Back
Poster Session C
Metabolic bone disease
Session: (1304–1331) Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
1330: Impact of COVID-19 Severity on Physical Function, Mobility, Falls and Fractures Among Older Patients After Hospitalization: A Longitudinal Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CW
Clara Wong, MPH
Yale School of Public Health
New Haven, CT, United States
Abstract Poster Presenter(s)
Clara Wong1, Diego Cabrera2, Mary Geda3, Andrew Cohen3, Lauren Ferrante3, Alexandra Hajduk3 and Evelyn Hsieh2, 1Yale School of Public Health, New Haven, CT, 2Section of Rheumatology, Allergy and Immunology, Yale School of Medicine, New Haven, CT, 3Yale School of Medicine, New Haven, CT
Background/Purpose: No longitudinal studies have examined the impact of COVID-19 or COVID-19 severity on physical function and disability outcomes among older adults. Multiple factors, including illness- and rehabilitation-related factors, can create a perfect storm for prolonged disability, and increased falls and fractures in this population. We evaluated the association between baseline severity of COVID-19 with outcomes at 6 months, including physical function, incident falls and fracture in a longitudinal virtual cohort of older patients.
Methods: The VALIANT (COVID-19 in Older Adults: A Longitudinal Assessment) study is a prospective observational cohort study that enrolled patients ≥60 years hospitalized for COVID-19 across the Yale-New Haven Health System from 7/2020-6/2021. Participants completed telephone survey interviews at baseline, and 1-, 3- and 6-months following hospital discharge. The survey included questions regarding sociodemographic characteristics, baseline health status, COVID-19 related factors, physical function, mobility, and falls/fractures. Stratified analyses by COVID-19 severity were performed based upon: Sequential Organ Failure Assessment (SOFA) score (range 0-24, ≥3 associated with increased COVID severity), level of care received, and inflammatory marker levels during hospitalization (hsCRP and IL-6).
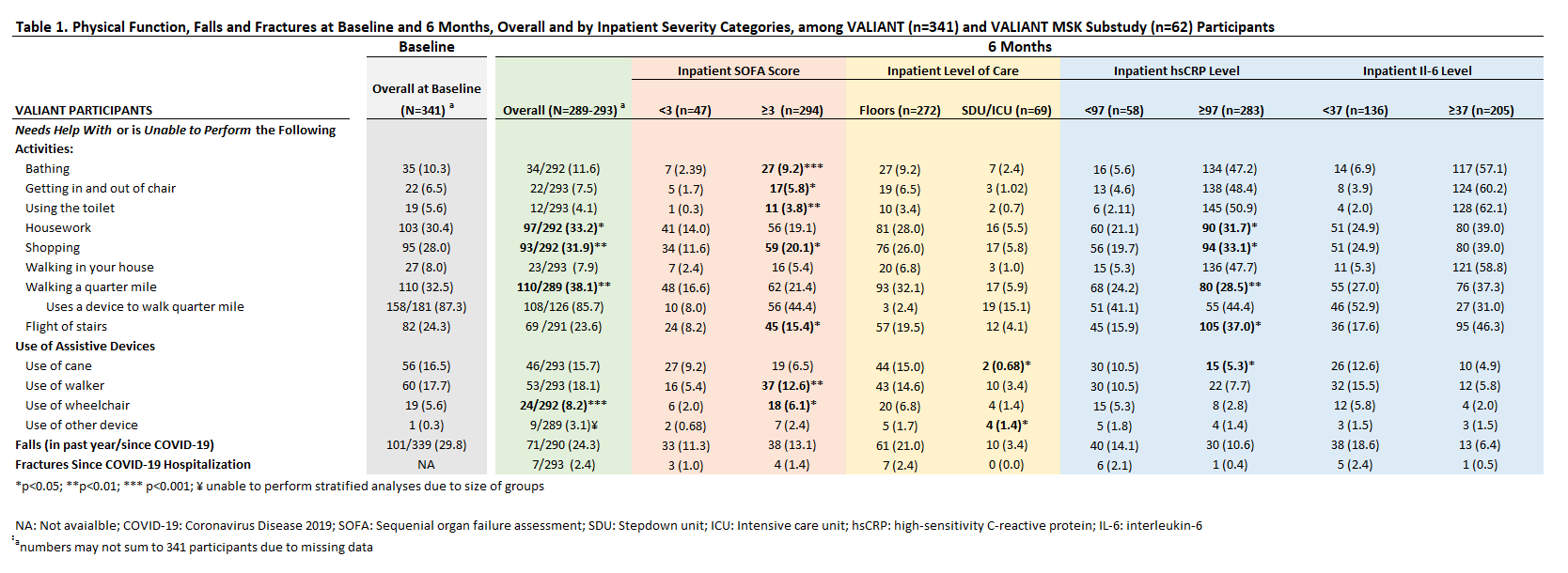
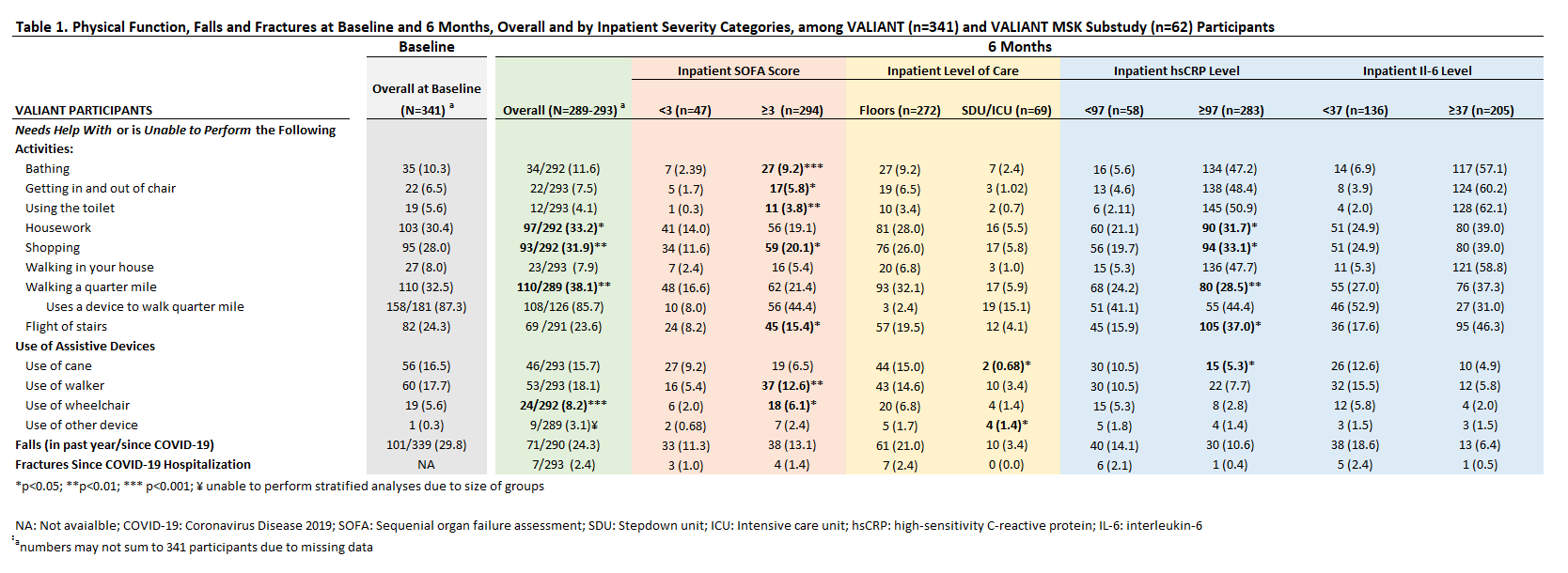
Results: We enrolled 341 participants (49% women, 72.5% White), with a median age of 70 (IQR 12) years. The proportion of patients reporting impairments with 8 different physical function domains at baseline and 6 months is shown in Table 1. At 6 months, we found a higher proportion of patients unable to independently do housework (33.2% vs 30.4%, p= 0.013), shop (31.9% vs 28.0%, p=0.002) and walk a quarter mile (38.1% vs 32.5%, p=0.008). When physical function at 6 months was stratified by COVID-19 severity, we found a higher proportion of patients with a high SOFA score (≥3 vs. < 3) reported being unable to independently bathe (9.2% vs 2.4%, p< 0.001), get in and out of a chair (5.8% vs 1.7%, p=0.017), use the toilet (3.8% vs 0.3%, p=0.006), shop (20.1% vs 11.6%, p=0.011), or walk flight of stairs (15.4% vs 8.2%, p=0.016). A significantly higher proportion of patients with high inpatient hsCRP levels (≥97 mg/L) were unable to independently do housework (31.7% vs 21.1%, p= 0.013), shop (33.1% vs 19.7%, p=0.043), walk a quarter mile (28.5% vs 24.2%, p=0.009) and walk a flight of stairs (37.0% vs 15.9%. p= 0.0114). Thirty percent (101/339) of participants reported a fall in the past year before COVID-19, while 24.3% participants reported a fall in the 6 months since COVID-19 hospitalization. There were no significant differences in incident falls when categorized by COVID severity. Seven participants reported having a fracture following hospitalization.
Conclusion: In this study, a greater proportion of older adults with severe COVID-19 reported impairments in multiple domains related to physical function and disability at 6 months post-hospitalization. Proactive strategies emphasizing rehabilitation and functional recovery are critically important for older adults hospitalized with COVID-19, particularly those with severe disease.
Disclosures: C. Wong, None; D. Cabrera, None; M. Geda, None; A. Cohen, None; L. Ferrante, None; A. Hajduk, None; E. Hsieh, None.
Background/Purpose: No longitudinal studies have examined the impact of COVID-19 or COVID-19 severity on physical function and disability outcomes among older adults. Multiple factors, including illness- and rehabilitation-related factors, can create a perfect storm for prolonged disability, and increased falls and fractures in this population. We evaluated the association between baseline severity of COVID-19 with outcomes at 6 months, including physical function, incident falls and fracture in a longitudinal virtual cohort of older patients.
Methods: The VALIANT (COVID-19 in Older Adults: A Longitudinal Assessment) study is a prospective observational cohort study that enrolled patients ≥60 years hospitalized for COVID-19 across the Yale-New Haven Health System from 7/2020-6/2021. Participants completed telephone survey interviews at baseline, and 1-, 3- and 6-months following hospital discharge. The survey included questions regarding sociodemographic characteristics, baseline health status, COVID-19 related factors, physical function, mobility, and falls/fractures. Stratified analyses by COVID-19 severity were performed based upon: Sequential Organ Failure Assessment (SOFA) score (range 0-24, ≥3 associated with increased COVID severity), level of care received, and inflammatory marker levels during hospitalization (hsCRP and IL-6).
Results: We enrolled 341 participants (49% women, 72.5% White), with a median age of 70 (IQR 12) years. The proportion of patients reporting impairments with 8 different physical function domains at baseline and 6 months is shown in Table 1. At 6 months, we found a higher proportion of patients unable to independently do housework (33.2% vs 30.4%, p= 0.013), shop (31.9% vs 28.0%, p=0.002) and walk a quarter mile (38.1% vs 32.5%, p=0.008). When physical function at 6 months was stratified by COVID-19 severity, we found a higher proportion of patients with a high SOFA score (≥3 vs. < 3) reported being unable to independently bathe (9.2% vs 2.4%, p< 0.001), get in and out of a chair (5.8% vs 1.7%, p=0.017), use the toilet (3.8% vs 0.3%, p=0.006), shop (20.1% vs 11.6%, p=0.011), or walk flight of stairs (15.4% vs 8.2%, p=0.016). A significantly higher proportion of patients with high inpatient hsCRP levels (≥97 mg/L) were unable to independently do housework (31.7% vs 21.1%, p= 0.013), shop (33.1% vs 19.7%, p=0.043), walk a quarter mile (28.5% vs 24.2%, p=0.009) and walk a flight of stairs (37.0% vs 15.9%. p= 0.0114). Thirty percent (101/339) of participants reported a fall in the past year before COVID-19, while 24.3% participants reported a fall in the 6 months since COVID-19 hospitalization. There were no significant differences in incident falls when categorized by COVID severity. Seven participants reported having a fracture following hospitalization.
Conclusion: In this study, a greater proportion of older adults with severe COVID-19 reported impairments in multiple domains related to physical function and disability at 6 months post-hospitalization. Proactive strategies emphasizing rehabilitation and functional recovery are critically important for older adults hospitalized with COVID-19, particularly those with severe disease.
Disclosures: C. Wong, None; D. Cabrera, None; M. Geda, None; A. Cohen, None; L. Ferrante, None; A. Hajduk, None; E. Hsieh, None.

