Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1567: Refractory Macular Edema Due to Behçet's Disease. Multicenter Comparative Study of Adalimumab and Certolizumab Pegol
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JM
Jose Luis Martin-Varillas, MD
Hospital Laredo
Laredo, Spain
Abstract Poster Presenter(s)
José Luis Martín-Varillas1, Lara Sánchez-Bilbao2, Vanesa Calvo Río3, Alf Adán4, Inés Hernanz Rodríguez4, Miguel Cordero Coma5, David Díaz Valle6, Patricia Fanlo7, Juan Ramón de Dios8, A. Garcia-Aparicio9, Sergio Rodriguez Montero10, Vega Jovani Casano11, Patricia Moya Alvarado12, eva Peña Sainz-Pardo13, José Luis Hernández2 and Ricardo Blanco14, 1Hospital de Laredo, Laredo, Cantabria, Spain, 2Hospital Universitario Marqués de Valdecilla, Santander, Spain, 3Valdecilla Hospital, Santander, Spain, 4H. Clinic, Barcelona, Spain, 5Hospital de León, León, Spain, 6Hospital Clínico San Carlos, Madrid, Spain, 7Complejo Hospitalario de Navarra, Navarra, Spain, 8Hospital de Araba, Araba, Spain, 9Hospital Universitario de Toledo, Toledo, Spain, 10Virgen de Valme University Hospital, Sevilla, Spain, 11National Health system, Alicante, Spain, 12Hospital Parc Tauli, Barcelona, Spain, 13Hospital Universitario 12 de Octubre, Madrid, Spain, 14Hospital Universitario Marqués de Valdecilla, IDIVAL, Santander, Spain
Background/Purpose: Cystoid Macular Edema (CME) is the leading cause of blindness in non-infectious uveitis. Behçet's disease (BD) is one of the diseases most frequently associated with CME. Our aims wereto compare the efficacy and safety of Certolizumab Pegol (CZP) and Adalimumab (ADA) in CME due to BD refractory to conventional therapy.
Methods: multicenter study of patients with CME secondary to BD refractory to glucocorticoids (GC) and at least 1 conventional immunosuppressant. All patients had CME (OCT >300µ) at baseline. Efficacy was assessed with the following ocular parameters: macular thickness (µm), visual acuity (BCVA) and GC-sparing effect. The efficacy of CZP vs. ADA was compared between the baseline visit, 1st and 6th month, and 1st and 2nd year. Statistical analysis was performed with IBM SPSS Statistics v.23.
Results: We studied 21 patients/38 affected eyes were studied. 10 patients were treated with CZP (200 mg c/2 weeks) and 11 with ADA (loading dose of 80 mg and subsequently 40 mg c/2 weeks). No statistically significant baseline differences were observed in both groups (CZP vs. ADA) in sex (♂/♀; 3/7 vs 5/6; p=0.65) and mean age (36.1±8.0 vs 42.2±8.6; p=0.10). However, CZP group was more severe with a longer time between EB diagnosis and biologic initiation (91.6±71.4 vs 34.4±21.3 months, p=0.02), and a greater median [IQR] number of previous biologic drugs (2 [0.75-3] vs 0 [0-0]). In CZP group, 8 patients were previously treated with ADA. Combined therapy with conventional DMARDs was used with ADA in 81.8% vs. 18.2% of CZP patients. Regarding the efficacy outcomes analyzed, a rapid and maintained improvement in macular thickness, measured by OCT, was observed after 2 years of follow-up in both groups with no statistically significant differences between them (TABLE). Improvement in visual acuity and a GC-sparing effect was also observed (TABLE). No serious adverse events were observed in either group.
Conclusion: Our study suggests that both CZP and ADA are effective in the treatment of CME due to BD refractory to conventional treatment. CZP was equally effective despite most patients were refractory to ADA.
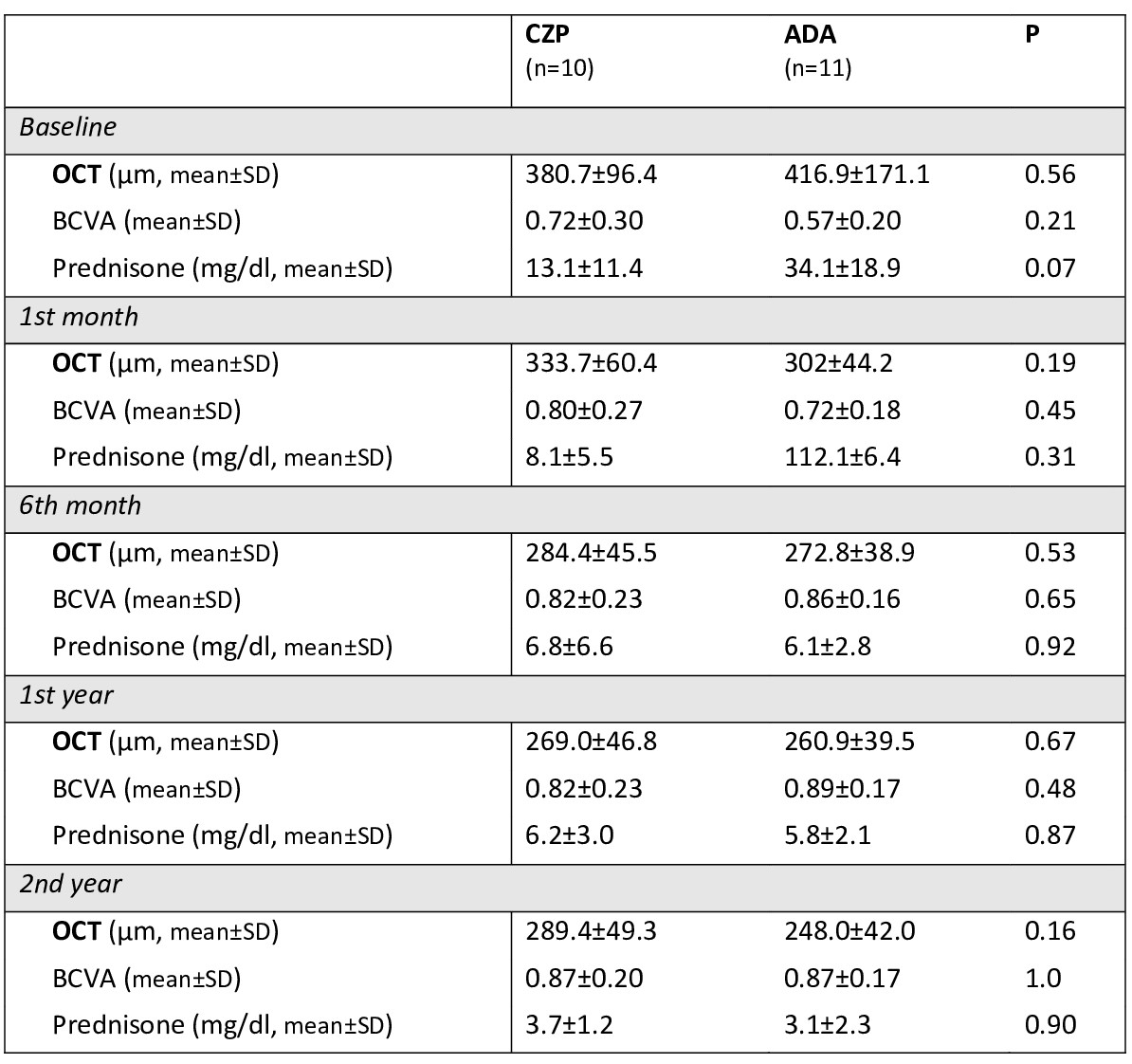 TABLE. main ocular parameters compared in the CZP-treated group vs. ADA-treated group.
TABLE. main ocular parameters compared in the CZP-treated group vs. ADA-treated group.
Disclosures: J. Martín-Varillas, AbbVie/Abbott, Pfizer, Janssen, UCB, Celgene; L. Sánchez-Bilbao, Eli Lilly; V. Calvo Río, AbbVie/Abbott, Eli Lilly, Merck/MSD, UCB; A. Adán, None; I. Hernanz Rodríguez, None; M. Cordero Coma, None; D. Díaz Valle, None; P. Fanlo, None; J. de Dios, None; A. Garcia-Aparicio, None; S. Rodriguez Montero, None; V. Jovani Casano, None; P. Moya Alvarado, None; e. Peña Sainz-Pardo, None; J. Hernández, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi.
Background/Purpose: Cystoid Macular Edema (CME) is the leading cause of blindness in non-infectious uveitis. Behçet's disease (BD) is one of the diseases most frequently associated with CME. Our aims wereto compare the efficacy and safety of Certolizumab Pegol (CZP) and Adalimumab (ADA) in CME due to BD refractory to conventional therapy.
Methods: multicenter study of patients with CME secondary to BD refractory to glucocorticoids (GC) and at least 1 conventional immunosuppressant. All patients had CME (OCT >300µ) at baseline. Efficacy was assessed with the following ocular parameters: macular thickness (µm), visual acuity (BCVA) and GC-sparing effect. The efficacy of CZP vs. ADA was compared between the baseline visit, 1st and 6th month, and 1st and 2nd year. Statistical analysis was performed with IBM SPSS Statistics v.23.
Results: We studied 21 patients/38 affected eyes were studied. 10 patients were treated with CZP (200 mg c/2 weeks) and 11 with ADA (loading dose of 80 mg and subsequently 40 mg c/2 weeks). No statistically significant baseline differences were observed in both groups (CZP vs. ADA) in sex (♂/♀; 3/7 vs 5/6; p=0.65) and mean age (36.1±8.0 vs 42.2±8.6; p=0.10). However, CZP group was more severe with a longer time between EB diagnosis and biologic initiation (91.6±71.4 vs 34.4±21.3 months, p=0.02), and a greater median [IQR] number of previous biologic drugs (2 [0.75-3] vs 0 [0-0]). In CZP group, 8 patients were previously treated with ADA. Combined therapy with conventional DMARDs was used with ADA in 81.8% vs. 18.2% of CZP patients. Regarding the efficacy outcomes analyzed, a rapid and maintained improvement in macular thickness, measured by OCT, was observed after 2 years of follow-up in both groups with no statistically significant differences between them (TABLE). Improvement in visual acuity and a GC-sparing effect was also observed (TABLE). No serious adverse events were observed in either group.
Conclusion: Our study suggests that both CZP and ADA are effective in the treatment of CME due to BD refractory to conventional treatment. CZP was equally effective despite most patients were refractory to ADA.
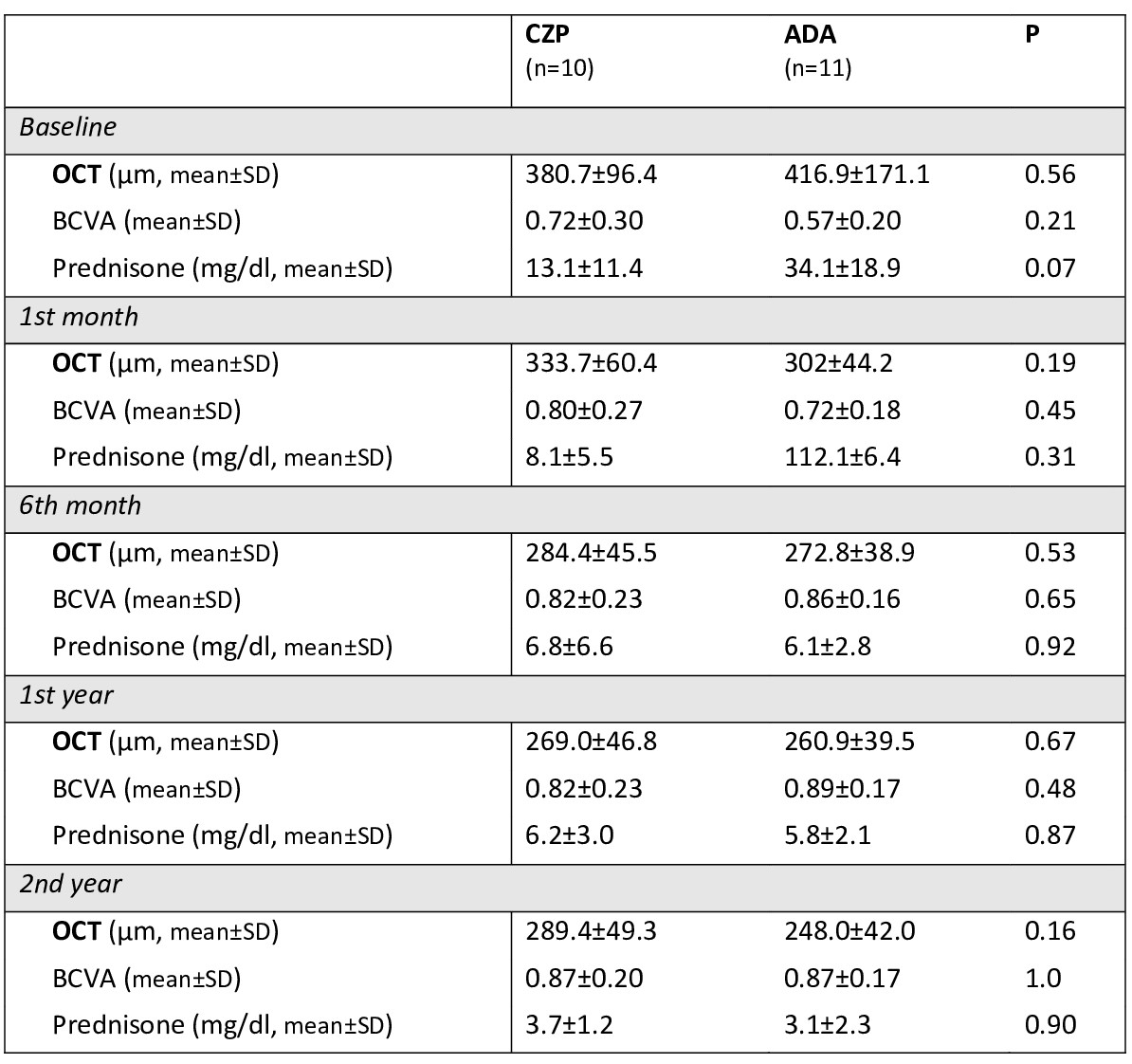 TABLE. main ocular parameters compared in the CZP-treated group vs. ADA-treated group.
TABLE. main ocular parameters compared in the CZP-treated group vs. ADA-treated group.Disclosures: J. Martín-Varillas, AbbVie/Abbott, Pfizer, Janssen, UCB, Celgene; L. Sánchez-Bilbao, Eli Lilly; V. Calvo Río, AbbVie/Abbott, Eli Lilly, Merck/MSD, UCB; A. Adán, None; I. Hernanz Rodríguez, None; M. Cordero Coma, None; D. Díaz Valle, None; P. Fanlo, None; J. de Dios, None; A. Garcia-Aparicio, None; S. Rodriguez Montero, None; V. Jovani Casano, None; P. Moya Alvarado, None; e. Peña Sainz-Pardo, None; J. Hernández, None; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi.

