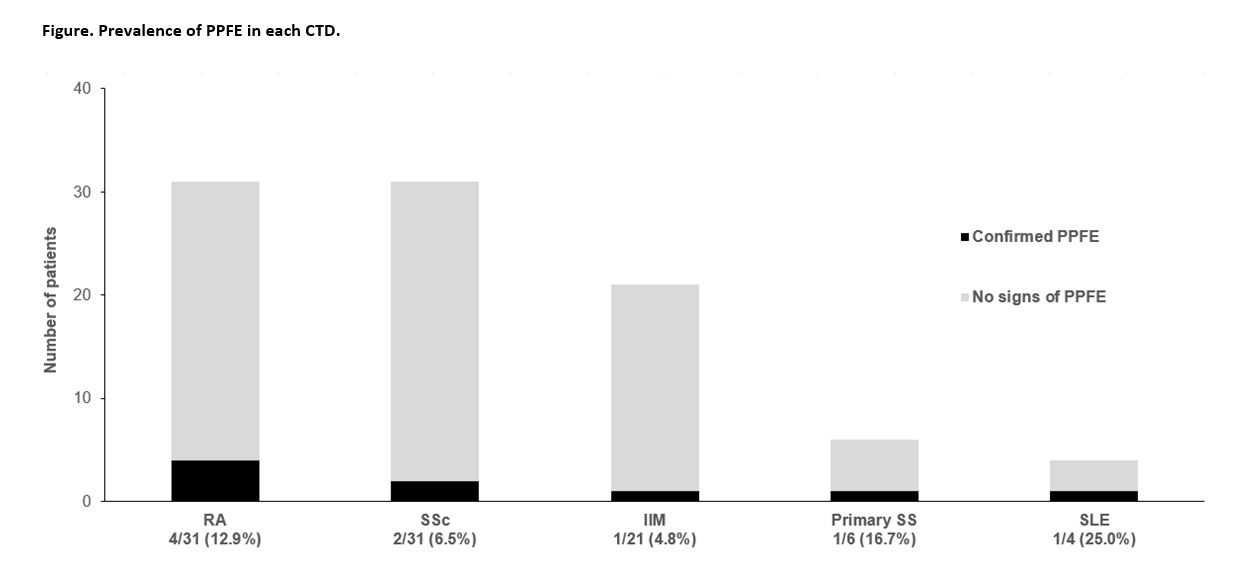 Figure. Prevalence of PPFE in each CTD-ILD.
Figure. Prevalence of PPFE in each CTD-ILD.Disclosures: B. Atienza-Mateo, AbbVie/Abbott, Roche, Pfizer, Celgene, Novartis, Janssen, UCB, Eli Lilly; S. Remuzgo-Martinez, None; D. Ferrer, None; G. Blanco Rodríguez, None; S. Izquierdo Cuervo, None; V. Mora-Cuesta, None; D. Iturbe-Fernández, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi; J. Cifrián, None; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD.

