Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1449: Incidence and Risk Factors for Active Tuberculosis in Patients with Systemic Lupus Erythematosus: A Multicenter Prospective Cohort Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LZ
Lifan ZHANG, MD, PhD, MPH
Peking Union Medical College Hospital
Beijing, Beijing, China
Abstract Poster Presenter(s)
Lifan Zhang1, xiaoqing zou2, Lantian Xie3, Jianghao Liu3, zhengrong yang4, qifei cao4, Chunlei Li5, Xiaochuan Sun5, Fengchun ZHANG6, Yan Zhao7, Xiaofeng Zeng8 and Xiaoqing Liu1, 1Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College; Clinical Epidemiology Unit, Peking Union Medical College, International Clinical Epidemiology Network; Center for Tuberculosis Research, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College; School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 3Peking Union Medical College Hospital, Peking Union Medical College, Beijing, China, 4Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 5Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 6Peking Union Medical College Hospital, Beijing, China, 7Department of Rheumatology and Clinical Immunology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Key Laboratory of Rheumatology & Clinical Immunology, Ministry of Education, Beijing, China, 8Department of Rheumatology, Peking Union Medical College Hospital (PUMCH), Chinese Academy of Medical Sciences National Clinical Research Center for Dermatologic and Immunologic Diseases (NCRC-DID), Beijing, China
Background/Purpose: The burden of tuberculosis (TB) and systemic lupus erythematosus (SLE) in China are both the second largest in the world. Patients with SLE are at high risk of developing TB, while there are no guidelines for prevention and management of TB in this population in China. This study aimed to investigate the incidence and explore the risk factors of active TB in patients with SLE, so as to provide evidence for the formulation of tuberculosis prevention and management strategies in patients with SLE in China.
Methods: We conducted a multicenter prospective cohort study. During September 2014 to March 2016, we recruited confirmed SLE outpatients and inpatients from 13 tertiary grade A general hospitals in eastern, central and western China. We collected baseline demographic characteristics, TB infection status, clinical diagnosis, treatment information, laboratory information and the incidence of active TB during follow-up. Survival curves were plotted using Kaplan–Meier method. Log-rank tests were used to assess the differences in the incidence of active TB. Risk factors for active TB disease were explored by the COX proportional risk model.
Results: Of the 1361 patients with SLE, 16 patients developed active TB and the median follow-up time is 59 months (IQR 56-63). The 1-year incidence of ATB in SLE patients was 367/100,000 (95% CI 119/100 000-855/100,000) and the 5-year cumulative incidence was 1125/100,000 (95% CI 631/100,000-1849/100,000). The results of COX multivariate regression analysis showed that the maximum daily dose of glucocorticoids (5 mg/day) (adjusted hazard ratio [aHR] = 1.14, 95% CI: 1.02-1.27, P = 0.019) and tuberculosis infection status (aHR = 8.71, 95% CI: 3.23-23.47, P < 0.001) were independent risk factors for active TB in patients with SLE, and that the lymphocyte percentage (aHR=0.94, 95% CI: 0.89-0.99, P=0.022) was a protective factor for active TB in patients with SLE.
Conclusion: The incidence of TB is higher in patients with SLE than in the general population. The risk of active TB in SLE patients is higher when the daily dose of glucocorticoids is increased or when they are in TB infection status. Therefore, prevention and treatment of tuberculosis should be considered in SLE patients.
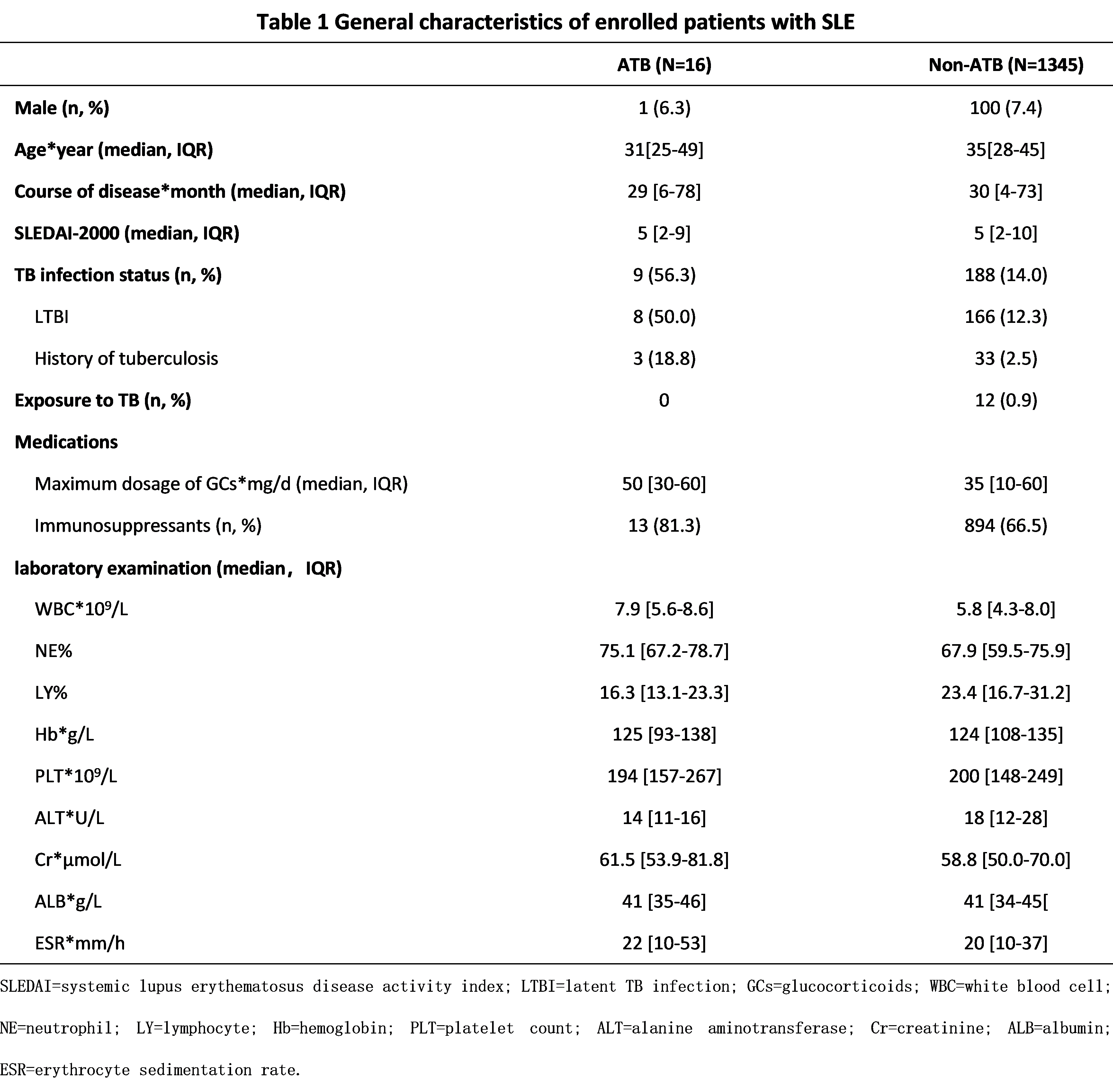 Table 1. General characteristics of enrolled patients with SLE
Table 1. General characteristics of enrolled patients with SLE
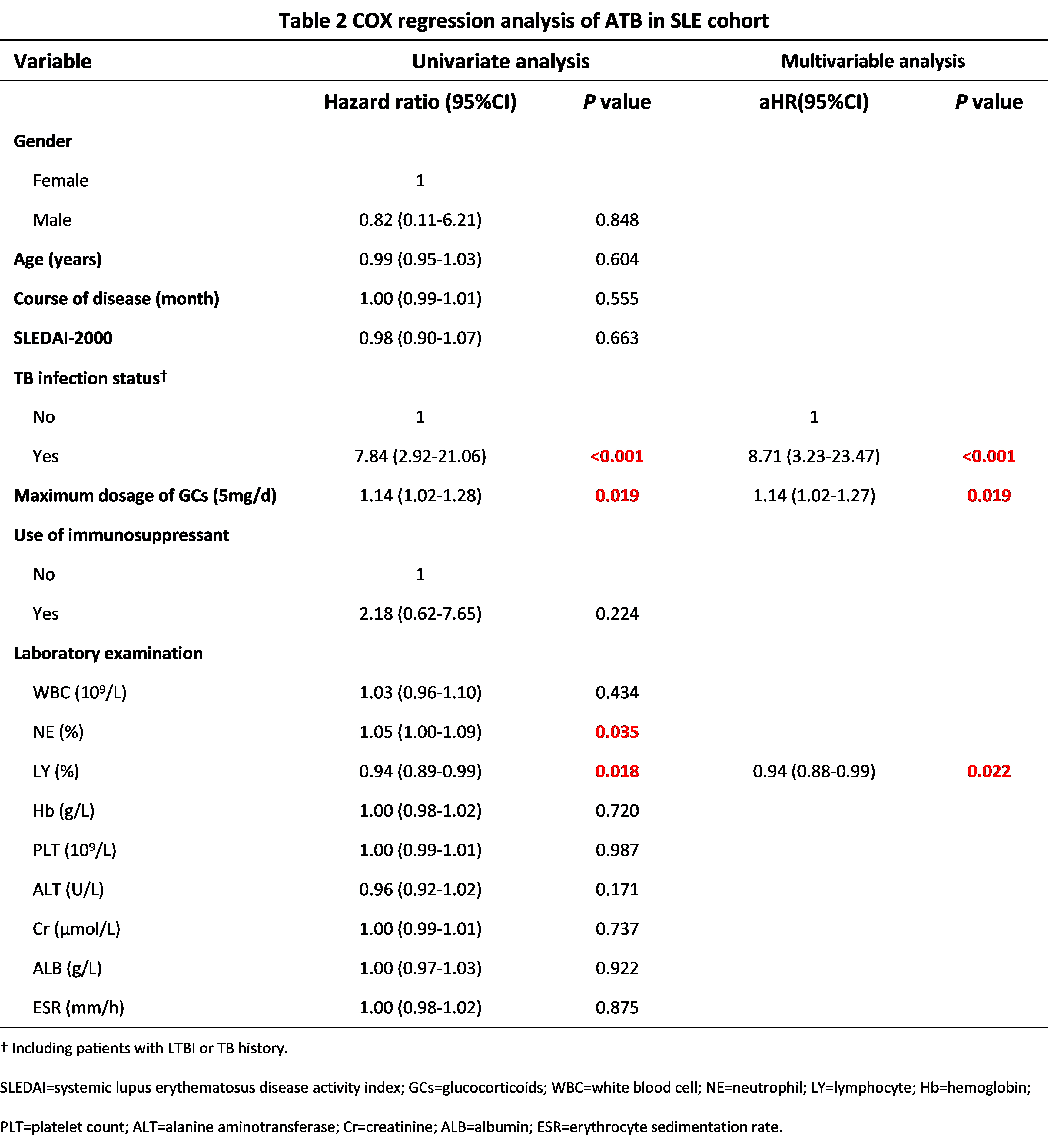 Table 2. COX regression analysis of ATB in SLE cohort
Table 2. COX regression analysis of ATB in SLE cohort
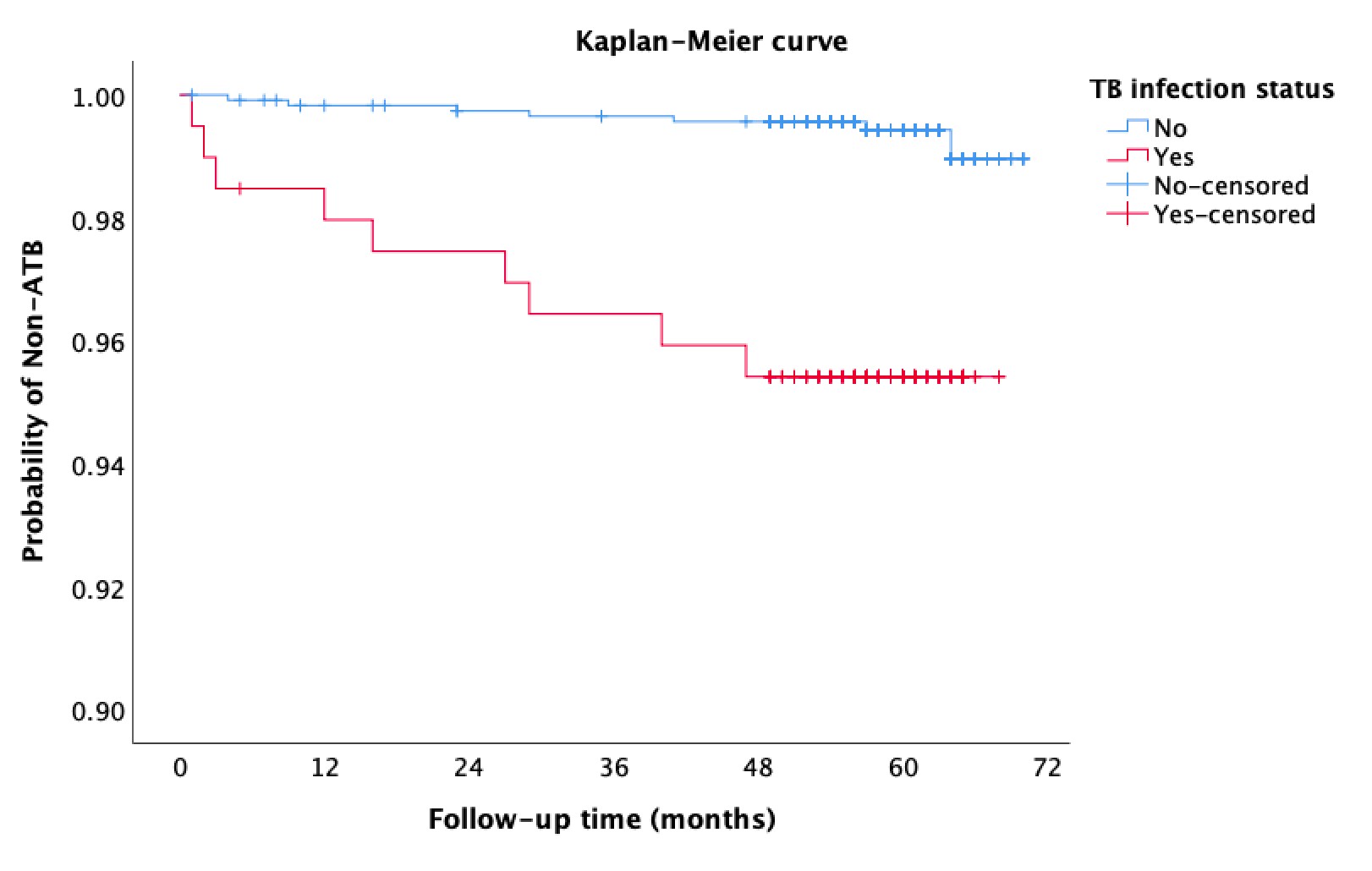 Figure 1. Incidence of ATB in patients with SLE according to TB infection status
Figure 1. Incidence of ATB in patients with SLE according to TB infection status
Disclosures: L. Zhang, None; x. zou, None; L. Xie, None; J. Liu, None; z. yang, None; q. cao, None; C. Li, None; X. Sun, None; F. ZHANG, None; Y. Zhao, None; X. Zeng, None; X. Liu, None.
Background/Purpose: The burden of tuberculosis (TB) and systemic lupus erythematosus (SLE) in China are both the second largest in the world. Patients with SLE are at high risk of developing TB, while there are no guidelines for prevention and management of TB in this population in China. This study aimed to investigate the incidence and explore the risk factors of active TB in patients with SLE, so as to provide evidence for the formulation of tuberculosis prevention and management strategies in patients with SLE in China.
Methods: We conducted a multicenter prospective cohort study. During September 2014 to March 2016, we recruited confirmed SLE outpatients and inpatients from 13 tertiary grade A general hospitals in eastern, central and western China. We collected baseline demographic characteristics, TB infection status, clinical diagnosis, treatment information, laboratory information and the incidence of active TB during follow-up. Survival curves were plotted using Kaplan–Meier method. Log-rank tests were used to assess the differences in the incidence of active TB. Risk factors for active TB disease were explored by the COX proportional risk model.
Results: Of the 1361 patients with SLE, 16 patients developed active TB and the median follow-up time is 59 months (IQR 56-63). The 1-year incidence of ATB in SLE patients was 367/100,000 (95% CI 119/100 000-855/100,000) and the 5-year cumulative incidence was 1125/100,000 (95% CI 631/100,000-1849/100,000). The results of COX multivariate regression analysis showed that the maximum daily dose of glucocorticoids (5 mg/day) (adjusted hazard ratio [aHR] = 1.14, 95% CI: 1.02-1.27, P = 0.019) and tuberculosis infection status (aHR = 8.71, 95% CI: 3.23-23.47, P < 0.001) were independent risk factors for active TB in patients with SLE, and that the lymphocyte percentage (aHR=0.94, 95% CI: 0.89-0.99, P=0.022) was a protective factor for active TB in patients with SLE.
Conclusion: The incidence of TB is higher in patients with SLE than in the general population. The risk of active TB in SLE patients is higher when the daily dose of glucocorticoids is increased or when they are in TB infection status. Therefore, prevention and treatment of tuberculosis should be considered in SLE patients.
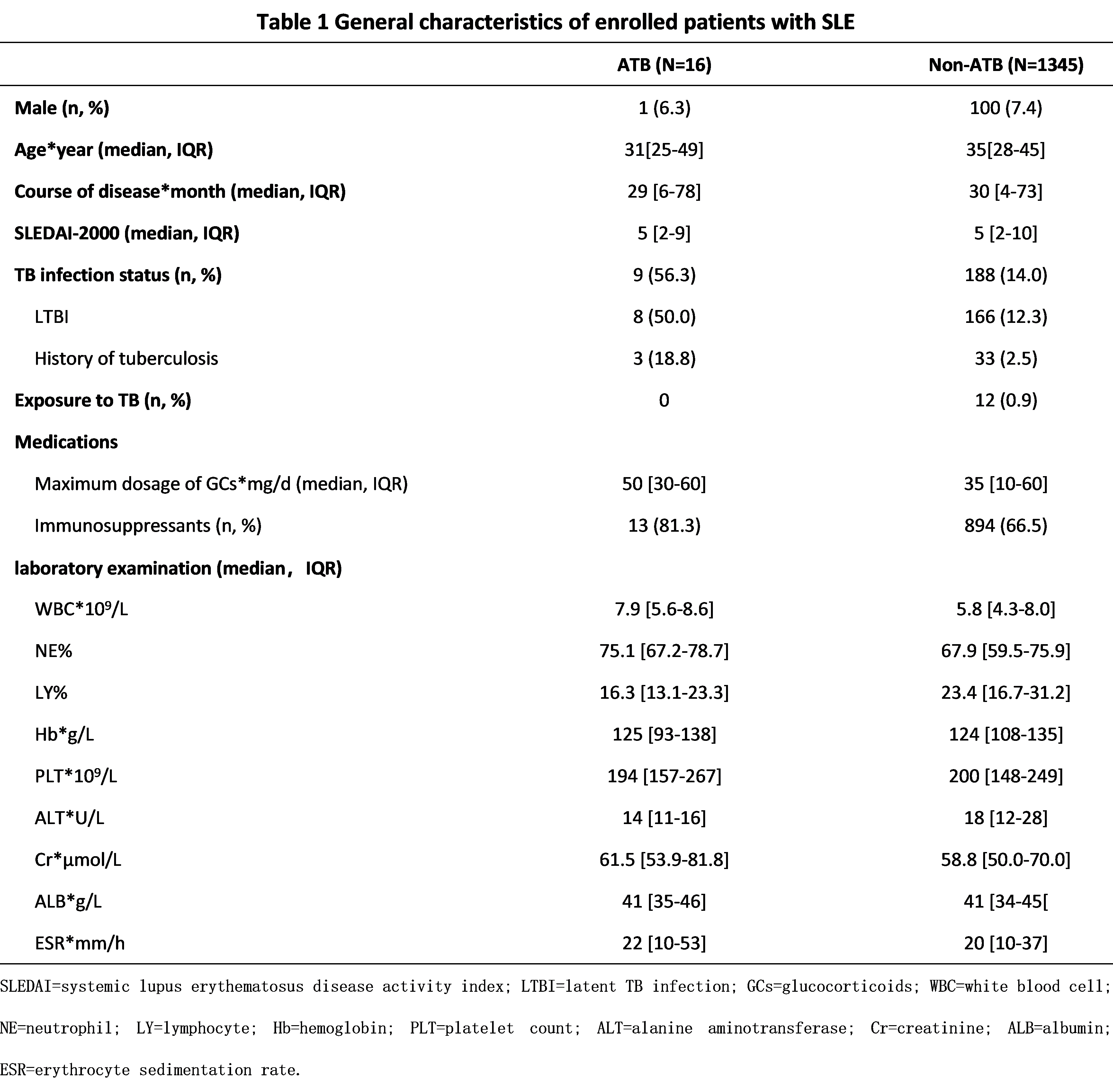 Table 1. General characteristics of enrolled patients with SLE
Table 1. General characteristics of enrolled patients with SLE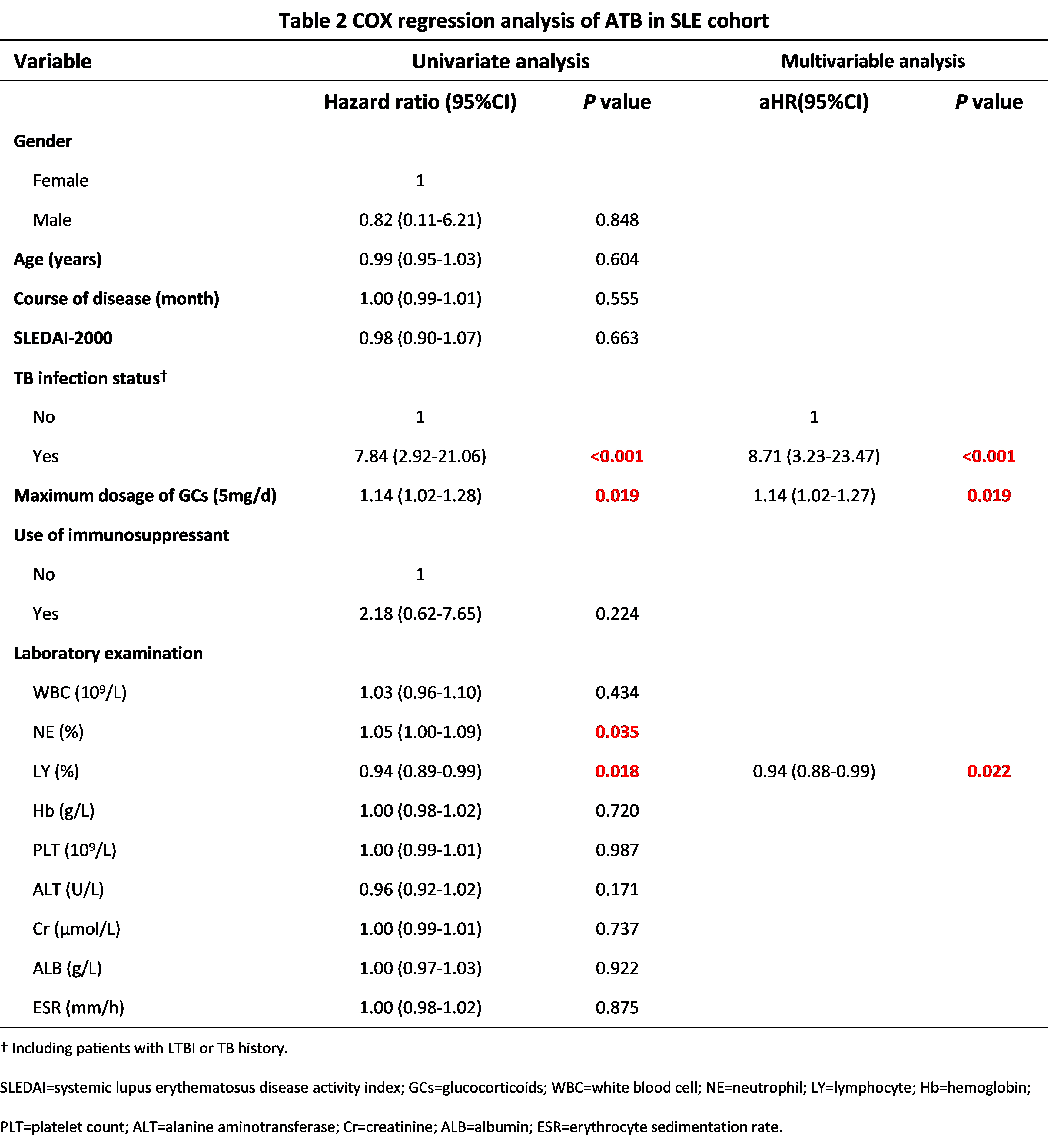 Table 2. COX regression analysis of ATB in SLE cohort
Table 2. COX regression analysis of ATB in SLE cohort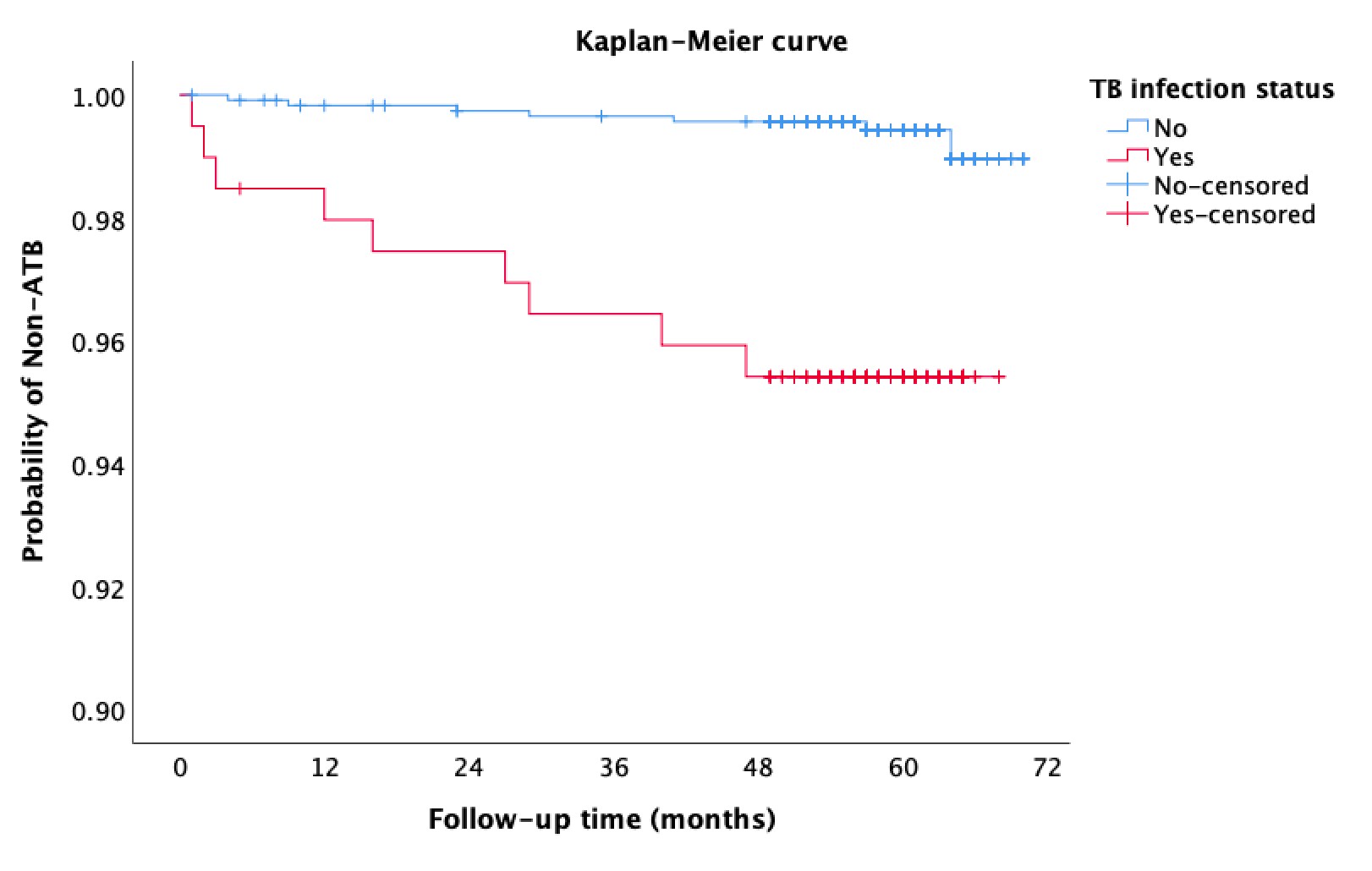 Figure 1. Incidence of ATB in patients with SLE according to TB infection status
Figure 1. Incidence of ATB in patients with SLE according to TB infection statusDisclosures: L. Zhang, None; x. zou, None; L. Xie, None; J. Liu, None; z. yang, None; q. cao, None; C. Li, None; X. Sun, None; F. ZHANG, None; Y. Zhao, None; X. Zeng, None; X. Liu, None.

