Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1469: Risk Factors for Herpes Zoster Among Patients with Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CS
Caroline Spitznagel, MD
Medical University of South Carolina
Charleston, SC, United States
Abstract Poster Presenter(s)
Caroline Spitznagel, Fedelis Mutiso, Jim Oates and Diane Kamen, Medical University of South Carolina, Charleston, SC
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have a higher prevalence and incidence of herpes zoster (HZ) compared with the general population. Our study was to determine the current burden of HZ and describe risk factors for its development among patients with SLE.
Methods: Data was obtained from an ongoing IRB-approved longitudinal registry of patients with SLE and non-SLE controls at the Medical University of South Carolina, including demographics, medical history, and SLE-related damage (SLICC Damage Index). Patient-reported history of HZ was confirmed by electronic medical record review. Descriptive analyses, Pearson's chi-squared testing, two-sample t-tests, and multivariable logistic regression were performed as appropriate.
Results: The study population included 726 registry participants with SLE, of whom 656 (90.36%) were female, 541 (74.52%) were Black, and 21 (2.89%) were Hispanic. In our study population, 143 (19.70%) SLE patients reported a history of HZ and 583 (80.30%) had no known history of HZ. Mean age of onset of SLE was similar between patients with and without a history of HZ, with mean ages 31.71 (+/- 14.23) and 31.17 (+/- 13.94) respectively (Table 1). Chi-square analysis revealed patients with a history of zoster were more likely to have any disease damage from SLE (SLICC-DI > 0) compared with patients who did not have a history of zoster (75.53% vs. 59.01%, p-value < 0.01). Patients with a history of zoster were also more likely to have high disease damage (SLICC-DI > 1) (54.93% vs 38.42%, p-value < 0.01). Female gender was also associated with HZ risk (95.10% vs 89.19%, p-value 0.03). There was no significant difference between HZ rates in Black vs. Non-Black patients (71.33% vs. 75.30%, p-value 0.31) or Hispanic vs. Non-Hispanic patients (2.80% vs 2.92%, p-value 0.94). We did not see a significant association between HZ and the individual SLE classification criteria (Table 2). Using logistic regression modeling, the odds of having a history of HZ with any SLE damage, adjusting for current age, gender, and race finds a significant odds ratio of 2.03 (p-value < 0.01, 95% CI 1.32-3.11).
Conclusion: Despite a lower risk of HZ among Blacks in the general population, our study found similar HZ prevalence between Blacks and non-Blacks. Additionally, our study found a significant relationship between higher SLE disease damage and HZ, consistent with findings in other SLE cohorts. Our results emphasize the need to identify HZ early among patients with dark skin, and promote HZ vaccination among those at highest risk.
.jpg) Table 1: Demographic information
Table 1: Demographic information
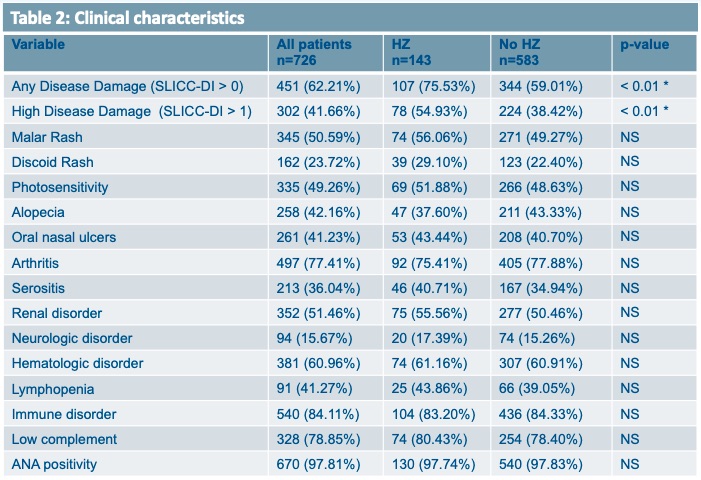 Table 2: Clinical characteristics
Table 2: Clinical characteristics
Disclosures: C. Spitznagel, None; F. Mutiso, None; J. Oates, None; D. Kamen, None.
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have a higher prevalence and incidence of herpes zoster (HZ) compared with the general population. Our study was to determine the current burden of HZ and describe risk factors for its development among patients with SLE.
Methods: Data was obtained from an ongoing IRB-approved longitudinal registry of patients with SLE and non-SLE controls at the Medical University of South Carolina, including demographics, medical history, and SLE-related damage (SLICC Damage Index). Patient-reported history of HZ was confirmed by electronic medical record review. Descriptive analyses, Pearson's chi-squared testing, two-sample t-tests, and multivariable logistic regression were performed as appropriate.
Results: The study population included 726 registry participants with SLE, of whom 656 (90.36%) were female, 541 (74.52%) were Black, and 21 (2.89%) were Hispanic. In our study population, 143 (19.70%) SLE patients reported a history of HZ and 583 (80.30%) had no known history of HZ. Mean age of onset of SLE was similar between patients with and without a history of HZ, with mean ages 31.71 (+/- 14.23) and 31.17 (+/- 13.94) respectively (Table 1). Chi-square analysis revealed patients with a history of zoster were more likely to have any disease damage from SLE (SLICC-DI > 0) compared with patients who did not have a history of zoster (75.53% vs. 59.01%, p-value < 0.01). Patients with a history of zoster were also more likely to have high disease damage (SLICC-DI > 1) (54.93% vs 38.42%, p-value < 0.01). Female gender was also associated with HZ risk (95.10% vs 89.19%, p-value 0.03). There was no significant difference between HZ rates in Black vs. Non-Black patients (71.33% vs. 75.30%, p-value 0.31) or Hispanic vs. Non-Hispanic patients (2.80% vs 2.92%, p-value 0.94). We did not see a significant association between HZ and the individual SLE classification criteria (Table 2). Using logistic regression modeling, the odds of having a history of HZ with any SLE damage, adjusting for current age, gender, and race finds a significant odds ratio of 2.03 (p-value < 0.01, 95% CI 1.32-3.11).
Conclusion: Despite a lower risk of HZ among Blacks in the general population, our study found similar HZ prevalence between Blacks and non-Blacks. Additionally, our study found a significant relationship between higher SLE disease damage and HZ, consistent with findings in other SLE cohorts. Our results emphasize the need to identify HZ early among patients with dark skin, and promote HZ vaccination among those at highest risk.
.jpg) Table 1: Demographic information
Table 1: Demographic information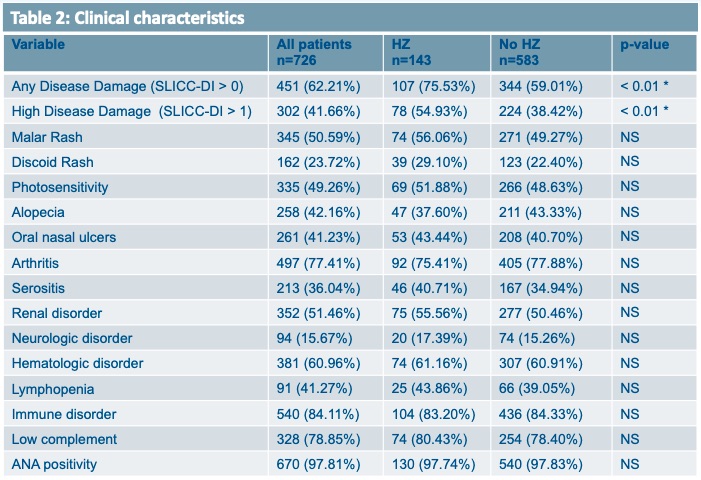 Table 2: Clinical characteristics
Table 2: Clinical characteristicsDisclosures: C. Spitznagel, None; F. Mutiso, None; J. Oates, None; D. Kamen, None.

