Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1443: Lymphadenopathy in Systemic Lupus Erythematosus: Clinical Characteristics and Prognostic Features
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Eleni Papachristodoulou, MD
Beth Israel Deaconess Medical Center
Watertown, MA, United States
Abstract Poster Presenter(s)
Eleni Papachristodoulou, Daniel Magliulo and Vasileios Kyttaris, Beth Israel Deaconess Medical Center, Boston, MA
Background/Purpose: Patients with SLE often develop lymphadenopathy (LAD), regarded as a relatively common manifestation of the disease. Its clinical significance has not yet been elucidated. We examined whether the presence of LAD and its different phenotypes is associated with other SLE clinical and laboratory manifestations.
Methods: We conducted a cross-sectional study of patients enrolled in the Beth Israel Deaconess Medical Center Lupus Cohort 2008-2022. The study was IRB approved. All patients met the 1997 ACR SLE criteria. Patients were categorized based on the presence and phenotype of LAD. Only patients in whom LAD could not be attributed to any other underlying cause were included. Demographic, clinical and laboratory parameters were compared between the groups. For statistical analysis x2 test for categorical variables and Student's t-test for continuous variables were conducted using SPSS 27.
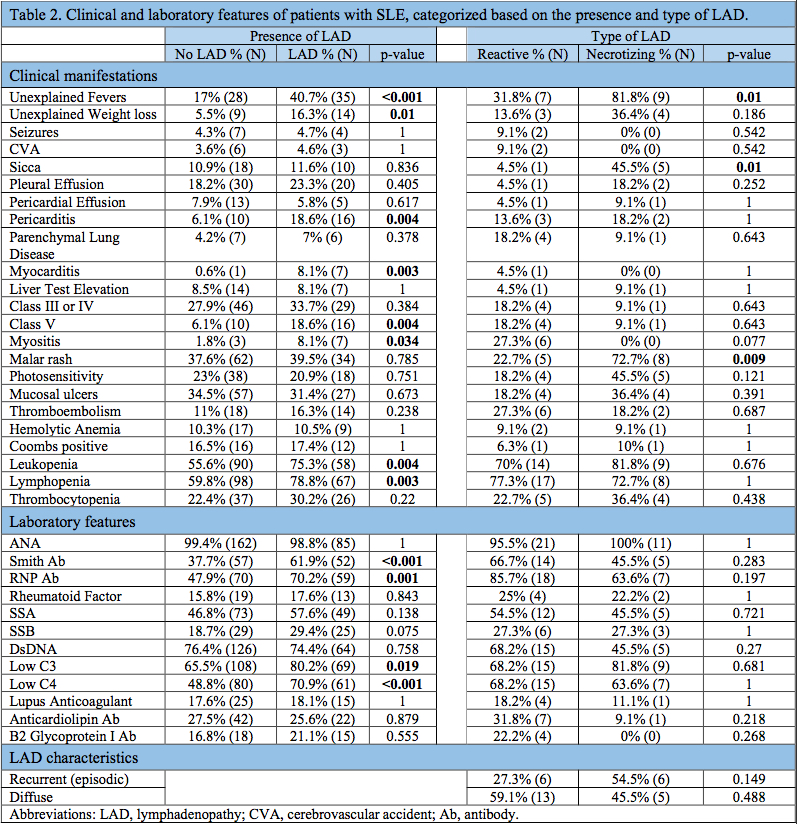
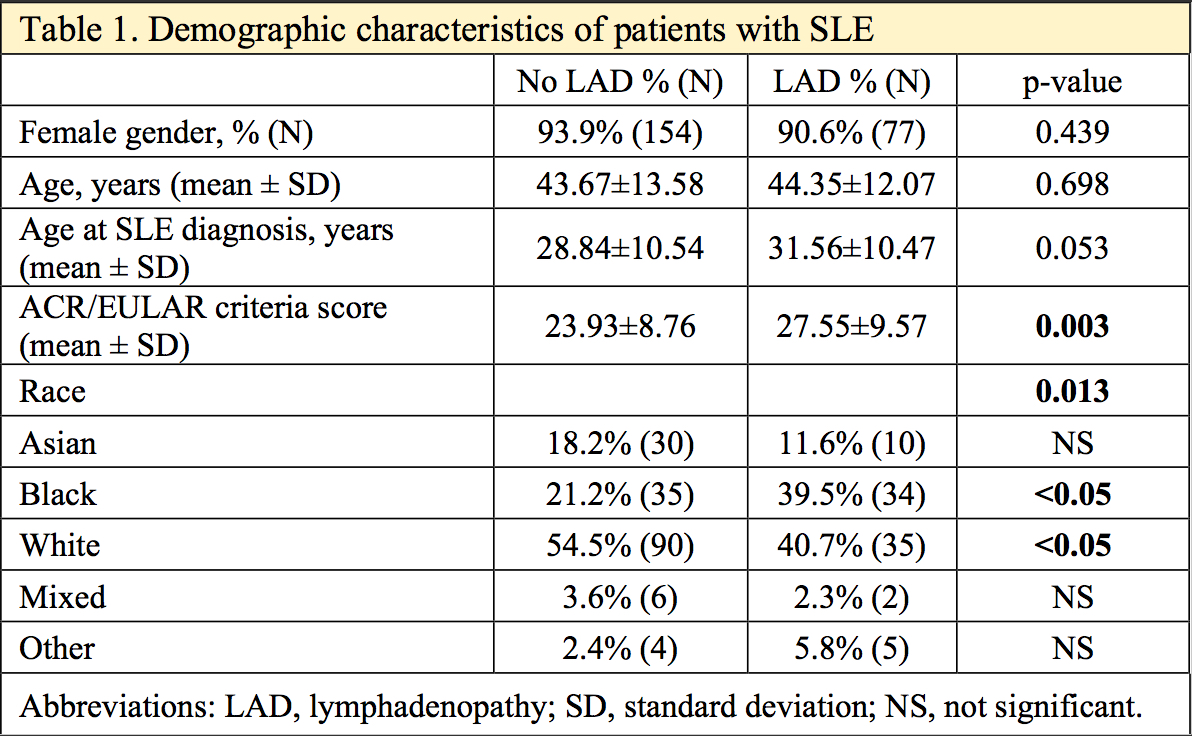
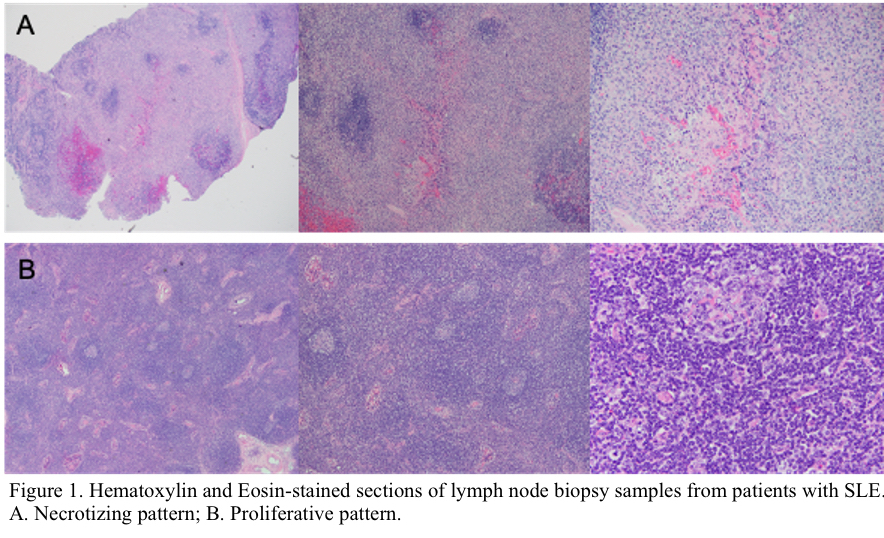
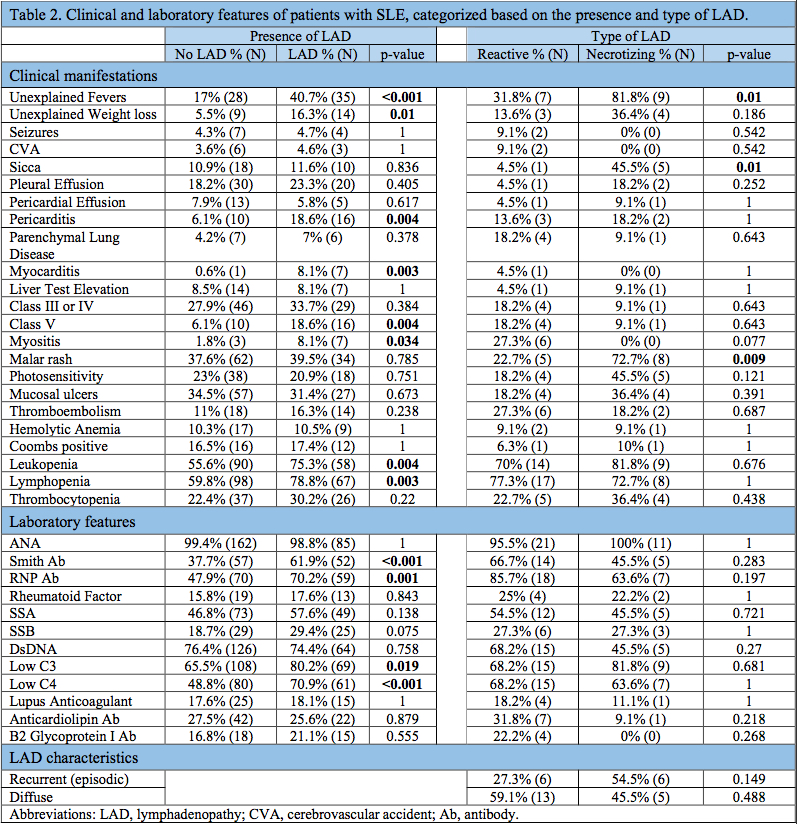
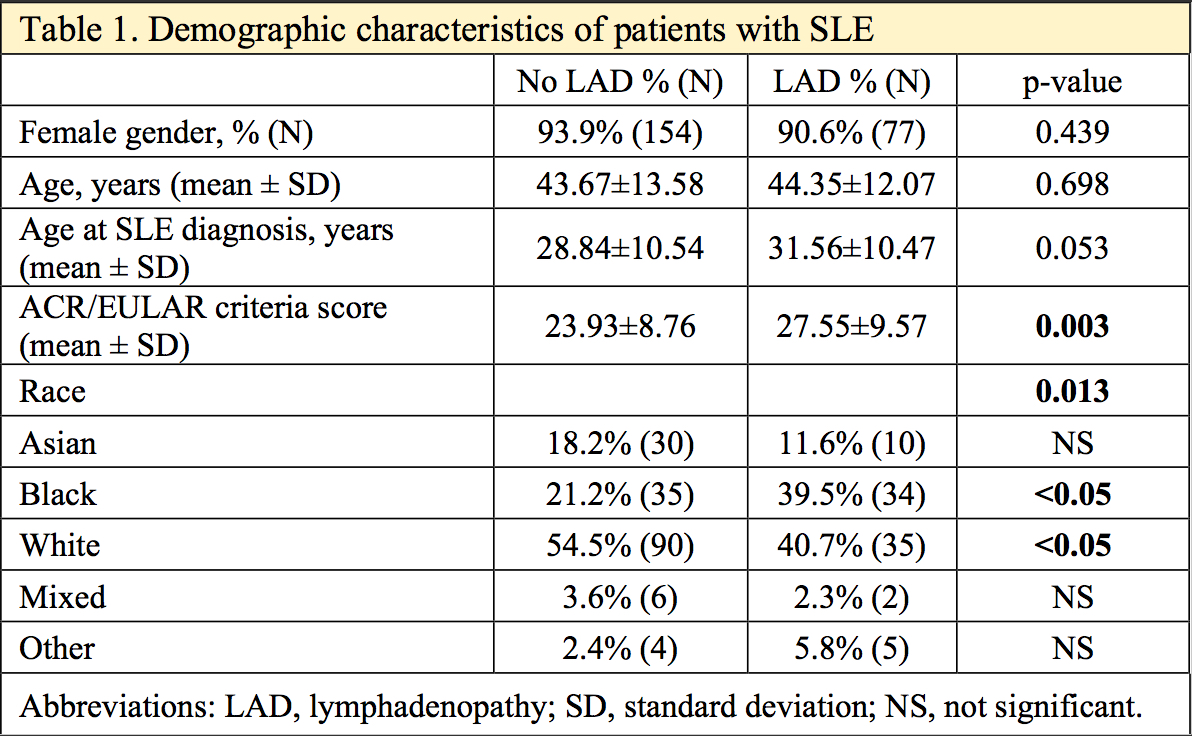
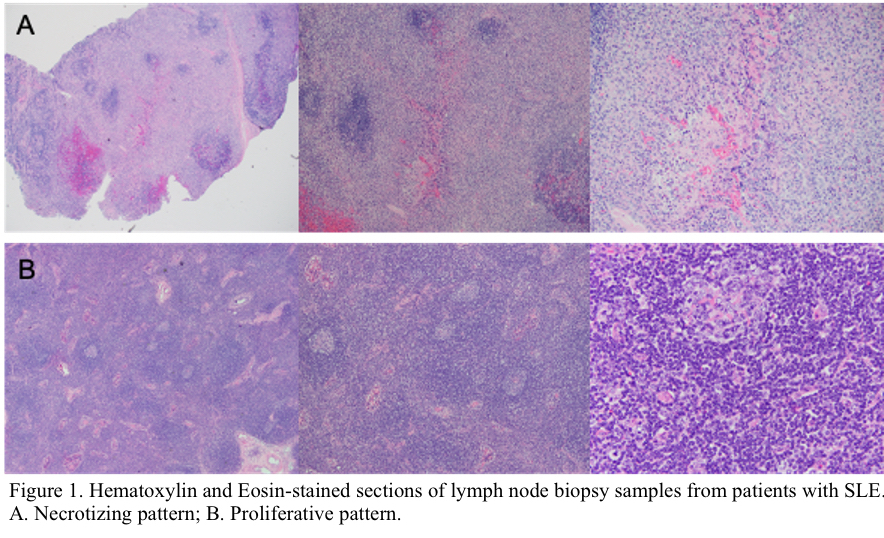
Results: 255 patients with SLE were included in the study, of whom 90 (35.29%) developed LAD; Lymphoma was the cause of LAD in three cases (3.33% of total LAD), one case was due to tuberculosis; these four subjects were excluded from this study. In total, 251 patients were included in the study (mean age 43.9±13 years, 92.8% female). 34.3% (86/251) of patients had at least one episode of LAD attributed to SLE. Patients with LAD had higher ACR/EULAR criteria score than patients who did not have lupus related LAD. Moreover, LAD was more common among black vs white patients (Table1). Clinical manifestations that presented significantly more frequently among patients with LAD included fever (40.7% vs 17%), weight loss (16.3% vs 5.5%), pericarditis (18.6% vs 6.1%), myocarditis (8.1% vs 0.6%), myositis (8.1% vs 1.8%), leukopenia (75.3% vs 55.6%), lymphopenia (78.8% vs 59.8%), and class V nephritis (18.6% vs 6.1%). Regarding serological markers, the presence of Smith Ab (61.9% vs 37.7%), RNP Ab (70.2% vs 47.9%), low C3 (80.2% vs 65.5%) and low C4 (70.9% vs 48.8%) were significantly more common in patients with LAD (Table 2). 38.4% (33/86) of the patients with LAD underwent lymph node biopsy, of which 66.7% (22) demonstrated a reactive/proliferative pattern and 33.3% (11) a necrotizing pattern (Figure1). When we compared the two phenotypes, we found that patients with necrotizing LAD were more likely to experience unexplained fevers, sicca and malar rash. No difference was identified regarding laboratory markers, the course or the extent of LAD between the two phenotypes. (Table 2).
Conclusion: In patients with SLE, the presence of LAD is common and associated with constitutional symptoms, myo/peri-carditis, cytopenias and nephritis, as well as with serological markers associated with increased disease activity. In this context, LAD may represent a manifestation of more active disease or an underlying process during the disease course. When comparing necrotizing vs reactive LAD, the presence of necrotic pattern in histology was associated with fever, malar rash, sicca but not worse prognosis. Lastly, in our cohort lymphoma was a rare but not infinitesimal cause of LAD (3.33% of LAD), pointing to the fact that although LAD is a common manifestation of SLE, biopsy is oftentimes needed to differentiate the two.
Disclosures: E. Papachristodoulou, None; D. Magliulo, None; V. Kyttaris, Exagen, Corbus Pharmaceuticals, Aurinia Pharmaceuticals, Scipher.
Background/Purpose: Patients with SLE often develop lymphadenopathy (LAD), regarded as a relatively common manifestation of the disease. Its clinical significance has not yet been elucidated. We examined whether the presence of LAD and its different phenotypes is associated with other SLE clinical and laboratory manifestations.
Methods: We conducted a cross-sectional study of patients enrolled in the Beth Israel Deaconess Medical Center Lupus Cohort 2008-2022. The study was IRB approved. All patients met the 1997 ACR SLE criteria. Patients were categorized based on the presence and phenotype of LAD. Only patients in whom LAD could not be attributed to any other underlying cause were included. Demographic, clinical and laboratory parameters were compared between the groups. For statistical analysis x2 test for categorical variables and Student's t-test for continuous variables were conducted using SPSS 27.
Results: 255 patients with SLE were included in the study, of whom 90 (35.29%) developed LAD; Lymphoma was the cause of LAD in three cases (3.33% of total LAD), one case was due to tuberculosis; these four subjects were excluded from this study. In total, 251 patients were included in the study (mean age 43.9±13 years, 92.8% female). 34.3% (86/251) of patients had at least one episode of LAD attributed to SLE. Patients with LAD had higher ACR/EULAR criteria score than patients who did not have lupus related LAD. Moreover, LAD was more common among black vs white patients (Table1). Clinical manifestations that presented significantly more frequently among patients with LAD included fever (40.7% vs 17%), weight loss (16.3% vs 5.5%), pericarditis (18.6% vs 6.1%), myocarditis (8.1% vs 0.6%), myositis (8.1% vs 1.8%), leukopenia (75.3% vs 55.6%), lymphopenia (78.8% vs 59.8%), and class V nephritis (18.6% vs 6.1%). Regarding serological markers, the presence of Smith Ab (61.9% vs 37.7%), RNP Ab (70.2% vs 47.9%), low C3 (80.2% vs 65.5%) and low C4 (70.9% vs 48.8%) were significantly more common in patients with LAD (Table 2). 38.4% (33/86) of the patients with LAD underwent lymph node biopsy, of which 66.7% (22) demonstrated a reactive/proliferative pattern and 33.3% (11) a necrotizing pattern (Figure1). When we compared the two phenotypes, we found that patients with necrotizing LAD were more likely to experience unexplained fevers, sicca and malar rash. No difference was identified regarding laboratory markers, the course or the extent of LAD between the two phenotypes. (Table 2).
Conclusion: In patients with SLE, the presence of LAD is common and associated with constitutional symptoms, myo/peri-carditis, cytopenias and nephritis, as well as with serological markers associated with increased disease activity. In this context, LAD may represent a manifestation of more active disease or an underlying process during the disease course. When comparing necrotizing vs reactive LAD, the presence of necrotic pattern in histology was associated with fever, malar rash, sicca but not worse prognosis. Lastly, in our cohort lymphoma was a rare but not infinitesimal cause of LAD (3.33% of LAD), pointing to the fact that although LAD is a common manifestation of SLE, biopsy is oftentimes needed to differentiate the two.
Disclosures: E. Papachristodoulou, None; D. Magliulo, None; V. Kyttaris, Exagen, Corbus Pharmaceuticals, Aurinia Pharmaceuticals, Scipher.

