Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0091: Association of Area-Level Heat and Social Vulnerability with Recurrent Hospitalizations Among Individuals with Rheumatic Conditions
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LS
Leah Santacroce, MS
Brigham and Women's Hospital
Boston, MA, United States
Abstract Poster Presenter(s)
Leah Santacroce, Paul Dellaripa, Karen Costenbader, Jamie collins and Candace Feldman, Brigham and Women's Hospital, Boston, MA
Background/Purpose: The neighborhood where a person lives influences health behaviors, access, and outcomes, and contributes to disparities. The relationship between susceptibility to the effects of climate change and acute care utilization among individuals with rheumatic conditions has not been investigated. We examined associations between neighborhood heat and social vulnerability and hospitalizations among individuals with systemic rheumatic conditions, crystalline arthritis, and osteoarthritis.
Methods: Using a Massachusetts (MA) multihospital data repository, we identified individuals ≥18 years with ≥1 ICD-9/10 code for a rheumatic condition who received rheumatology care from 4/1/2018- 4/1/2021 with a valid MA address. We defined the index date as two years before the most recent encounter and the baseline period as one year pre-index date. Addresses were geocoded and linked by census tract to the CDC's Social Vulnerability Index (SVI) and the Metropolitan Area Planning Council's Heat Vulnerability Index (HVI). The SVI includes socioeconomic status, household composition, disability, race, ethnicity, language, housing type and transportation. The HVI includes proximity to hazards (heat), socioeconomic, occupational, health and housing conditions. We used multilevel, multinomial logistic regression models to examine the odds of 1-3 and ≥4 hospitalizations (reference = 0) over two years post index date separately by vulnerability index, adjusting for age, gender, race, ethnicity, insurance, and comorbidities. We used multilevel logistic regression models to examine the odds of ≥2 hospitalizations (vs. < 2) by disease category.
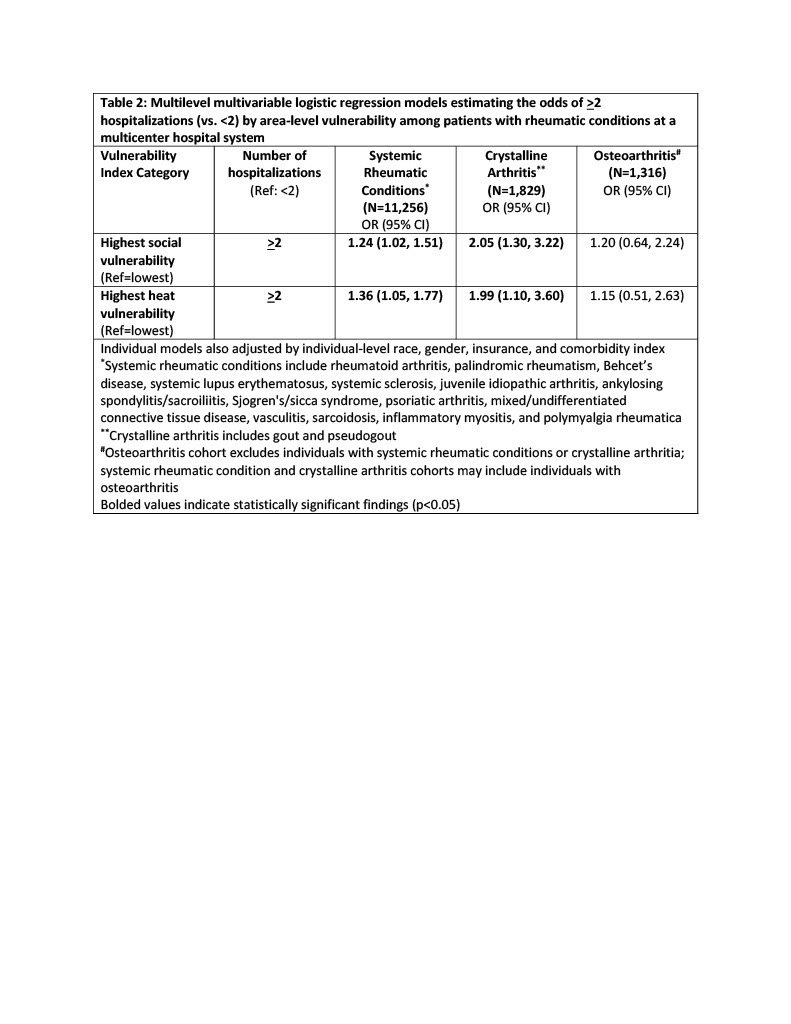
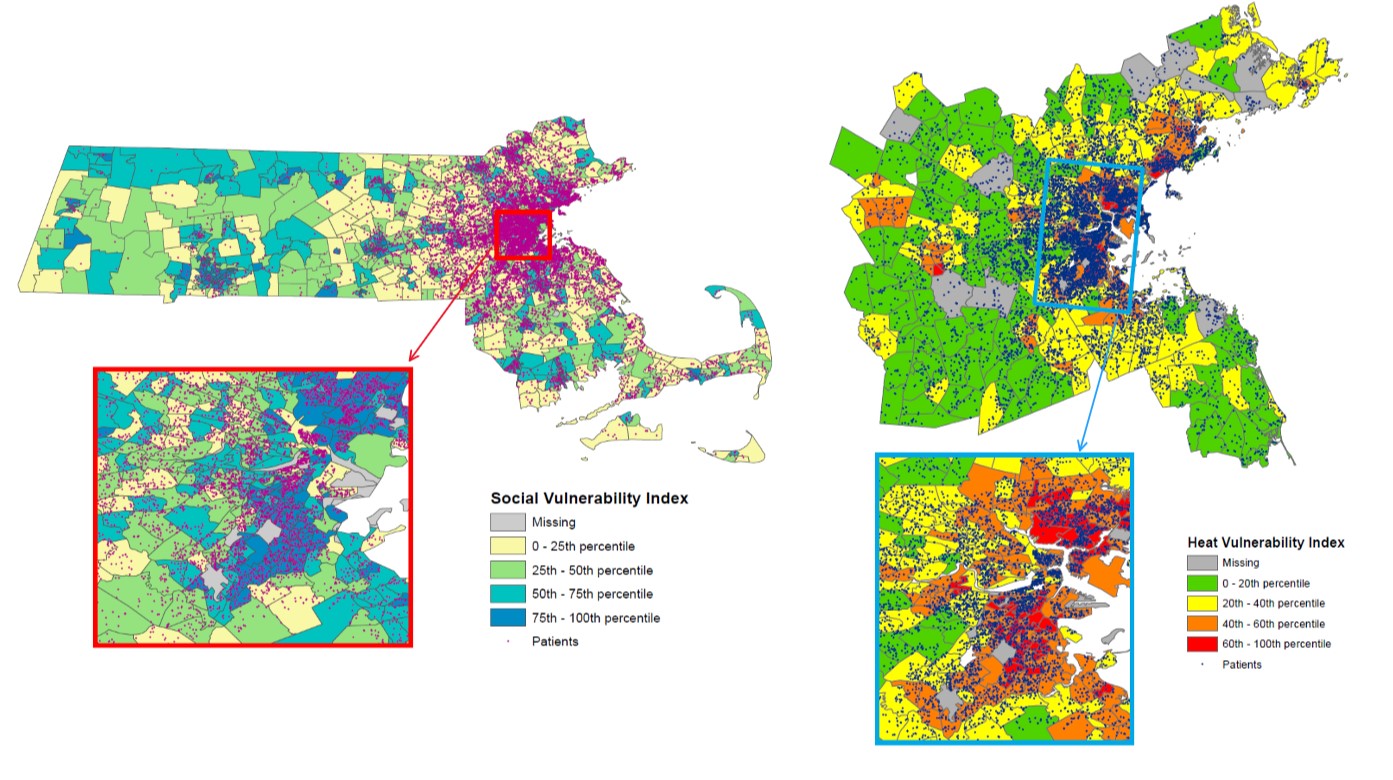
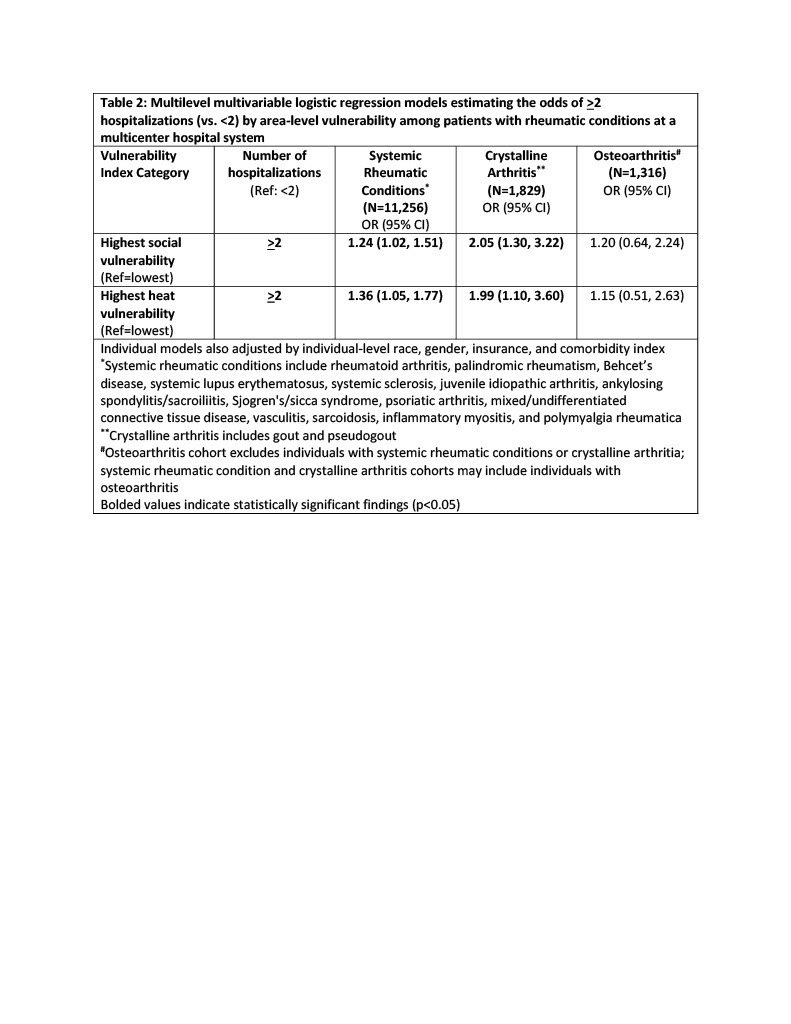
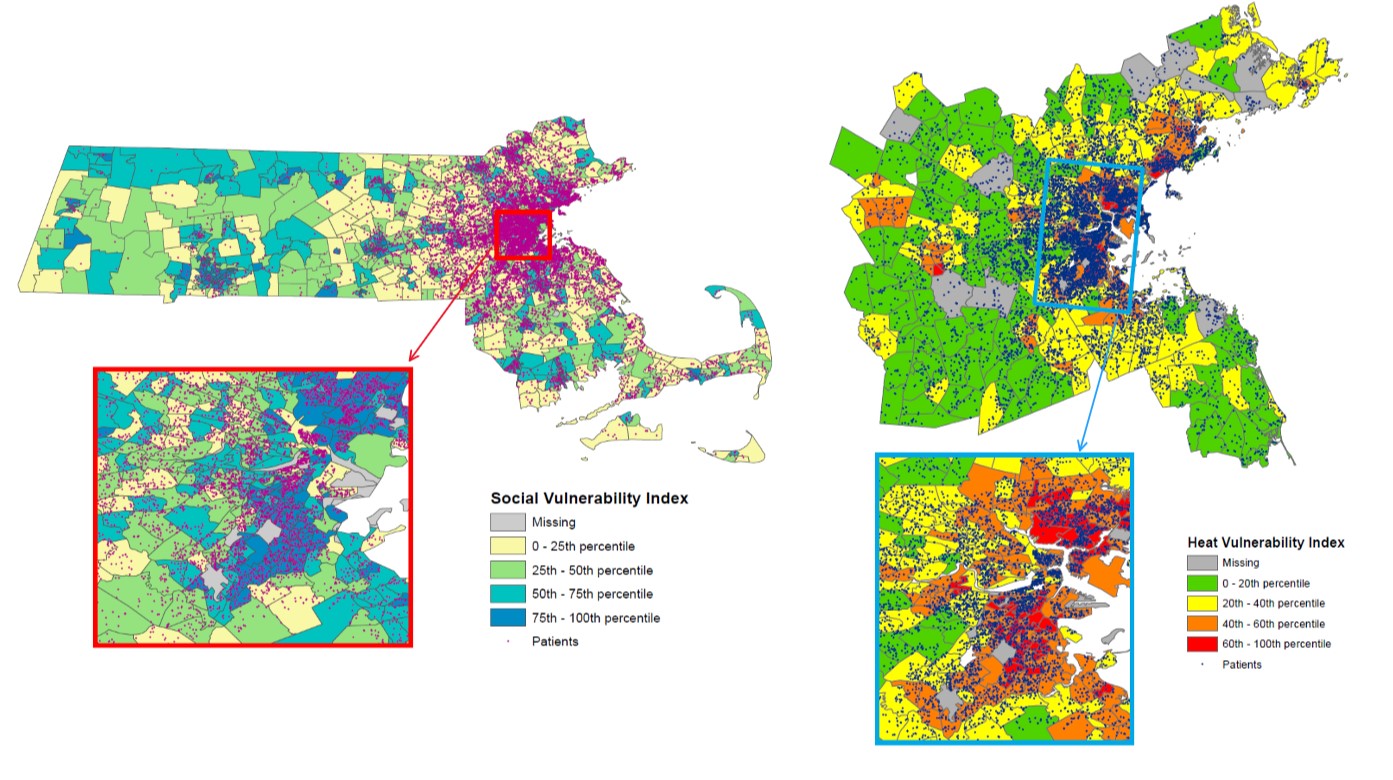
Results: Among 14,401 individuals, 11,256 had codes for a systemic rheumatic condition, 1,829 for crystalline arthritis without a systemic condition, and 1,316 for osteoarthritis without a systemic condition or crystalline arthritis. The mean age was 61.9 (SD 15.7) years, 70% were female, 79% White, 7% Black, and 2% Hispanic. 18.8% lived in the highest SVI areas, 11.7% in the highest HVI areas (Figure 1). There were 8,251 hospitalizations; 689 individuals (5%) had ≥4. Accounting for individual-level factors, individuals living in the highest vs. lowest SVI areas had 1.84 times higher odds (95% CI 1.43-2.36) of ≥4 hospitalizations. Individuals living in the highest vs. lowest HVI areas had 1.64 times greater odds (95% CI 1.17-2.31) of ≥4 hospitalizations (Table 1). Black race, male gender, public insurance, and greater comorbidities were associated with recurrent hospitalizations. Significant associations were seen between area vulnerability and recurrent hospitalizations among individuals with systemic rheumatic conditions and crystalline arthritis. (Table 2).
Conclusion: Individuals with systemic rheumatic conditions and crystalline arthritis living in areas with high vs. low social and heat vulnerability had significantly greater odds of recurrent hospitalizations. Identification of neighborhoods where patients with rheumatic conditions are most susceptible to the adverse effects of climate change is critical to develop adaptive and mitigative strategies in the face of the evolving climate emergency.
.jpg)
Disclosures: L. Santacroce, None; P. Dellaripa, Uptodate, FDA, Genentech, Bristol-Myers Squibb(BMS), Boehringer-Ingelheim; K. Costenbader, Eli Lilly, Janssen, Amgen, AstraZeneca Pharmaceuticals LP, GlaxoSmithKline(GSK), Gilead, Exagen, Neutrolis, Cel-Sci, Alkermes; J. collins, None; C. Feldman, AtlasBio, Pfizer Pharmaceuticals, BMS Foundation, Health Resources in Action, Illumina, Mestag Therapeutics, Elsevier.
Background/Purpose: The neighborhood where a person lives influences health behaviors, access, and outcomes, and contributes to disparities. The relationship between susceptibility to the effects of climate change and acute care utilization among individuals with rheumatic conditions has not been investigated. We examined associations between neighborhood heat and social vulnerability and hospitalizations among individuals with systemic rheumatic conditions, crystalline arthritis, and osteoarthritis.
Methods: Using a Massachusetts (MA) multihospital data repository, we identified individuals ≥18 years with ≥1 ICD-9/10 code for a rheumatic condition who received rheumatology care from 4/1/2018- 4/1/2021 with a valid MA address. We defined the index date as two years before the most recent encounter and the baseline period as one year pre-index date. Addresses were geocoded and linked by census tract to the CDC's Social Vulnerability Index (SVI) and the Metropolitan Area Planning Council's Heat Vulnerability Index (HVI). The SVI includes socioeconomic status, household composition, disability, race, ethnicity, language, housing type and transportation. The HVI includes proximity to hazards (heat), socioeconomic, occupational, health and housing conditions. We used multilevel, multinomial logistic regression models to examine the odds of 1-3 and ≥4 hospitalizations (reference = 0) over two years post index date separately by vulnerability index, adjusting for age, gender, race, ethnicity, insurance, and comorbidities. We used multilevel logistic regression models to examine the odds of ≥2 hospitalizations (vs. < 2) by disease category.
Results: Among 14,401 individuals, 11,256 had codes for a systemic rheumatic condition, 1,829 for crystalline arthritis without a systemic condition, and 1,316 for osteoarthritis without a systemic condition or crystalline arthritis. The mean age was 61.9 (SD 15.7) years, 70% were female, 79% White, 7% Black, and 2% Hispanic. 18.8% lived in the highest SVI areas, 11.7% in the highest HVI areas (Figure 1). There were 8,251 hospitalizations; 689 individuals (5%) had ≥4. Accounting for individual-level factors, individuals living in the highest vs. lowest SVI areas had 1.84 times higher odds (95% CI 1.43-2.36) of ≥4 hospitalizations. Individuals living in the highest vs. lowest HVI areas had 1.64 times greater odds (95% CI 1.17-2.31) of ≥4 hospitalizations (Table 1). Black race, male gender, public insurance, and greater comorbidities were associated with recurrent hospitalizations. Significant associations were seen between area vulnerability and recurrent hospitalizations among individuals with systemic rheumatic conditions and crystalline arthritis. (Table 2).
Conclusion: Individuals with systemic rheumatic conditions and crystalline arthritis living in areas with high vs. low social and heat vulnerability had significantly greater odds of recurrent hospitalizations. Identification of neighborhoods where patients with rheumatic conditions are most susceptible to the adverse effects of climate change is critical to develop adaptive and mitigative strategies in the face of the evolving climate emergency.
.jpg)
Disclosures: L. Santacroce, None; P. Dellaripa, Uptodate, FDA, Genentech, Bristol-Myers Squibb(BMS), Boehringer-Ingelheim; K. Costenbader, Eli Lilly, Janssen, Amgen, AstraZeneca Pharmaceuticals LP, GlaxoSmithKline(GSK), Gilead, Exagen, Neutrolis, Cel-Sci, Alkermes; J. collins, None; C. Feldman, AtlasBio, Pfizer Pharmaceuticals, BMS Foundation, Health Resources in Action, Illumina, Mestag Therapeutics, Elsevier.

