Back
Poster Session C
Pediatric autoimmune diseases: Kawasaki disease, juvenile dermatomyositis and juvenile localized scleroderma
Session: (1360–1386) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
1363: Impact of SARS-CoV-2 on the Clinical Presentation of Juvenile Idiopathic Inflammatory Myopathies
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JP
Jessica Perfetto, MD
The Children's Hospital at Montefiore
New York, NY, United States
Abstract Poster Presenter(s)
Jessica Perfetto1, Donna Yoo2, Carolina Tamashiro3, Megan Perron4, Natalia Vasquez Canizares5 and Dawn Wahezi6, 1The Children's Hospital at Montefiore, Division of Rheumatology, Bronx, NY, 2Albert Einstein College of Medicine, Bronx, NY, 3The Children's Hospital at Montefiore, Department of Pediatrics, Bronx, NY, 4Children's Hospital Colorado, Division of Rheumatology, Aurora, CO, 5Children's Hospital at Montefiore/ Albert Einstein College of Medicine, New York, NY, 6Children's Hospital at Montefiore, Bronx, NY
Background/Purpose: Viruses can trigger juvenile idiopathic inflammatory myopathies (JIIM), including juvenile dermatomyositis (JDM), juvenile polymyositis (JPM), and overlap myositis. There is growing evidence that infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can trigger autoimmune diseases in genetically susceptible individuals, including idiopathic inflammatory myopathies (IIM). Studies show similarities between SARS-CoV-2 infection and anti-melanoma differentiation-associated gene 5 (MDA5) antibody-related dermatomyositis, suggesting possible shared underlying autoimmune and/or inflammatory mechanisms. To date, few studies described individual cases of JIIM following SARS-CoV-2 infection, and, to our knowledge, none explored its effects on the clinical presentation of JIIM. In this study, we aim to investigate the impact of SARS-CoV-2 on JIIM by comparing onset of new JIIM cases and clinical and laboratory characteristics at disease onset in patients diagnosed before and after onset of the Coronavirus Disease 2019 pandemic (COVID 19).
Methods: Patients diagnosed with JIIM prior to age 19 at The Children's Hospital at Montefiore were eligible for study inclusion. Demographic, clinical, and laboratory data, as well as evidence of exposure to SARS-CoV-2, were collected retrospectively by manual chart review. Patients were grouped into pre-COVID 19 (defined as prior to January 1, 2020) and post-COVID 19 (defined as January 1, 2020, or later). Descriptive statistics were used to summarize each variable. Non-parametric testing was performed using Fischer's exact test and Wilcoxon rank sum test.
Results: Forty-four patients were included (Table 1). Thirty-four patients (77.3%) were diagnosed pre-COVID 19 and ten patients (22.7%) were diagnosed post-COVID 19, of which five (50%) had known exposure to or infection with SARS-CoV-2. Patients diagnosed with JIIM post-COVID 19 were more likely to be non-Hispanic Black or Asian (p = 0.041), develop disease at an older age (p = 0.009), and present with non-classic cutaneous manifestations (as opposed to classic findings of Gottron's papules/sign or Heliotrope rash) (p = 0.031), despite similar frequencies of JDM versus overlap myositis. While presence of muscle weakness did not differ between the groups, patients diagnosed post-COVID 19 tended to have more severe weakness, though results were not statistically significant. Despite delays to diagnosis reported during the pandemic, there was no difference between time from symptom onset to diagnosis.
Conclusion: This is the first study to explore the potential effects of SARS-CoV-2 on the clinical presentation of JIIM. In our center, we found that patients diagnosed with JIIM after COVID 19 were more likely to be racial minorities, older, and present with non-classic cutaneous manifestations. Clinicians should consider JIIM even in the absence of classic cutaneous manifestations, particularly in the post-COVID 19 era. Patients should be followed longitudinally to explore long-term impacts of SARS-CoV-2 on JIIM. Further investigation is warranted to identify the mechanisms by which SARS-CoV-2 impacts JIIM and how these differ from the effects of other viruses.
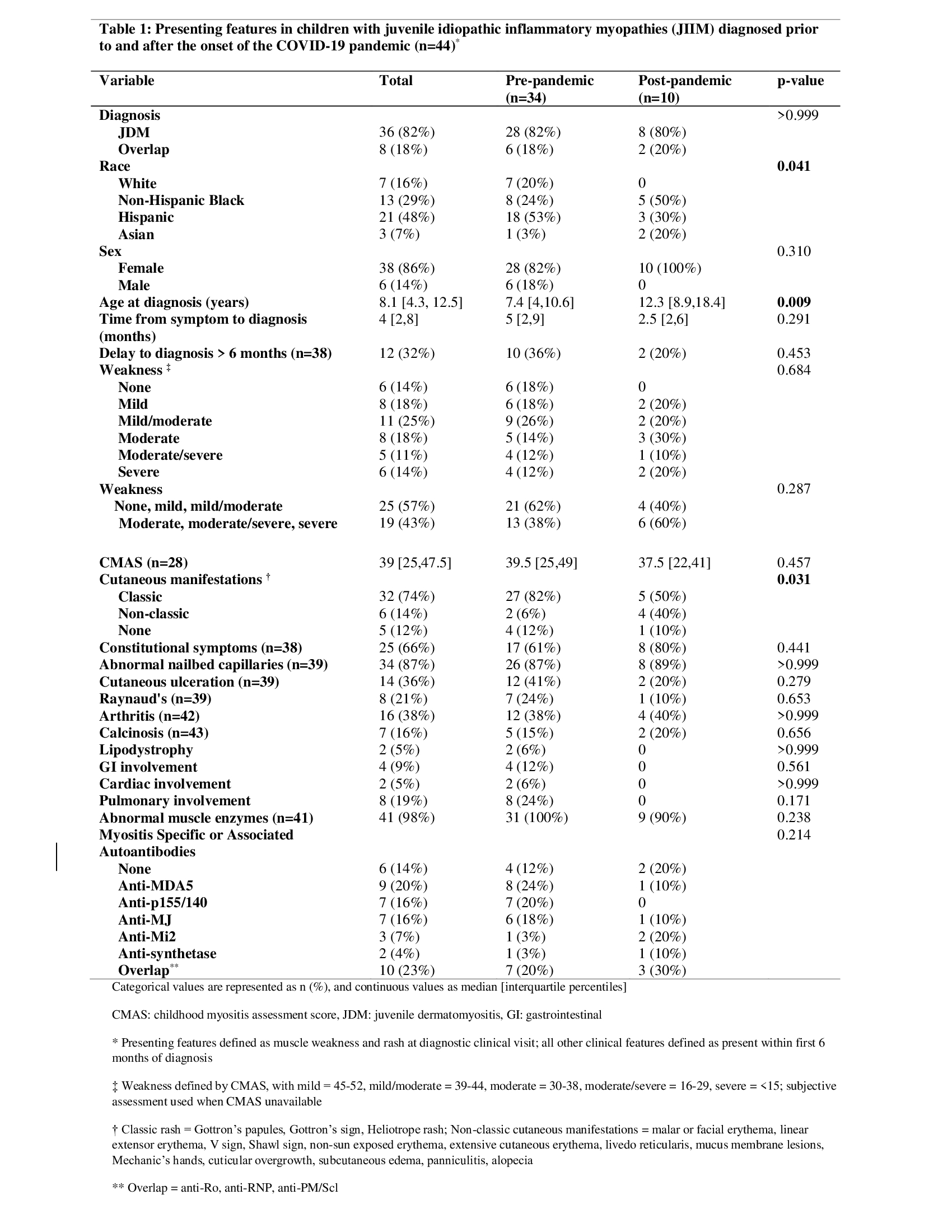 Table 1
Table 1
Disclosures: J. Perfetto, None; D. Yoo, None; C. Tamashiro, None; M. Perron, None; N. Vasquez Canizares, None; D. Wahezi, None.
Background/Purpose: Viruses can trigger juvenile idiopathic inflammatory myopathies (JIIM), including juvenile dermatomyositis (JDM), juvenile polymyositis (JPM), and overlap myositis. There is growing evidence that infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can trigger autoimmune diseases in genetically susceptible individuals, including idiopathic inflammatory myopathies (IIM). Studies show similarities between SARS-CoV-2 infection and anti-melanoma differentiation-associated gene 5 (MDA5) antibody-related dermatomyositis, suggesting possible shared underlying autoimmune and/or inflammatory mechanisms. To date, few studies described individual cases of JIIM following SARS-CoV-2 infection, and, to our knowledge, none explored its effects on the clinical presentation of JIIM. In this study, we aim to investigate the impact of SARS-CoV-2 on JIIM by comparing onset of new JIIM cases and clinical and laboratory characteristics at disease onset in patients diagnosed before and after onset of the Coronavirus Disease 2019 pandemic (COVID 19).
Methods: Patients diagnosed with JIIM prior to age 19 at The Children's Hospital at Montefiore were eligible for study inclusion. Demographic, clinical, and laboratory data, as well as evidence of exposure to SARS-CoV-2, were collected retrospectively by manual chart review. Patients were grouped into pre-COVID 19 (defined as prior to January 1, 2020) and post-COVID 19 (defined as January 1, 2020, or later). Descriptive statistics were used to summarize each variable. Non-parametric testing was performed using Fischer's exact test and Wilcoxon rank sum test.
Results: Forty-four patients were included (Table 1). Thirty-four patients (77.3%) were diagnosed pre-COVID 19 and ten patients (22.7%) were diagnosed post-COVID 19, of which five (50%) had known exposure to or infection with SARS-CoV-2. Patients diagnosed with JIIM post-COVID 19 were more likely to be non-Hispanic Black or Asian (p = 0.041), develop disease at an older age (p = 0.009), and present with non-classic cutaneous manifestations (as opposed to classic findings of Gottron's papules/sign or Heliotrope rash) (p = 0.031), despite similar frequencies of JDM versus overlap myositis. While presence of muscle weakness did not differ between the groups, patients diagnosed post-COVID 19 tended to have more severe weakness, though results were not statistically significant. Despite delays to diagnosis reported during the pandemic, there was no difference between time from symptom onset to diagnosis.
Conclusion: This is the first study to explore the potential effects of SARS-CoV-2 on the clinical presentation of JIIM. In our center, we found that patients diagnosed with JIIM after COVID 19 were more likely to be racial minorities, older, and present with non-classic cutaneous manifestations. Clinicians should consider JIIM even in the absence of classic cutaneous manifestations, particularly in the post-COVID 19 era. Patients should be followed longitudinally to explore long-term impacts of SARS-CoV-2 on JIIM. Further investigation is warranted to identify the mechanisms by which SARS-CoV-2 impacts JIIM and how these differ from the effects of other viruses.
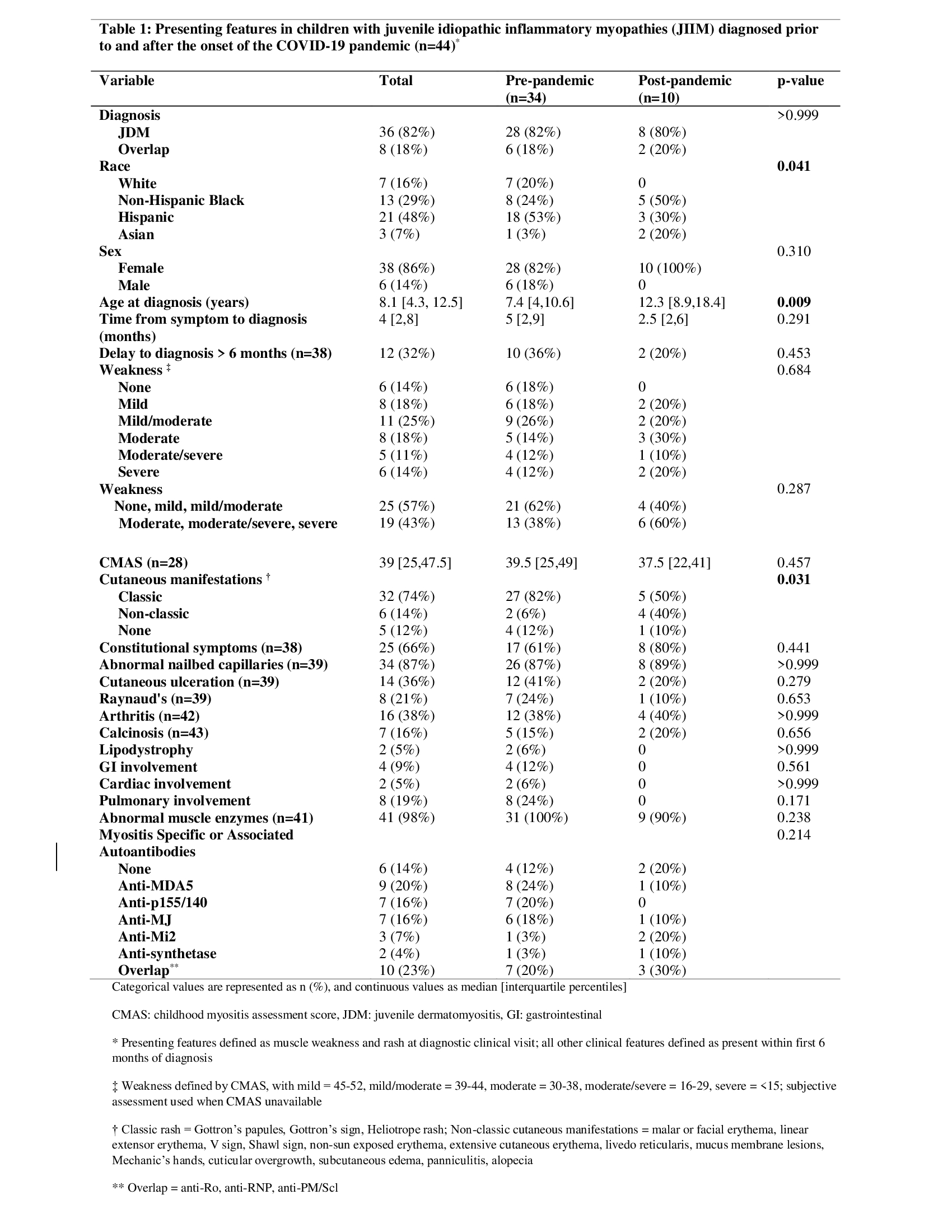 Table 1
Table 1Disclosures: J. Perfetto, None; D. Yoo, None; C. Tamashiro, None; M. Perron, None; N. Vasquez Canizares, None; D. Wahezi, None.

