Back
Poster Session C
Rheumatoid arthritis (RA)
Session: (1387–1416) RA – Diagnosis, Manifestations, and Outcomes Poster III
1409: Impact of a Hybrid Medical Care Model in the Rheumatoid Arthritis Patient-Reported Outcomes: A Non-inferiority Crossover Randomized Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GG
Guillermo Guaracha Basañez, MD
Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán"
Mexico city, Federal District, Mexico
Abstract Poster Presenter(s)
Guillermo Guaracha Basañez1, Irazu Contreras-Yáñez2, Vivian Estrada-González2, Lexli Pacheco-Santiago2, Salvador Valverde-Hernández2 and Virginia Pascual Ramos3, 1Instituto Nacional de Ciencias Médicas y Nutrición \"Salvador Zubirn\", Ciudad de México, Mexico, 2Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Ciudad de México, Mexico, 3Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Ciudad de México, Mexico
Background/Purpose: Patients and physicians can naturally adopt hybrid healthcare models (HC), that combine face-to-face consultations (FFC) with telemedicine. The study's objective was to compare the impact of two healthcare interventions, HC and FFC, on the patient-reported outcomes (PROs) of RA patients, during the current COVID-19 pandemic.
Methods: Consecutive patients reincorporated to an outpatient clinic previously lockdown, were invited to a non-inferiority, crossover, and randomized study (October 2020-May 2022). Patients were randomized to six months of FFC or HC (intervention period-1) and then the converse modality (intervention period-2). Intervention period-1 was followed by two months "washout period". The six months of FFC consisted of three to four consecutive standardized medical evaluations. The six months of HC consisted of three to four consecutive standardized medical evaluations, starting with a video conference consultation, and alternating with FFC, the period considered at least two video conference consultations. The primary outcome was disease activity/severity behavior (RAPID3). Additional PROs were disability (HAQ-DI), quality-of-life (WHOQOL-BREF), adherence to medical care, satisfaction with medical care, and treatment recommendations. Sample size calculation established 55 patients/healthcare intervention. To summarize PROs' behavior during the study, Areas Under the Curve (AUC) were calculated.
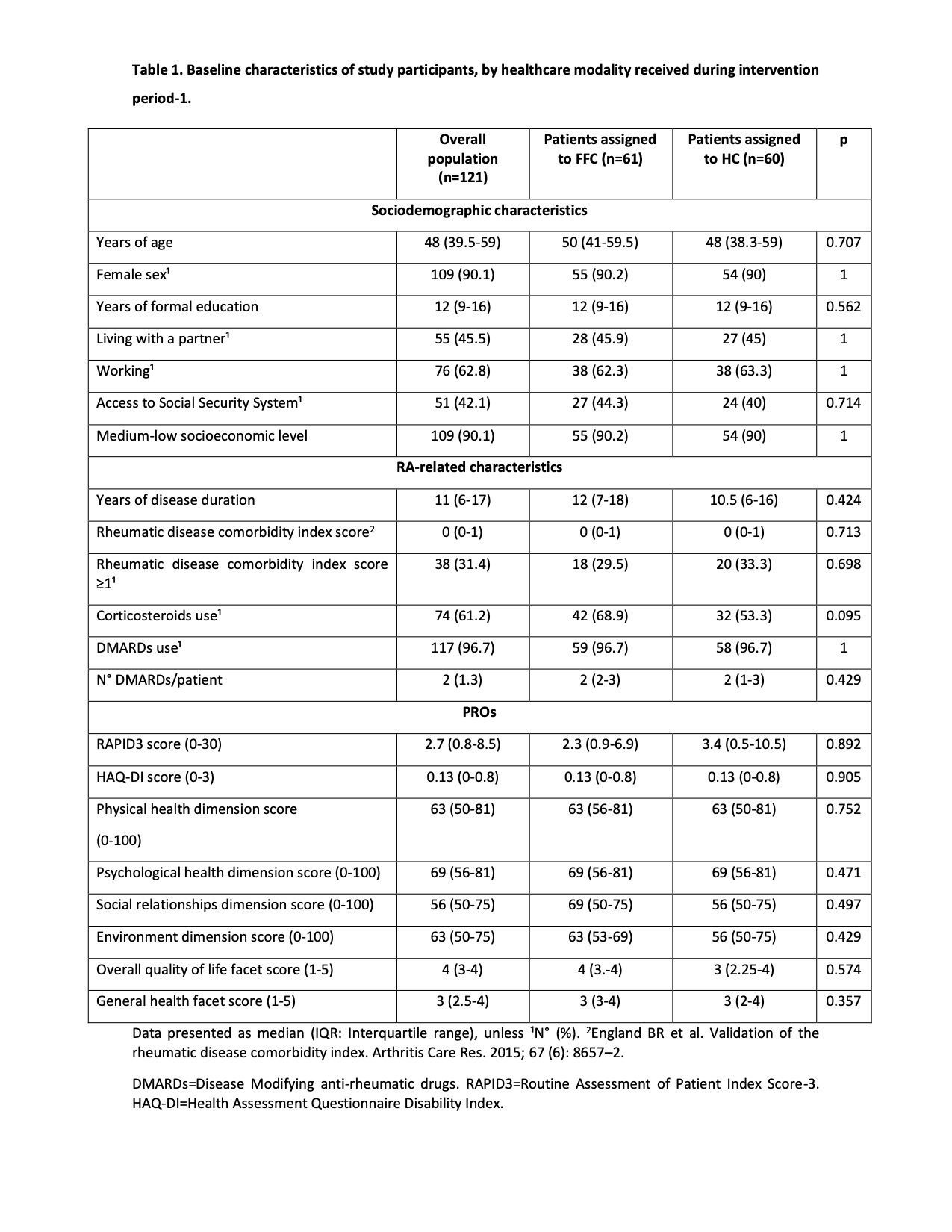
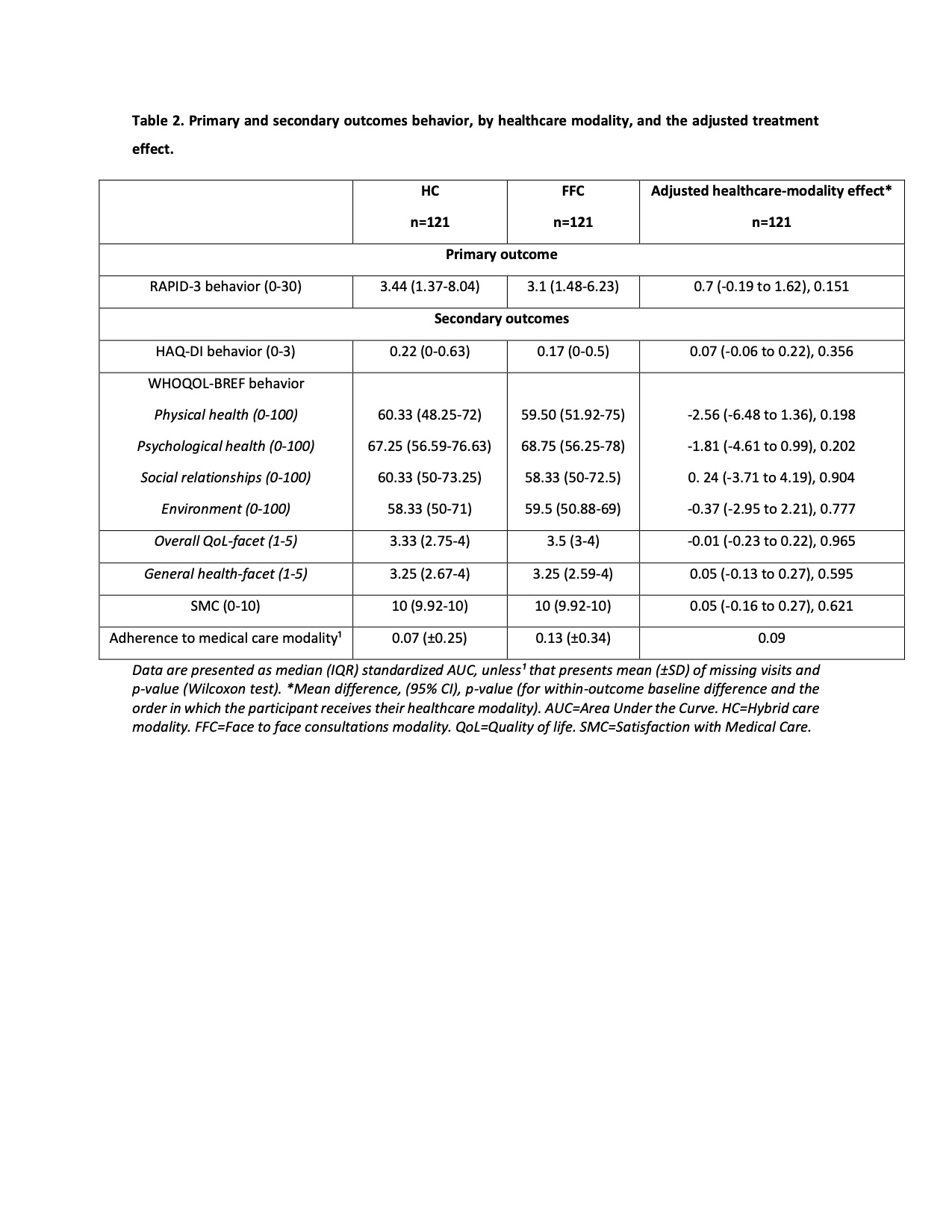
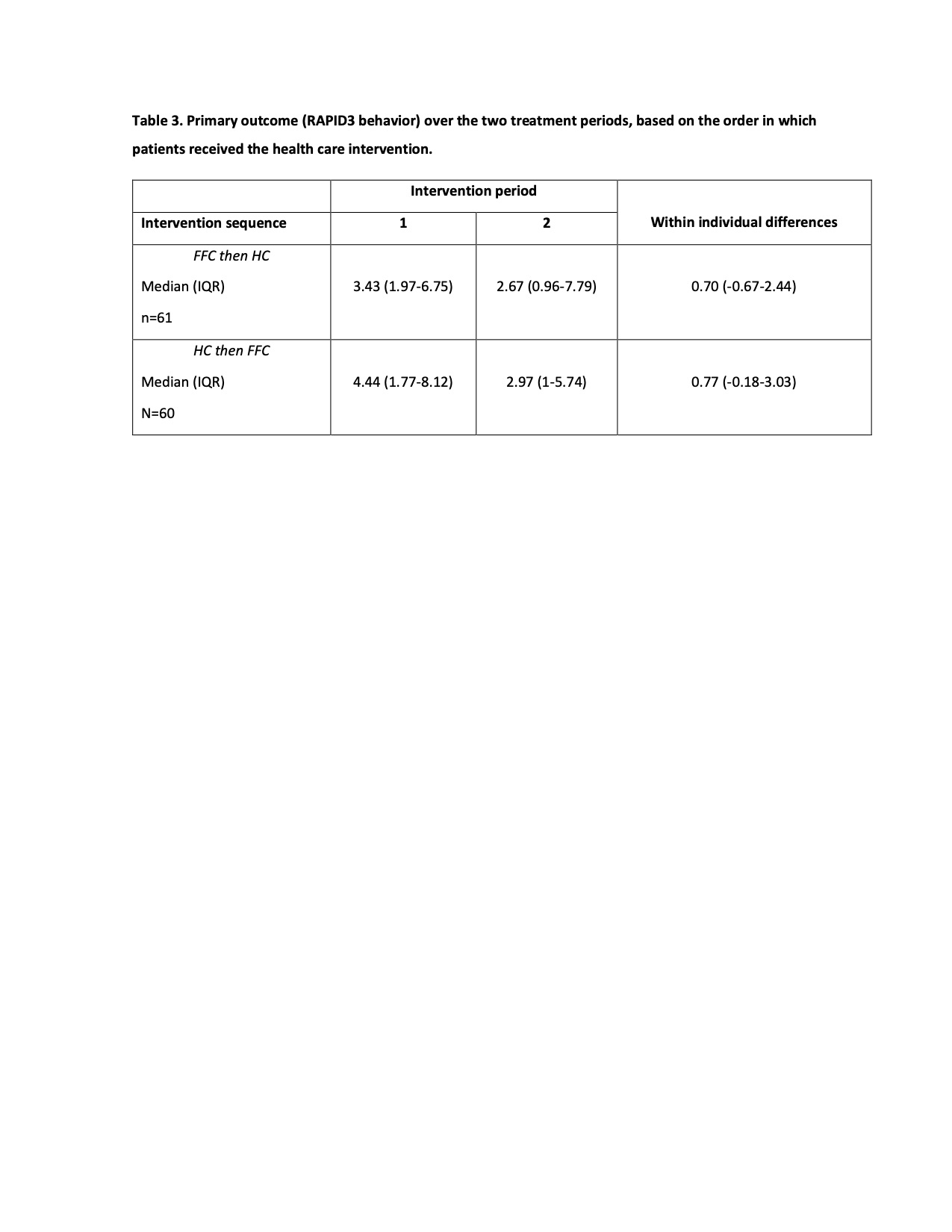
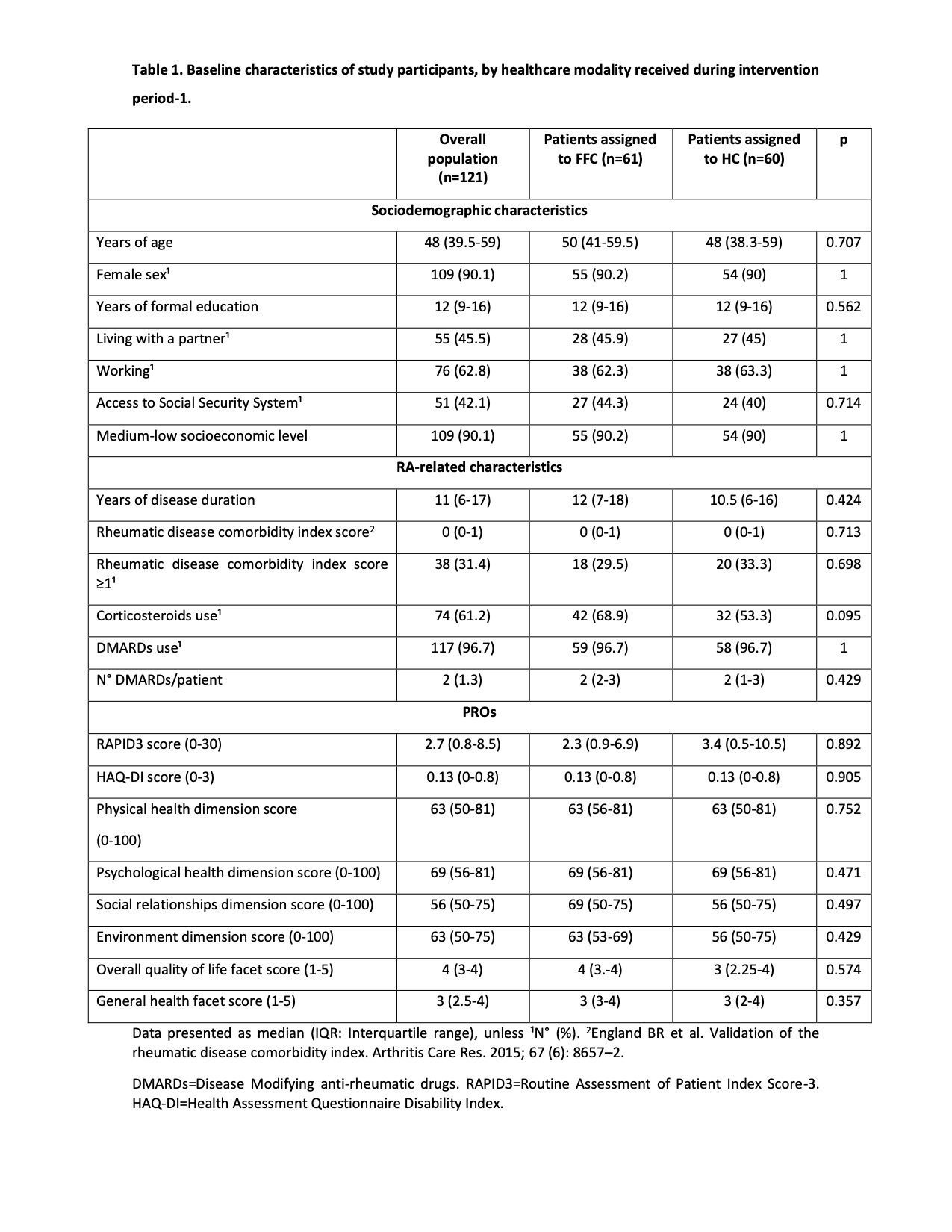
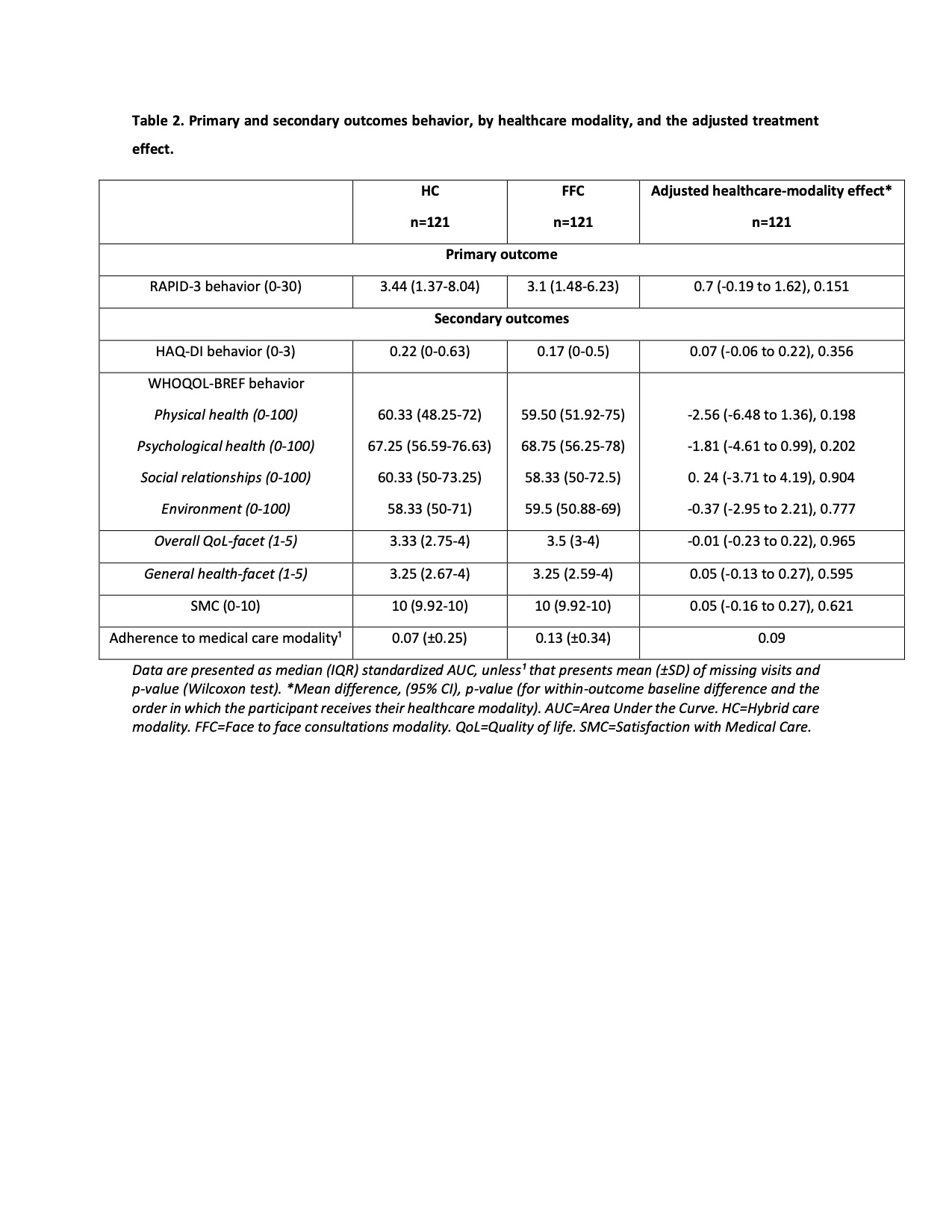
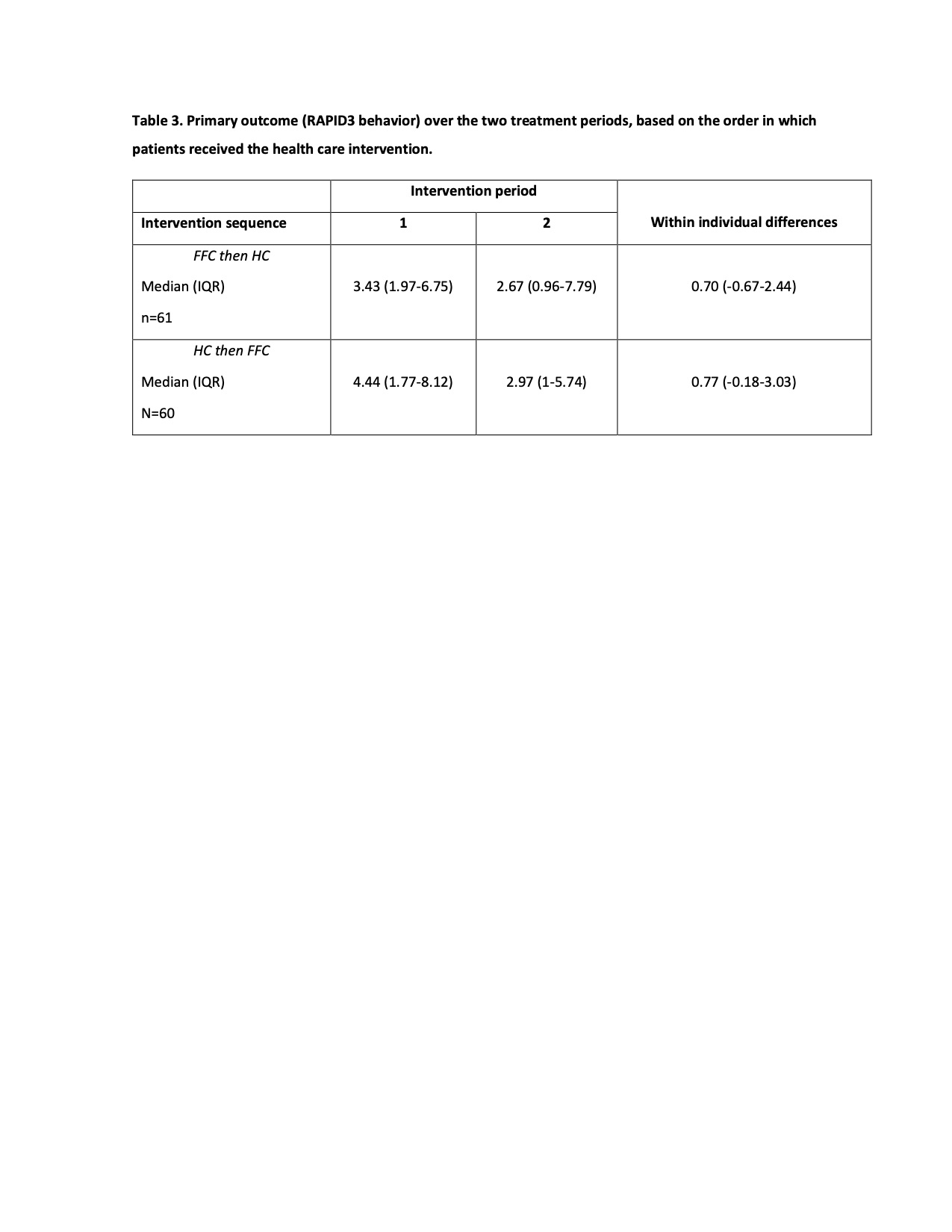
Results: There were 138 patients invited to participate, 130 agreed and 121 completed their study participation. Sixty-one and 60 patients respectively, received FFC and HC over the intervention period-1. Patients were primarily middle-aged females (90.1%), with 12 (IQR 9-16) years of education, long-standing disease, receiving DMARDs (96.7%), and corticosteroids (61.2%). Overall, they had low disease activity (median RAPID3: 2.7), while the quality of life was compromised. Table 1 summarizes the baseline characteristics of the participants and their comparison based on healthcare modality received during intervention period-1. Table 2 summarizes the results from comparing period-1 and period-2 of primary and secondary outcomes between patients assigned to either healthcare modality. Differences in RAPID3 behavior were below the non-inferiority margin, the adjusted intervention effect was 0.7, 95% CI (-0.19 to 1.62), and p=0.151.Table 3 summarizes the RAPID3 behavior over the two treatment periods, based on the order in which patients received the health care intervention. Within individual differences in RAPID3 behavior were below the non-inferiority margin and considered the order in which patients received the intervention. Finally, in the HC group, there were 313 consultations, among whom 133 (42.5%) were video conference consultations. The FFC ended more frequently with increased and reduced treatment recommendations, while video conference consultations with an unchanged treatment recommendation (p=0.014).
Conclusion: HC was non-inferior to in-person consultations in achieving PROs during the COVID-19 pandemic in RA patients. HC model impacts treatment decisions by favoring a more "contemplative" approach to patients' perceived outcomes.
Disclosures: G. Guaracha Basañez, None; I. Contreras-Yáñez, None; V. Estrada-González, None; L. Pacheco-Santiago, None; S. Valverde-Hernández, None; V. Pascual Ramos, None.
Background/Purpose: Patients and physicians can naturally adopt hybrid healthcare models (HC), that combine face-to-face consultations (FFC) with telemedicine. The study's objective was to compare the impact of two healthcare interventions, HC and FFC, on the patient-reported outcomes (PROs) of RA patients, during the current COVID-19 pandemic.
Methods: Consecutive patients reincorporated to an outpatient clinic previously lockdown, were invited to a non-inferiority, crossover, and randomized study (October 2020-May 2022). Patients were randomized to six months of FFC or HC (intervention period-1) and then the converse modality (intervention period-2). Intervention period-1 was followed by two months "washout period". The six months of FFC consisted of three to four consecutive standardized medical evaluations. The six months of HC consisted of three to four consecutive standardized medical evaluations, starting with a video conference consultation, and alternating with FFC, the period considered at least two video conference consultations. The primary outcome was disease activity/severity behavior (RAPID3). Additional PROs were disability (HAQ-DI), quality-of-life (WHOQOL-BREF), adherence to medical care, satisfaction with medical care, and treatment recommendations. Sample size calculation established 55 patients/healthcare intervention. To summarize PROs' behavior during the study, Areas Under the Curve (AUC) were calculated.
Results: There were 138 patients invited to participate, 130 agreed and 121 completed their study participation. Sixty-one and 60 patients respectively, received FFC and HC over the intervention period-1. Patients were primarily middle-aged females (90.1%), with 12 (IQR 9-16) years of education, long-standing disease, receiving DMARDs (96.7%), and corticosteroids (61.2%). Overall, they had low disease activity (median RAPID3: 2.7), while the quality of life was compromised. Table 1 summarizes the baseline characteristics of the participants and their comparison based on healthcare modality received during intervention period-1. Table 2 summarizes the results from comparing period-1 and period-2 of primary and secondary outcomes between patients assigned to either healthcare modality. Differences in RAPID3 behavior were below the non-inferiority margin, the adjusted intervention effect was 0.7, 95% CI (-0.19 to 1.62), and p=0.151.Table 3 summarizes the RAPID3 behavior over the two treatment periods, based on the order in which patients received the health care intervention. Within individual differences in RAPID3 behavior were below the non-inferiority margin and considered the order in which patients received the intervention. Finally, in the HC group, there were 313 consultations, among whom 133 (42.5%) were video conference consultations. The FFC ended more frequently with increased and reduced treatment recommendations, while video conference consultations with an unchanged treatment recommendation (p=0.014).
Conclusion: HC was non-inferior to in-person consultations in achieving PROs during the COVID-19 pandemic in RA patients. HC model impacts treatment decisions by favoring a more "contemplative" approach to patients' perceived outcomes.
Disclosures: G. Guaracha Basañez, None; I. Contreras-Yáñez, None; V. Estrada-González, None; L. Pacheco-Santiago, None; S. Valverde-Hernández, None; V. Pascual Ramos, None.

