Back
Poster Session C
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1518–1542) Systemic Sclerosis and Related Disorders – Clinical Poster II
1535: Frequency of Arrhythmias, Abnormal Electrocardiography and Sudden Cardiac Death in Systemic Sclerosis: A Systematic Review and Meta-analysis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JF
Jessica Fairley, MBBS, FRACP
The University of Melbourne
Melbourne, Victoria, Australia
Abstract Poster Presenter(s)
Jessica Fairley1, Laura Ross2, Alannah Quinlivan3, Dylan Hansen4, Elizabeth Paratz5, Wendy Stevens4, Peter M Kistler6, Andre La Gerche7 and Mandana Nikpour8, 1The University of Melbourne, Melbourne, Australia, 2The University of Melbourne at St. Vincent's Hospital, Brunswick, Australia, 3St Vincent's Hospital Melbourne and the University of Melbourne, Melbourne, Australia, 4St Vincent's Hospital Melbourne, Melbourne, Australia, 5The Baker Institute; St Vincent's Hospital Melbourne, Melbourne, Australia, 6The Baker Heart and Diabetes Institute; The University of Melbourne; Monash University, Melbourne, Australia, 7The Baker Heart and Diabetes Institute; The University of Melbourne, Melbourne, Australia, 8The University of Melbourne at St. Vincent's Hospital Melbourne, Melbourne, Australia
Background/Purpose: Scleroderma (SSc) Heart Involvement (SHI) is an under recognised complication of SSc and may manifest as arrhythmias or sudden cardiac death(SCD). The incidence of SCD in Australia is approximately 35-89 per 100,000 (1) however there is limited data in SSc to date. We sought to determine the incidence of SCD, arrhythmias and conduction abnormalities in SSc.
Methods: We searched MEDLINE and EMBASE to March 2022. English language studies reporting the incidence of SCD, arrhythmias and electrocardiography (ECG) abnormalities in adults with SSc were included. We excluded small case series (< 10 participants), reviews, letters or commentaries. Meta-analysis was performed using Stata 17.0.
Results: Of 1651 potentially relevant records, 79 studies were included involving 12553 individuals. Ten studies included cohorts with diagnosed/suspected SHI, 20 without SHI, and 49 cohorts unselected for SHI. Forty five studies were cross sectional, 30 cohort, 2 case control and 1 case series. Twenty two studies involved a comparator group. All studies were at moderate-high risk of bias. Significant heterogeneity was identified in methodology and outcome.
SCD occurred in 12% of known SHI (n=5 studies, 95%CI 2-22%, I2 90%), 3% of unselected participants (n=5, 95%CI 0-10%, I2 91%) and 7% of those without diagnosed SHI (n=1, 95%CI 2-21%) (Figure 1). Despite this, from limited controlled data, there was no significantly increased prevalence of arrhythmias or ECG abnormalities in SSc (Table 1). This may reflect inherent difficulties in pooling low quality, heterogenous, observational data.
Resting ECGs were abnormal in 69% of those with SHI (n=2, 95% CI 61-78%) and 40-47% of unselected cohorts or those without diagnosed SHI. Non-specific ST-T changes were present in 31% of those with SHI (n=2, 95%CI 19-43%), and 9-15% of those without SHI and unselected cohorts. Conduction block was seen in 14-37% of unselected cohorts or those without SHI (no SHI data).
Non sustained ventricular tachycardia (NSVT) occurred in 18% with SHI (n=4, 95%CI 3-34%, I2 76%), 9% without SHI (n=7, 95%CI 5-12%, I2 41%) and 7% of unselected cohorts (n=10, 95%CI 4-9%, I2 23%) (Figure 2A). Atrial fibrillation (AF) incidence was similar in those with or without SHI. Premature ventricular complexes (PVC) were seen in 67% with SHI (n=1, 95%CI 47-82%), 66% without SHI (n=2, 95%CI 59-74%) and 55% of unselected cohorts (n=5, 95%CI 35-75%, I2 94%) (Figure 2B). Frequent PVC ( >1000/24h) occurred in 70% with SHI (n=1, 95%CI 40-89%) versus 6% without SHI (n=2, 95%CI 0-11%). PVC pairs were more common in those with SHI.
Conclusion: The incidence of SCD in SSc is estimated at 5-12%; substantially higher than the general population. Arrhythmias including NSVT and PVC are common in SSc with and without diagnosed SHI. Identification of risk factors for SCD through imaging and monitoring technologies may help identify patients at risk patients with SSc
1. Wong CX, Brown A, Lau DH et al. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019;28(1):6-14.
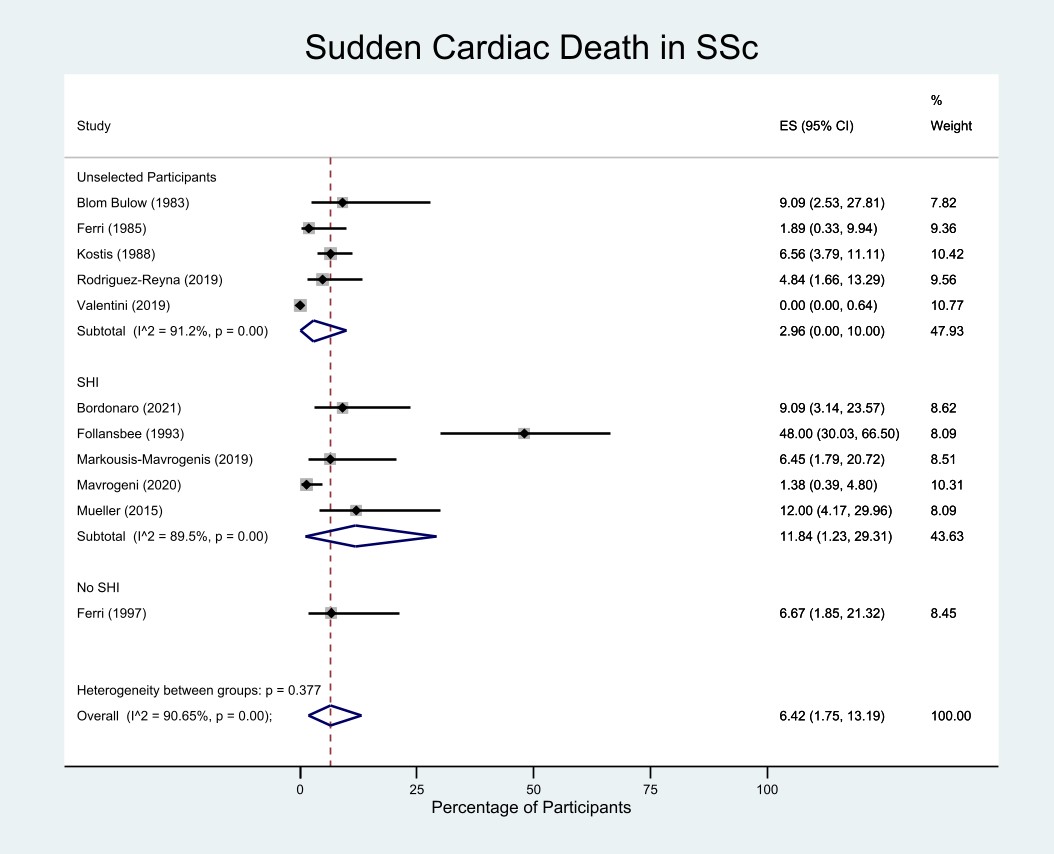 Figure 1: Pooled frequency of sudden cardiac death in SSc.
Figure 1: Pooled frequency of sudden cardiac death in SSc.
Abbreviations: ES - effect size, SHI - systemic sclerosis heart involvement, SSc - systemic sclerosis.
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1289515-2-ANY.jpg width=440 height=681.278976818545 border=0 style=border-style: none;>
.jpg) Figure 2: Prevalence of NSVT and PVC on Holter Monitoring in SSc.
Figure 2: Prevalence of NSVT and PVC on Holter Monitoring in SSc.
Abbreviations: ES - effect size, NSVT - nonsustained ventricular tachycardia, PVC - premature ventricular complex, SHI - systemic sclerosis heart involvement, SSc - systemic sclerosis.
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
Disclosures: J. Fairley, None; L. Ross, None; A. Quinlivan, None; D. Hansen, None; E. Paratz, None; W. Stevens, None; P. Kistler, None; A. La Gerche, None; M. Nikpour, Janssen, AstraZeneca, GlaxoSmithKlein(GSK), Boehringer-Ingelheim, Bristol-Myers Squibb(BMS).
Background/Purpose: Scleroderma (SSc) Heart Involvement (SHI) is an under recognised complication of SSc and may manifest as arrhythmias or sudden cardiac death(SCD). The incidence of SCD in Australia is approximately 35-89 per 100,000 (1) however there is limited data in SSc to date. We sought to determine the incidence of SCD, arrhythmias and conduction abnormalities in SSc.
Methods: We searched MEDLINE and EMBASE to March 2022. English language studies reporting the incidence of SCD, arrhythmias and electrocardiography (ECG) abnormalities in adults with SSc were included. We excluded small case series (< 10 participants), reviews, letters or commentaries. Meta-analysis was performed using Stata 17.0.
Results: Of 1651 potentially relevant records, 79 studies were included involving 12553 individuals. Ten studies included cohorts with diagnosed/suspected SHI, 20 without SHI, and 49 cohorts unselected for SHI. Forty five studies were cross sectional, 30 cohort, 2 case control and 1 case series. Twenty two studies involved a comparator group. All studies were at moderate-high risk of bias. Significant heterogeneity was identified in methodology and outcome.
SCD occurred in 12% of known SHI (n=5 studies, 95%CI 2-22%, I2 90%), 3% of unselected participants (n=5, 95%CI 0-10%, I2 91%) and 7% of those without diagnosed SHI (n=1, 95%CI 2-21%) (Figure 1). Despite this, from limited controlled data, there was no significantly increased prevalence of arrhythmias or ECG abnormalities in SSc (Table 1). This may reflect inherent difficulties in pooling low quality, heterogenous, observational data.
Resting ECGs were abnormal in 69% of those with SHI (n=2, 95% CI 61-78%) and 40-47% of unselected cohorts or those without diagnosed SHI. Non-specific ST-T changes were present in 31% of those with SHI (n=2, 95%CI 19-43%), and 9-15% of those without SHI and unselected cohorts. Conduction block was seen in 14-37% of unselected cohorts or those without SHI (no SHI data).
Non sustained ventricular tachycardia (NSVT) occurred in 18% with SHI (n=4, 95%CI 3-34%, I2 76%), 9% without SHI (n=7, 95%CI 5-12%, I2 41%) and 7% of unselected cohorts (n=10, 95%CI 4-9%, I2 23%) (Figure 2A). Atrial fibrillation (AF) incidence was similar in those with or without SHI. Premature ventricular complexes (PVC) were seen in 67% with SHI (n=1, 95%CI 47-82%), 66% without SHI (n=2, 95%CI 59-74%) and 55% of unselected cohorts (n=5, 95%CI 35-75%, I2 94%) (Figure 2B). Frequent PVC ( >1000/24h) occurred in 70% with SHI (n=1, 95%CI 40-89%) versus 6% without SHI (n=2, 95%CI 0-11%). PVC pairs were more common in those with SHI.
Conclusion: The incidence of SCD in SSc is estimated at 5-12%; substantially higher than the general population. Arrhythmias including NSVT and PVC are common in SSc with and without diagnosed SHI. Identification of risk factors for SCD through imaging and monitoring technologies may help identify patients at risk patients with SSc
1. Wong CX, Brown A, Lau DH et al. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019;28(1):6-14.
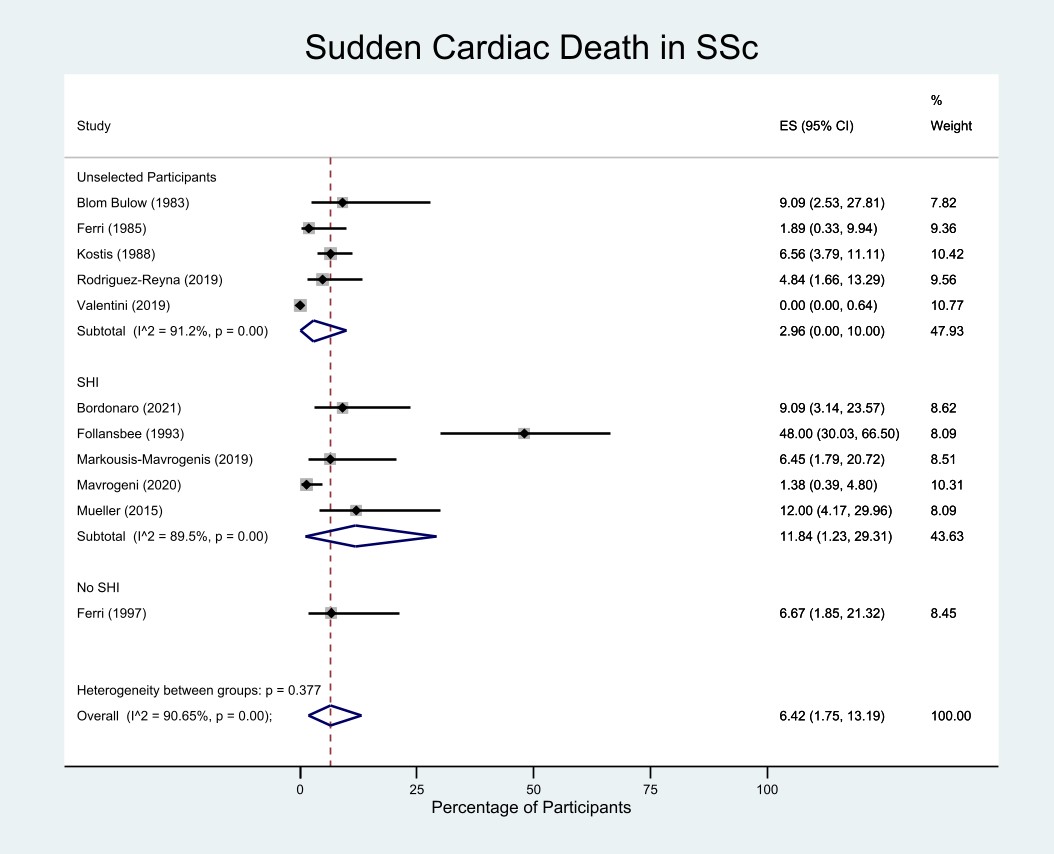 Figure 1: Pooled frequency of sudden cardiac death in SSc.
Figure 1: Pooled frequency of sudden cardiac death in SSc.Abbreviations: ES - effect size, SHI - systemic sclerosis heart involvement, SSc - systemic sclerosis.
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1289515-2-ANY.jpg width=440 height=681.278976818545 border=0 style=border-style: none;>
Table 1: Pooled Prevalence of each outcome, by subgroup
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
Unselected participants refers to a group with SSc who were not selected as having SHI (definite or suspected) or other relevant cardiac signs or symptoms, or as not having SHI, or where S
*I2 values on able to be calculated where >3 studies available to pool.
Abbreviations: AF – atrial fibrillation; CI – confidence interval; ECG – electrocardiography; LBBB – left bundle branch block; NOS – not otherwise specified; NSVT – nonsustained ventricular tachycardia; PAC – premature atrial complexes; PVC – premature ventricular complexes; RBBB – right bundle branch block; SSc – systemic sclerosis; SVT – supraventricular tachycardia.
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
Unselected participants refers to a group with SSc who were not selected as having SHI (definite or suspected) or other relevant cardiac signs or symptoms, or as not having SHI, or where S
*I2 values on able to be calculated where >3 studies available to pool.
Abbreviations: AF – atrial fibrillation; CI – confidence interval; ECG – electrocardiography; LBBB – left bundle branch block; NOS – not otherwise specified; NSVT – nonsustained ventricular tachycardia; PAC – premature atrial complexes; PVC – premature ventricular complexes; RBBB – right bundle branch block; SSc – systemic sclerosis; SVT – supraventricular tachycardia.
.jpg) Figure 2: Prevalence of NSVT and PVC on Holter Monitoring in SSc.
Figure 2: Prevalence of NSVT and PVC on Holter Monitoring in SSc.Abbreviations: ES - effect size, NSVT - nonsustained ventricular tachycardia, PVC - premature ventricular complex, SHI - systemic sclerosis heart involvement, SSc - systemic sclerosis.
NB: "SHI" refers to participants selected as having definite/suspected SHI including abnormal cardiac investigations, arrhythmias, or cardiac symptoms/signs. "No SHI" refers to participants selected as not having any features of SHI. "Unselected" participants refers to cohorts where SHI status was not specified or there were a mixture of participants with/without abnormal cardiac investigations/symptoms/signs.
Disclosures: J. Fairley, None; L. Ross, None; A. Quinlivan, None; D. Hansen, None; E. Paratz, None; W. Stevens, None; P. Kistler, None; A. La Gerche, None; M. Nikpour, Janssen, AstraZeneca, GlaxoSmithKlein(GSK), Boehringer-Ingelheim, Bristol-Myers Squibb(BMS).

