Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0092: Characterizing Levels of Specialist Care Received by Patients with Systemic Lupus Erythematosus: Clinical Characteristics, Emergency Care, Hospitalization, and Costs Among Commercially-insured Adults in the United States
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SW
Sandra Wu, PhD
AstraZeneca
Hockessin, DE, United States
Abstract Poster Presenter(s)
Sandra Sze-jung Wu1, Allison Perry2, Helen Varker3, Christine Dube1 and Gary Bryant4, 1AstraZeneca, Wilmington, DE, 2IBM Watson Health, Cambridge, MA, 3Merative, Cambridge, MA, 4AstraZeneca, New Castle, DE
Background/Purpose: Heterogeneous SLE manifestations can delay referral and diagnosis by a rheumatologist (rheum) in as many as 75% of patients (pts) with SLE.1 After diagnosis, rheum care is expected for the continuum in SLE treatment. Pts with severe organ involvement may also require consultation by a nephrologist (neph), pulmonologist (pulm), or neurologist (neuro). The type of specialist care pts receive is an important part of their SLE disease journey. We aimed to characterize pts with SLE and describe the disease burden associated with levels of specialist consultation in a commercially-insured SLE population.
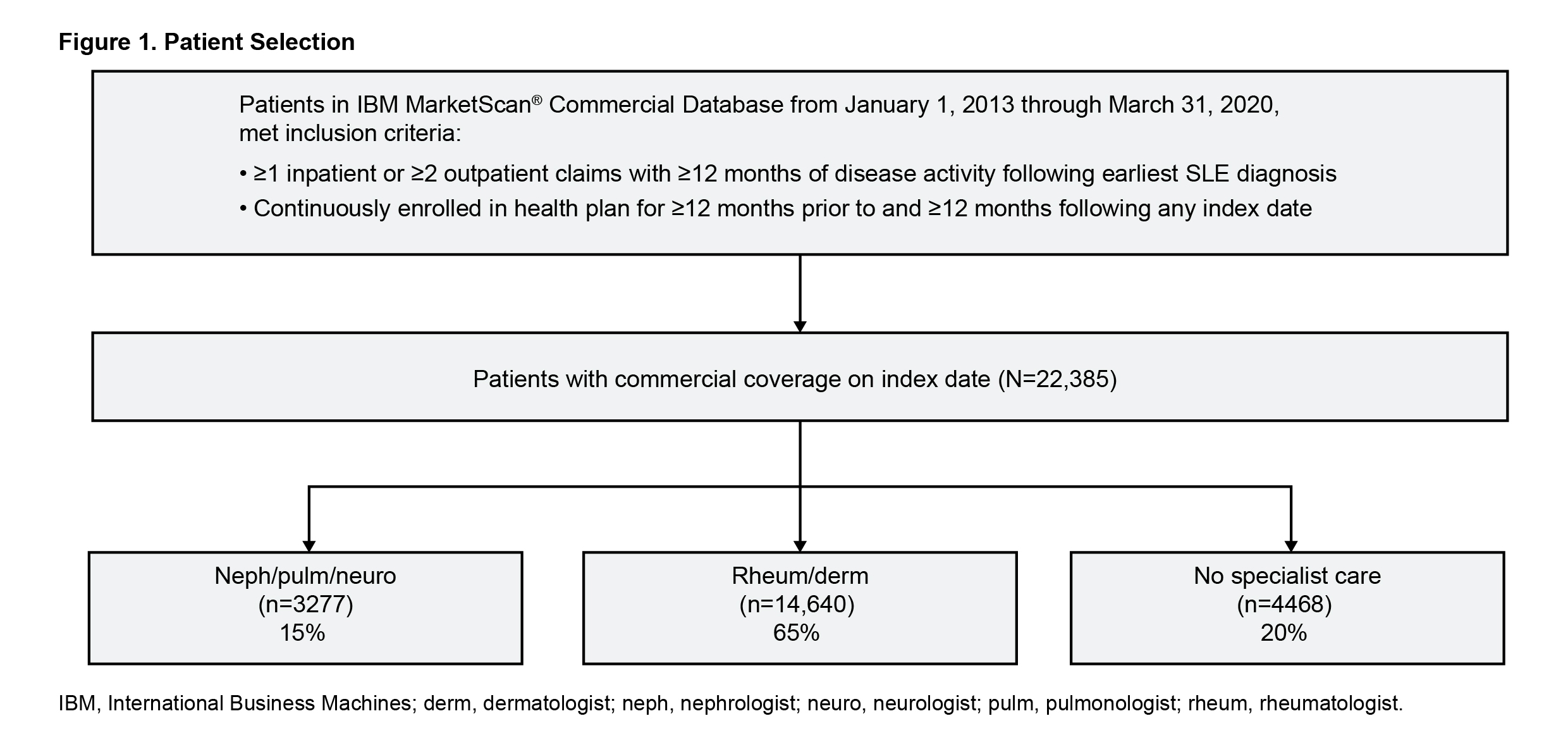
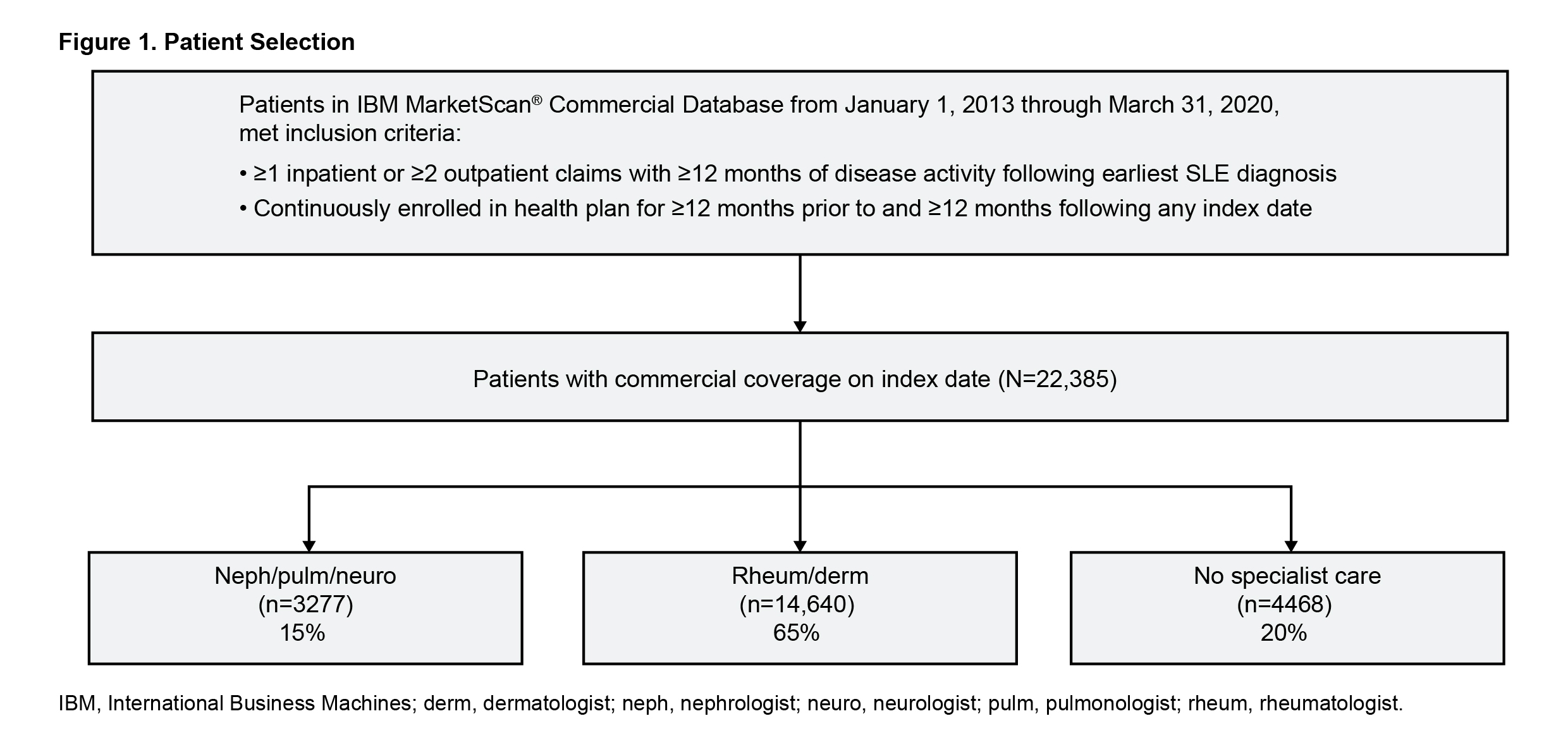
Methods: This retrospective study included pts from the IBM MarketScan Commercial Claims and Encounters database between January 2013–March 2020 with ≥1 inpatient (IP) SLE or ≥2 outpatient claims with ≥12 months of disease activity (Figure 1). Index date was randomized to create a prevalence cohort with ≥12 months prior disease history. Flares were defined using a published claims-based algorithm.2 Demographics, clinical characteristics, and utilization/costs were compared in 3 cohorts of SLE pts based on levels of specialist visits in the baseline year: 1) with neph/pulm/neuro/rheum/dermatologist (derm) care, 2) with rheum/derm care but no neph/pulm/neuro, and 3) no specialist visit.
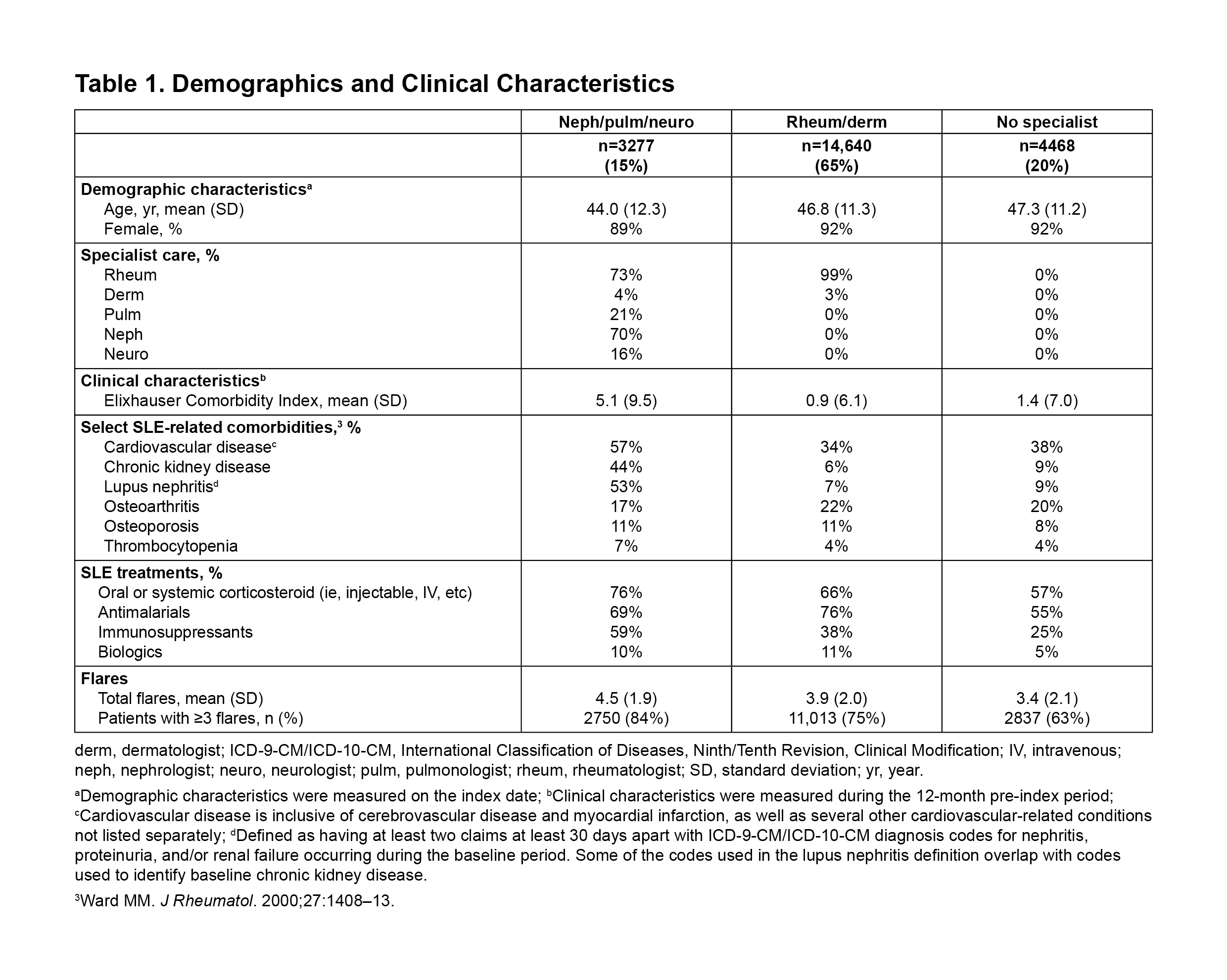
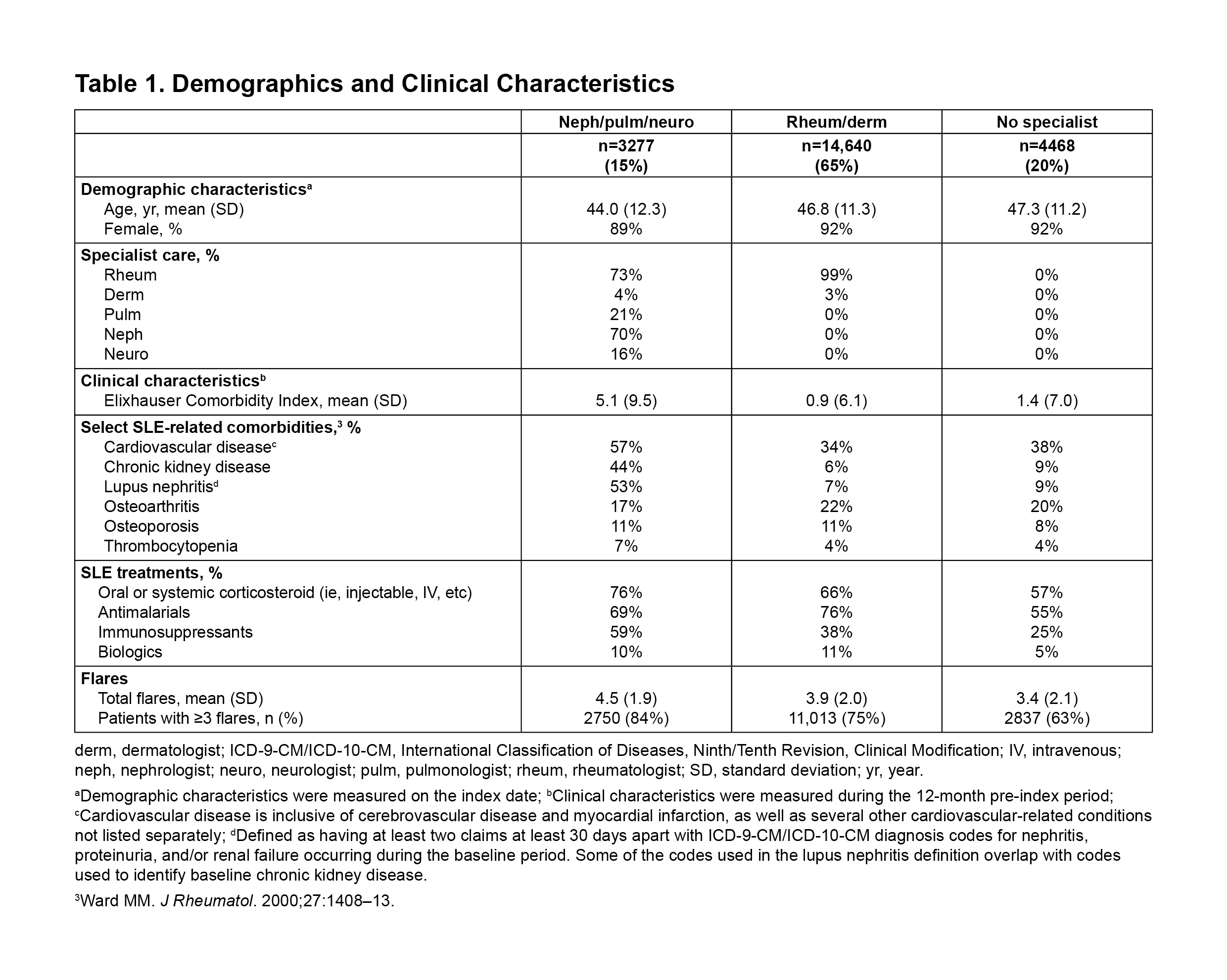
Results: Among 22,385 pts, 15% received neph/pulm/neuro care, 65% rheum/derm care, and 20% received no specialist care during a year (Table 1). Pts with neph/pulm/neuro care were younger than those with rheum/derm care. Mean Elixhauser Comorbidity Index (ECI) was higher in pts with neph/pulm/neuro than those under rheum/derm care. Overall, 84% with neph/pulm/neuro care and 75% with rheum/derm care had ≥3 flares. Pts with neph/pulm/neuro care had higher oral/systemic corticosteroid and immunosuppressant use, lower antimalarial use, and comparable use of biologic therapies, compared with pts receiving rheum/derm care.
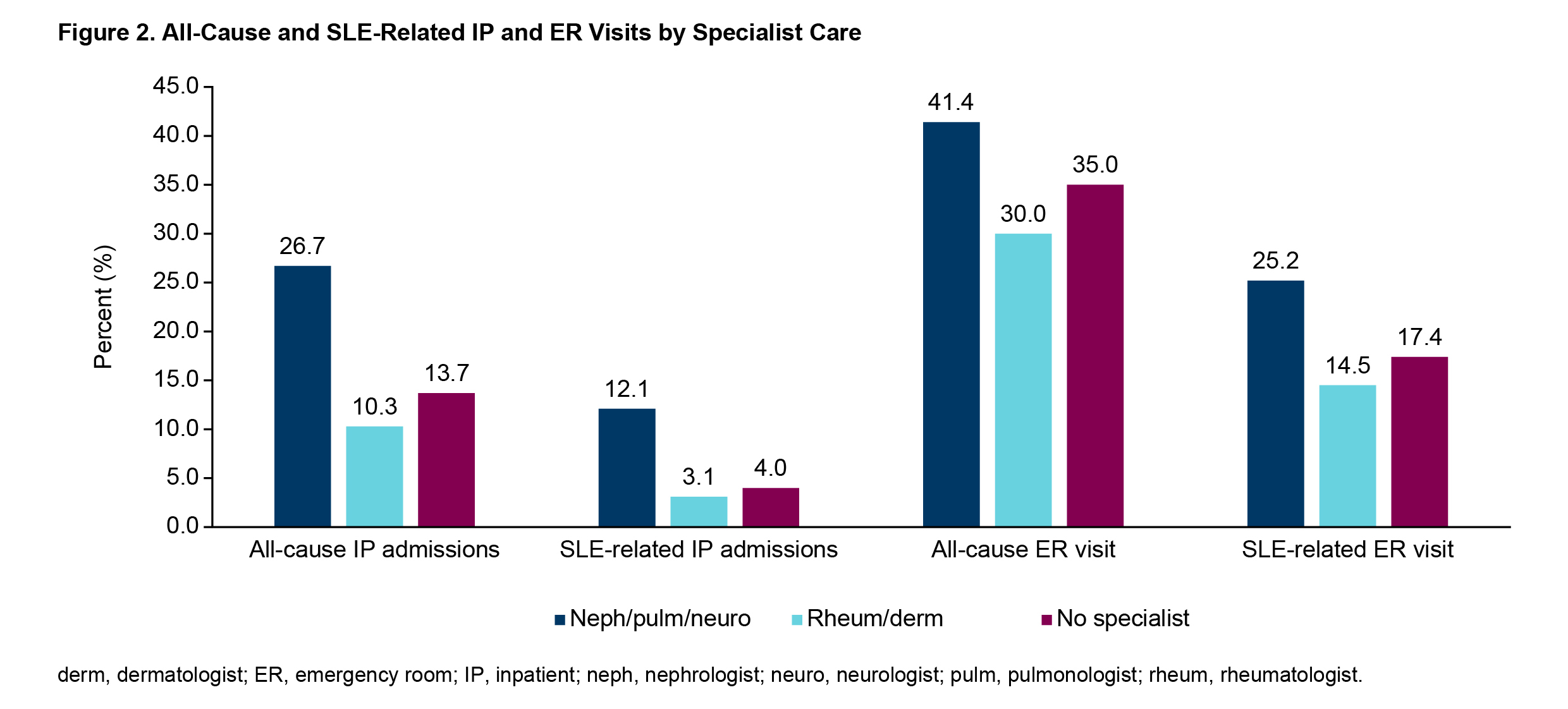
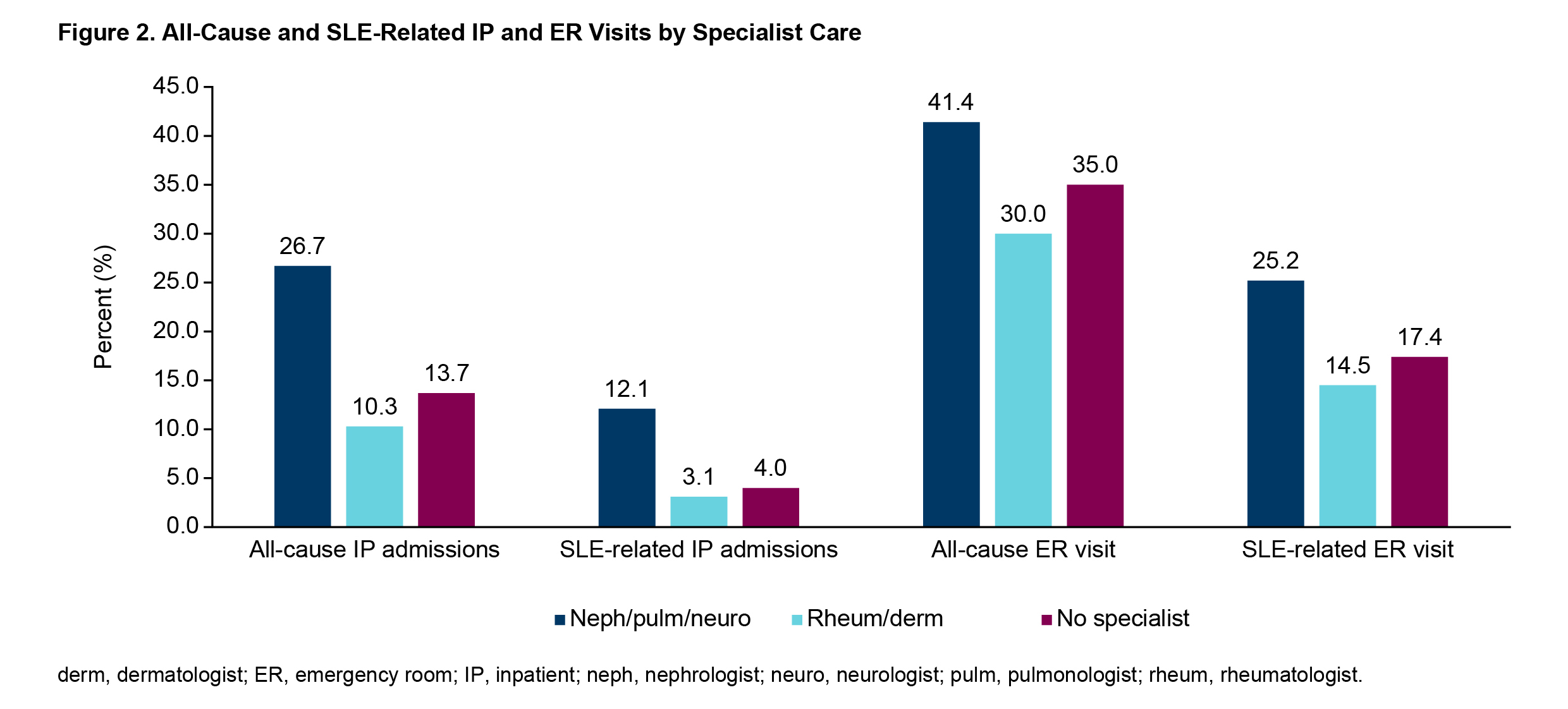
Pts with neph/pulm/neuro care had higher rates of all-cause (27% vs 10%) and SLE-related IP admissions (12% vs 3%) and all-cause (41% vs 30%) and SLE-related emergency room (ER) visits (25% vs 15%), compared with rheum/derm care pts (Figure 2). Mean (SD) all-cause total healthcare costs were higher for pts with neph/pulm/neuro care vs pts with rheum/derm care ($59,003 [139,448] vs $26,660 [63,648]).
Patients in the no-specialist cohort were older and tended to have higher mean (SD) ECI than the rheum/derm cohort (1.4 [7.0] vs 0.9 [6.1]); most continued to receive SLE treatment and had mean 3.4 flares/year (63% had ≥3 flares). The no-specialist cohort had modestly higher SLE-related IP admissions (4% vs 3%), SLE-related ER visits (17% vs 15%), and all-cause healthcare costs than those with rheum/derm care ($29,230 [68,737] vs $26,660 [63,648]).
Conclusion: Among pts with SLE with various organ involvement, this study demonstrated the burden of disease through the proxy of treating specialists. These data also highlighted gaps in care and unmet needs among pts with SLE who lack specialist care despite having multiple flares and high IP/ER utilization.
Reference:
1. Kapsala N. 2022; doi: 10.55563/clinexprheumatol/x3s9td
2. Garris C. J Med Econ. 2013;16:667–77.
Disclosures: S. Sze-jung Wu, AstraZeneca; A. Perry, None; H. Varker, AstraZeneca; C. Dube, AstraZeneca; G. Bryant, AstraZeneca.
Background/Purpose: Heterogeneous SLE manifestations can delay referral and diagnosis by a rheumatologist (rheum) in as many as 75% of patients (pts) with SLE.1 After diagnosis, rheum care is expected for the continuum in SLE treatment. Pts with severe organ involvement may also require consultation by a nephrologist (neph), pulmonologist (pulm), or neurologist (neuro). The type of specialist care pts receive is an important part of their SLE disease journey. We aimed to characterize pts with SLE and describe the disease burden associated with levels of specialist consultation in a commercially-insured SLE population.
Methods: This retrospective study included pts from the IBM MarketScan Commercial Claims and Encounters database between January 2013–March 2020 with ≥1 inpatient (IP) SLE or ≥2 outpatient claims with ≥12 months of disease activity (Figure 1). Index date was randomized to create a prevalence cohort with ≥12 months prior disease history. Flares were defined using a published claims-based algorithm.2 Demographics, clinical characteristics, and utilization/costs were compared in 3 cohorts of SLE pts based on levels of specialist visits in the baseline year: 1) with neph/pulm/neuro/rheum/dermatologist (derm) care, 2) with rheum/derm care but no neph/pulm/neuro, and 3) no specialist visit.
Results: Among 22,385 pts, 15% received neph/pulm/neuro care, 65% rheum/derm care, and 20% received no specialist care during a year (Table 1). Pts with neph/pulm/neuro care were younger than those with rheum/derm care. Mean Elixhauser Comorbidity Index (ECI) was higher in pts with neph/pulm/neuro than those under rheum/derm care. Overall, 84% with neph/pulm/neuro care and 75% with rheum/derm care had ≥3 flares. Pts with neph/pulm/neuro care had higher oral/systemic corticosteroid and immunosuppressant use, lower antimalarial use, and comparable use of biologic therapies, compared with pts receiving rheum/derm care.
Pts with neph/pulm/neuro care had higher rates of all-cause (27% vs 10%) and SLE-related IP admissions (12% vs 3%) and all-cause (41% vs 30%) and SLE-related emergency room (ER) visits (25% vs 15%), compared with rheum/derm care pts (Figure 2). Mean (SD) all-cause total healthcare costs were higher for pts with neph/pulm/neuro care vs pts with rheum/derm care ($59,003 [139,448] vs $26,660 [63,648]).
Patients in the no-specialist cohort were older and tended to have higher mean (SD) ECI than the rheum/derm cohort (1.4 [7.0] vs 0.9 [6.1]); most continued to receive SLE treatment and had mean 3.4 flares/year (63% had ≥3 flares). The no-specialist cohort had modestly higher SLE-related IP admissions (4% vs 3%), SLE-related ER visits (17% vs 15%), and all-cause healthcare costs than those with rheum/derm care ($29,230 [68,737] vs $26,660 [63,648]).
Conclusion: Among pts with SLE with various organ involvement, this study demonstrated the burden of disease through the proxy of treating specialists. These data also highlighted gaps in care and unmet needs among pts with SLE who lack specialist care despite having multiple flares and high IP/ER utilization.
Reference:
1. Kapsala N. 2022; doi: 10.55563/clinexprheumatol/x3s9td
2. Garris C. J Med Econ. 2013;16:667–77.
Disclosures: S. Sze-jung Wu, AstraZeneca; A. Perry, None; H. Varker, AstraZeneca; C. Dube, AstraZeneca; G. Bryant, AstraZeneca.

