Back
Poster Session C
Metabolic bone disease
Session: (1304–1331) Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
1326: Impact of COVID-19 Severity on Bone Mineral Density, Sarcopenia and Physical Performance Among Older Adults Following Hospitalization: A Pilot Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DC
Diego Cabrera, MD
Yale School of Medicine
Lima, Peru
Abstract Poster Presenter(s)
Diego Cabrera1, Clara Wong2, Andrew Cohen3, Lauren Ferrante3, Alexandra Hajduk3 and Evelyn Hsieh1, 1Section of Rheumatology, Allergy and Immunology, Yale School of Medicine, New Haven, CT, 2Yale School of Public Health, New Haven, CT, 3Yale School of Medicine, New Haven, CT
Background/Purpose: Altered bone mineral density (BMD), muscle mass and physical performance has been associated with adverse outcomes, however, the effect of COVID-19 on the musculoskeletal system is still not well described. Older individuals are at high risk for musculoskeletal impairments including weakness, deficiencies in performance and bone loss following hospitalization due to both illness and immobilization. This risk may be compounded among patients with severe COVID-19, which is characterized by hyperinflammation.
Methods: Individuals ≥60 years who completed 6 months of follow up as part of a virtual observational cohort of adults previously hospitalized for COVID-19 across a large U.S. health system were invited to participate in this study. Dual energy X-ray absorptiometry (DXA) was used to measure BMD at the lumbar spine (LS), femoral neck (FN) and total hip (TH), and trabecular bone score (TBS); DXA was also used to measure trunk and limb lean mass (LM) and fat mass (FM). Physical performance was assessed via the Short Physical Performance Battery (SPPB) (range 0-12, cutoff point ≤8) and physical strength via grip strength. Sarcopenia was assessed according to the European Working Group on Sarcopenia in Older People 2019 guidelines. Regression analyses were used to model associations between measures of COVID severity [based upon Sequential Organ Failure Assessment (SOFA) score (range 0-24, ≥3 associated with COVID severity), level of care received, and hsCRP and IL-6 levels during hospitalization] and musculoskeletal outcomes.
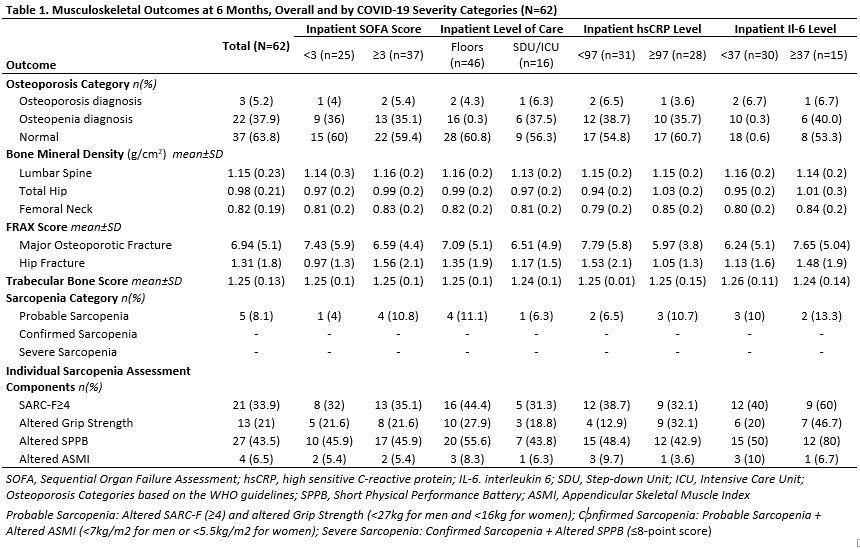
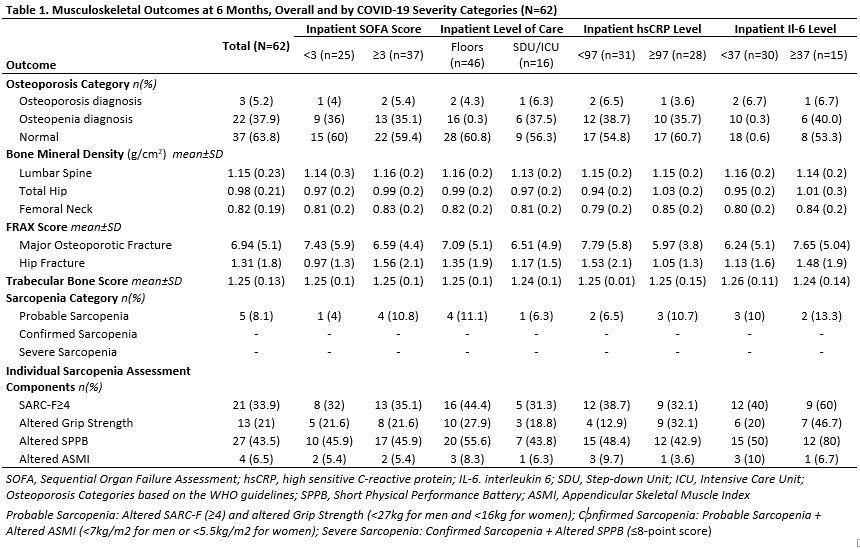
Results: Sixty-two participants were enrolled with a mean age of 68.5±6 years and 52% were male. The mean BMI was 30.5±9 kg/m2 and mean duration of hospitalization was 7±8 days. Mean FN, TH and LS BMD were 0.82±0.19 g/cm2, 0.98± 0.21g/cm2 and 1.15±0.23 g/cm2, respectively. Three patients (5.2%) were diagnosed with osteoporosis and 22/62 (37.9%) were diagnosed with low bone mineral density according to WHO guidelines. The mean TBS was 1.25±0.3. There was a weak negative correlation between SOFA score and TH (r=-0.18) and FN BMD (r=-0.09). Overall mean SPPB score was 8.3±1 and grip strength was 27.01±10 kg, with 27(43.5%) and 13(21%) patients scoring below the threshold on each one, respectively. Among the five participants with probable sarcopenia, four had a SOFA score ≥3. Higher comorbidity count (p=0.001) and trunk FM (p< 0.001) were independently associated with lower SPPB score but SOFA score showed no association.
Conclusion: In this pilot study, an important proportion of patients had altered BMD and physical performance and strength 6-9 months after their COVID-related hospitalization. Consistent with prior literature, age and BMI were independent factors related to BMD. Higher comorbidity count and trunk FM were associated with lower physical performance. Understanding the long-term impacts of COVID-19, and of COVID-19 severity, on musculoskeletal outcomes is critically important and larger prospective studies are warranted to inform prevention strategies.
Disclosures: D. Cabrera, None; C. Wong, None; A. Cohen, None; L. Ferrante, None; A. Hajduk, None; E. Hsieh, None.
Background/Purpose: Altered bone mineral density (BMD), muscle mass and physical performance has been associated with adverse outcomes, however, the effect of COVID-19 on the musculoskeletal system is still not well described. Older individuals are at high risk for musculoskeletal impairments including weakness, deficiencies in performance and bone loss following hospitalization due to both illness and immobilization. This risk may be compounded among patients with severe COVID-19, which is characterized by hyperinflammation.
Methods: Individuals ≥60 years who completed 6 months of follow up as part of a virtual observational cohort of adults previously hospitalized for COVID-19 across a large U.S. health system were invited to participate in this study. Dual energy X-ray absorptiometry (DXA) was used to measure BMD at the lumbar spine (LS), femoral neck (FN) and total hip (TH), and trabecular bone score (TBS); DXA was also used to measure trunk and limb lean mass (LM) and fat mass (FM). Physical performance was assessed via the Short Physical Performance Battery (SPPB) (range 0-12, cutoff point ≤8) and physical strength via grip strength. Sarcopenia was assessed according to the European Working Group on Sarcopenia in Older People 2019 guidelines. Regression analyses were used to model associations between measures of COVID severity [based upon Sequential Organ Failure Assessment (SOFA) score (range 0-24, ≥3 associated with COVID severity), level of care received, and hsCRP and IL-6 levels during hospitalization] and musculoskeletal outcomes.
Results: Sixty-two participants were enrolled with a mean age of 68.5±6 years and 52% were male. The mean BMI was 30.5±9 kg/m2 and mean duration of hospitalization was 7±8 days. Mean FN, TH and LS BMD were 0.82±0.19 g/cm2, 0.98± 0.21g/cm2 and 1.15±0.23 g/cm2, respectively. Three patients (5.2%) were diagnosed with osteoporosis and 22/62 (37.9%) were diagnosed with low bone mineral density according to WHO guidelines. The mean TBS was 1.25±0.3. There was a weak negative correlation between SOFA score and TH (r=-0.18) and FN BMD (r=-0.09). Overall mean SPPB score was 8.3±1 and grip strength was 27.01±10 kg, with 27(43.5%) and 13(21%) patients scoring below the threshold on each one, respectively. Among the five participants with probable sarcopenia, four had a SOFA score ≥3. Higher comorbidity count (p=0.001) and trunk FM (p< 0.001) were independently associated with lower SPPB score but SOFA score showed no association.
Conclusion: In this pilot study, an important proportion of patients had altered BMD and physical performance and strength 6-9 months after their COVID-related hospitalization. Consistent with prior literature, age and BMI were independent factors related to BMD. Higher comorbidity count and trunk FM were associated with lower physical performance. Understanding the long-term impacts of COVID-19, and of COVID-19 severity, on musculoskeletal outcomes is critically important and larger prospective studies are warranted to inform prevention strategies.
Disclosures: D. Cabrera, None; C. Wong, None; A. Cohen, None; L. Ferrante, None; A. Hajduk, None; E. Hsieh, None.

