Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0118: Sex-Based Variations in Emergency Department Utilization by Persons with Inflammatory Arthritis Conditions
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CB
Cheryl Barnabe, MD, FRCPC, MSc
University of Calgary
Calgary, AB, Canada
Abstract Poster Presenter(s)
Cheryl Barnabe1, Patrick McLane2, Nadia Luca1, Katie Lin1, Kelsey Chomistek1, Meghan Elliott1, Shanon McQuitty3, Eileen Davidson3, Clare Hildebrandt4, Steven Katz2, Brian Holroyd2 and Claire Barber1, 1University of Calgary, Calgary, AB, Canada, 2University of Alberta, Edmonton, AB, Canada, 3Arthritis Research Canada, Vancouver, BC, Canada, 4Patient and Family Advisors, Alberta Health Services, Calgary, AB, Canada
Background/Purpose: High quality ambulatory care provision should mitigate avoidable emergency department (ED) visits by persons with inflammatory arthritis (IA) conditions and address the unique realities of those facing inequities in care. Our objective was to characterize ED use by persons with IA conditions based on female or male identity to inform required ambulatory care service enhancements.
Methods: Estimates of ED utilization were obtained from analyzing population-based data from a universal provincial health system in Alberta, Canada (~4.4 million residents). Validated case definitions were applied to physician claims and hospitalization administrative datasets (years 2002-2018) to create prevalent cohorts of persons with Rheumatoid Arthritis (RA), Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), Juvenile Idiopathic Arthritis (JIA) and gout. Records were then linked to the National Ambulatory Care Reporting System dataset in which ED use is documented with details of presentation (timing, acuity, diagnosis, and disposition). Estimates were stratified by binary sex identity for descriptive analysis; annual estimates for years 2008-2018 were generated to identify possible time trends, and data presented here are from fiscal year 2017-2018.
Results: There were 60,373 persons with an IA condition (26,029 female) with 156,570 ED visits (68,910 by females) in the 2017-2018 fiscal year (Table 1). Females with AS and gout were significantly more likely than males to have at least 1 ED visit (difference for AS 7.5%; 95%CI 6.1, 8.9; difference for gout 11.0%; 95%CI 10.3, 11.8). Assigned acuity scores varied by sex with males more frequently assigned '1-resuscitation' and '2-emergent' Canadian Triage & Acuity Scores. For all conditions except JIA, over half of all visits occurred during the day shift (08:00-16:00 hours); females presented at a higher frequency during the evening shift (16:01-22:00 hours) and males during the night shift (22:01-07:59 hours) (p< 0.01). Females with PsA and JIA were significantly more likely than males to present to the ED on a weekday as compared to a weekend or statutory holiday (72.6% vs 68.7%; 71.5% vs 65.0% respectively). The reasons for ED visits were similar between males and females, except for visits for infections being higher in females with JIA (20.1% vs 15.4% of visits), and injuries being higher in males with JIA (31.3% vs 22.6% of visits) (Figure 2). Significantly more males with AS (difference 0.7%; 95%CI 0.2, 1.1) and gout (difference 2.9%; 95%CI 2.7, 3.2) than females with these conditions presented to the ED for a flare, whereas presentations for flares were not different for the other IA conditions. More males with RA returned to the ED within 72 hours of their initial discharge (difference 2.5%; 95%CI 1.2, 3.8). Males with RA, PsA and AS were more frequently admitted to hospital (difference 1.1%, 3.9% and 1.4% respectively, all p< 0.01), whereas females with gout were more frequently admitted (difference 4.0%; 95%CI 3.4, 4.6).
Conclusion: Patterns of ED utilization that vary between females and male persons with different types of IA conditions will need to be recognized in proposed health system solutions aiming to reduce avoidable acute care use.
.jpg) Table 1. Emergency Department Visits by Females and Males with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
Table 1. Emergency Department Visits by Females and Males with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
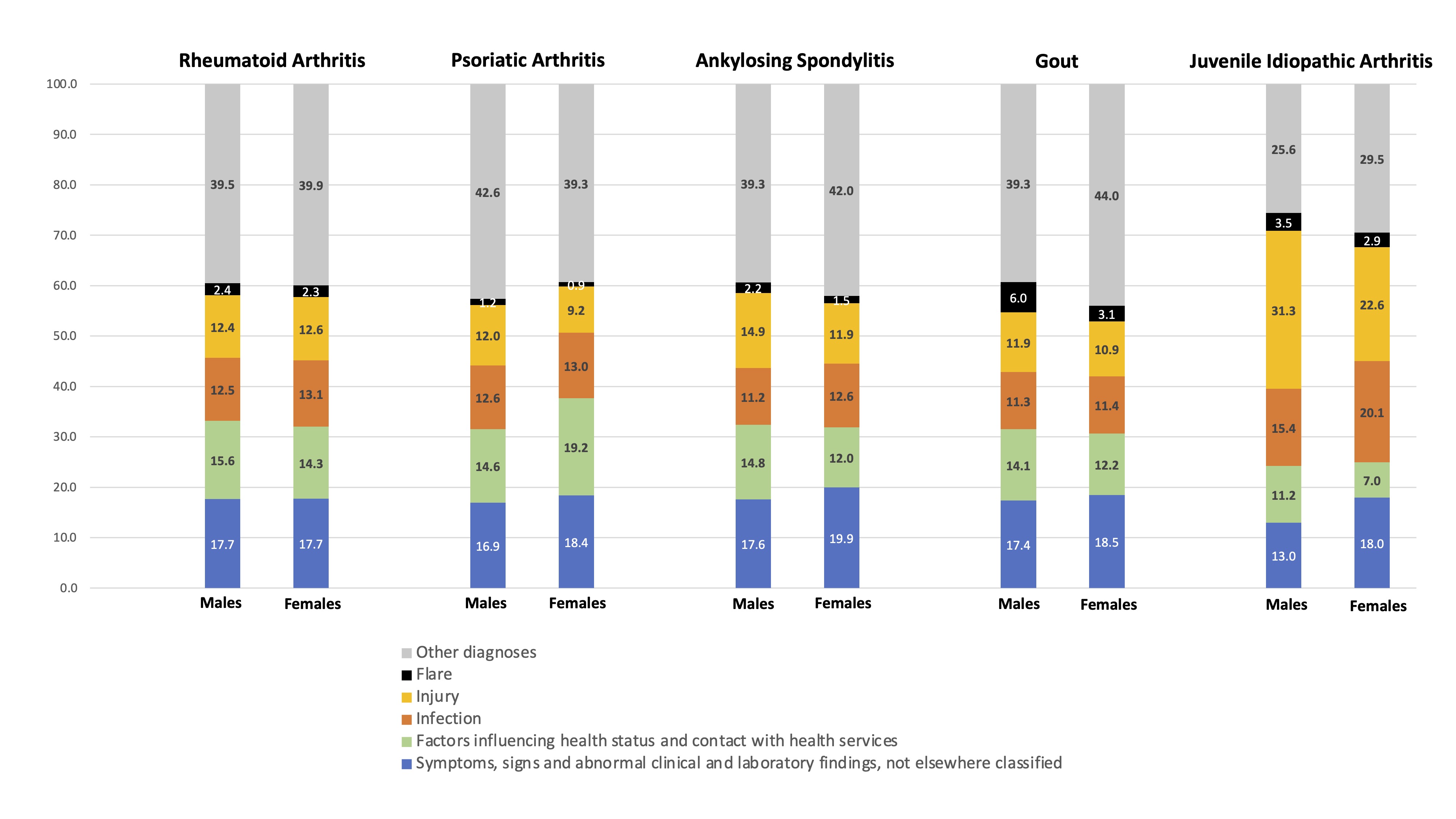 Figure 1. Diagnoses from Emergency Department Use by Males and Females with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Figure 1. Diagnoses from Emergency Department Use by Males and Females with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Disclosures: C. Barnabe, Janssen, Fresenius Kabi, Celltrion Healthcare, Pfizer; P. McLane, None; N. Luca, None; K. Lin, None; K. Chomistek, None; M. Elliott, None; S. McQuitty, None; E. Davidson, None; C. Hildebrandt, None; S. Katz, None; B. Holroyd, None; C. Barber, None.
Background/Purpose: High quality ambulatory care provision should mitigate avoidable emergency department (ED) visits by persons with inflammatory arthritis (IA) conditions and address the unique realities of those facing inequities in care. Our objective was to characterize ED use by persons with IA conditions based on female or male identity to inform required ambulatory care service enhancements.
Methods: Estimates of ED utilization were obtained from analyzing population-based data from a universal provincial health system in Alberta, Canada (~4.4 million residents). Validated case definitions were applied to physician claims and hospitalization administrative datasets (years 2002-2018) to create prevalent cohorts of persons with Rheumatoid Arthritis (RA), Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), Juvenile Idiopathic Arthritis (JIA) and gout. Records were then linked to the National Ambulatory Care Reporting System dataset in which ED use is documented with details of presentation (timing, acuity, diagnosis, and disposition). Estimates were stratified by binary sex identity for descriptive analysis; annual estimates for years 2008-2018 were generated to identify possible time trends, and data presented here are from fiscal year 2017-2018.
Results: There were 60,373 persons with an IA condition (26,029 female) with 156,570 ED visits (68,910 by females) in the 2017-2018 fiscal year (Table 1). Females with AS and gout were significantly more likely than males to have at least 1 ED visit (difference for AS 7.5%; 95%CI 6.1, 8.9; difference for gout 11.0%; 95%CI 10.3, 11.8). Assigned acuity scores varied by sex with males more frequently assigned '1-resuscitation' and '2-emergent' Canadian Triage & Acuity Scores. For all conditions except JIA, over half of all visits occurred during the day shift (08:00-16:00 hours); females presented at a higher frequency during the evening shift (16:01-22:00 hours) and males during the night shift (22:01-07:59 hours) (p< 0.01). Females with PsA and JIA were significantly more likely than males to present to the ED on a weekday as compared to a weekend or statutory holiday (72.6% vs 68.7%; 71.5% vs 65.0% respectively). The reasons for ED visits were similar between males and females, except for visits for infections being higher in females with JIA (20.1% vs 15.4% of visits), and injuries being higher in males with JIA (31.3% vs 22.6% of visits) (Figure 2). Significantly more males with AS (difference 0.7%; 95%CI 0.2, 1.1) and gout (difference 2.9%; 95%CI 2.7, 3.2) than females with these conditions presented to the ED for a flare, whereas presentations for flares were not different for the other IA conditions. More males with RA returned to the ED within 72 hours of their initial discharge (difference 2.5%; 95%CI 1.2, 3.8). Males with RA, PsA and AS were more frequently admitted to hospital (difference 1.1%, 3.9% and 1.4% respectively, all p< 0.01), whereas females with gout were more frequently admitted (difference 4.0%; 95%CI 3.4, 4.6).
Conclusion: Patterns of ED utilization that vary between females and male persons with different types of IA conditions will need to be recognized in proposed health system solutions aiming to reduce avoidable acute care use.
.jpg) Table 1. Emergency Department Visits by Females and Males with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
Table 1. Emergency Department Visits by Females and Males with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)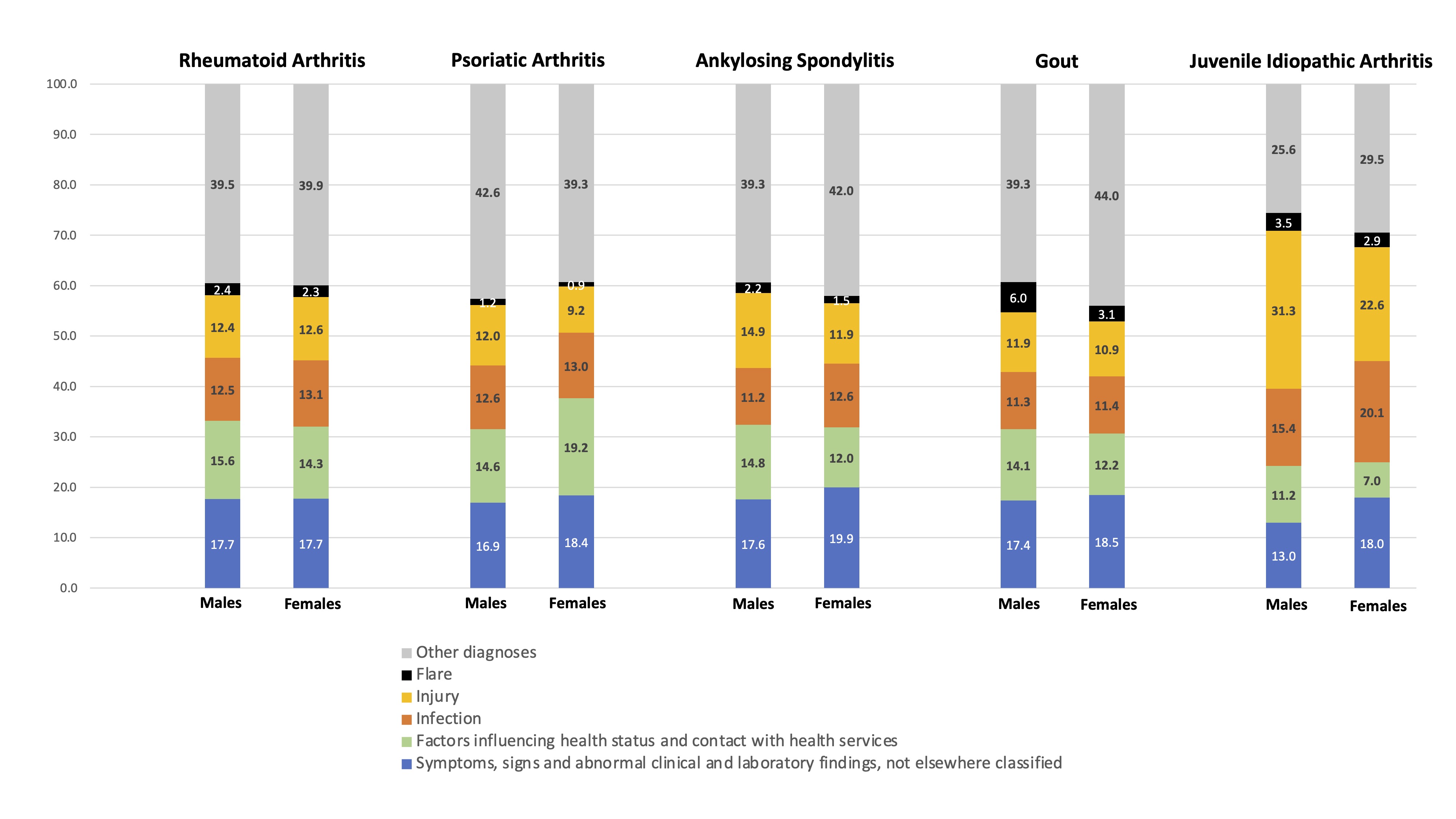 Figure 1. Diagnoses from Emergency Department Use by Males and Females with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Figure 1. Diagnoses from Emergency Department Use by Males and Females with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)Disclosures: C. Barnabe, Janssen, Fresenius Kabi, Celltrion Healthcare, Pfizer; P. McLane, None; N. Luca, None; K. Lin, None; K. Chomistek, None; M. Elliott, None; S. McQuitty, None; E. Davidson, None; C. Hildebrandt, None; S. Katz, None; B. Holroyd, None; C. Barber, None.

