Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0477: Can Beta-blockers Prevent Aortic Dilation in Patients with Giant Cell Arteritis and Large Vessel Vasculitis?
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- Hd
Hubert de Boysson, MD, PhD
Caen university Hospital
Caen, France
Abstract Poster Presenter(s)
Hubert De Boysson1, Anael DUMONT2, Samuel DESHAYES2, Alexandre Nguyen2 and Achille Aouba1, 1Department of Internal Medicine, UR4650 PSIR, Normandie Univ, UNICAEN, CHU de Caen Normandie, Caen, France, 2Caen University Hospital, Caen, France
Background/Purpose: We analyzed whether the use of beta-blockers in addition to conventional care in patients with Giant cell arteritis (GCA) and large vessel vasculitis (LVV) can help reduce the risk of aortic dilatation.
Methods: We conducted a monocentric retrospective study including 65 consecutive patients with GCA-related LVV who all underwent a control of aorta morphology during follow-up. We created a vascular score ranging from 0, i.e. no cardiovascular (CV) risk factor or event, to 1, i.e. multiple CV risk factors and events, to quantify the impact of CV risk factors and/or previous CV events on the prescription of beta-blockers, as well as on the risk of aortic dilation development.
Results: The characteristics at diagnosis of the 65 GCA patients with LVV are indicated in Table 1. At the time of GCA diagnosis, 15 (23%) patients took beta-blockers which they continued thereafter. The vascular score was significantly higher in patients who received beta-blockers (0.25 [0.125–0.625] in patients with beta-blockers vs. 0.125 [0–0.625] in patients without, p< 0.0001; Table 1). No difference regarding GCA characteristics and treatment was observed when comparing patients with and without beta-blockers (Table 1).
The median follow-up was 91 [25–163] months in GCA patients with beta-blockers, and 61 [14–248] months in GCA patients without beta-blockers (p=0.13). The last control imaging of the aorta was performed in all patients 26 [6–144] months after the first imaging.
A new aortic dilation, not observed on the first imaging, was detected in 15 (23%) patients and none of them were receiving beta-blockers. Survival without new aortic dilation in patients with and without beta-blockers is shown in Figure 1 (log-rank: p=0.009). These 15 patients did not exhibit a higher vascular score than patients without aortic dilation (0.125 [0–0.375] in patients who developed an aortic dilation vs. 0.125 [0–0.625] in those without aortic dilation, p=0.38). Aortic dilation was detected 38 [6–120] months after the first imaging and developed on an aortic segment which was inflamed on the first imaging, of the thoracic section in 14 and of the abdominal section in 1.
The death rate was not different in patients with and without beta-blockers, as well as in patients with and without aortic dilation.
Conclusion: This study is the first to suggest that beta-blockers in addition to conventional care in patients with GCA and LVV may help reduce the risk of aortic dilatation during follow-up, as in non-inflammatory aortic diseases.
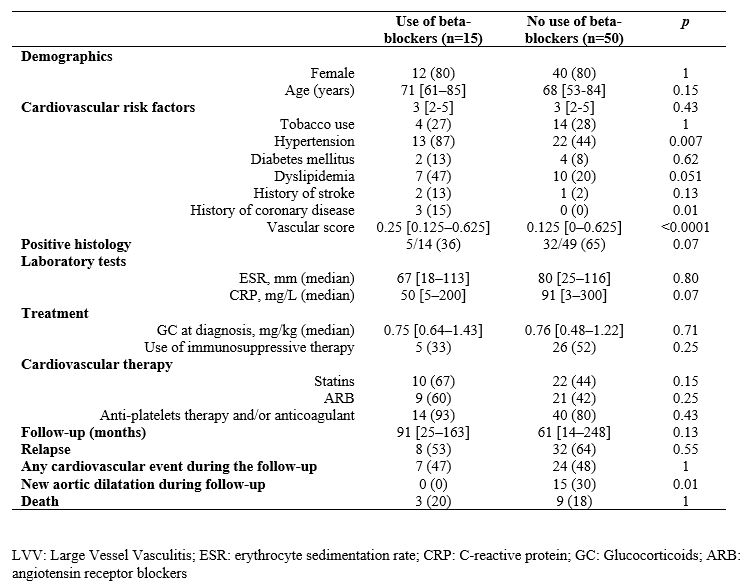 Table 1. Characteristics at baseline and during the follow-up of GCA patients with large vessel vasculitis, with and without beta-blockers
Table 1. Characteristics at baseline and during the follow-up of GCA patients with large vessel vasculitis, with and without beta-blockers
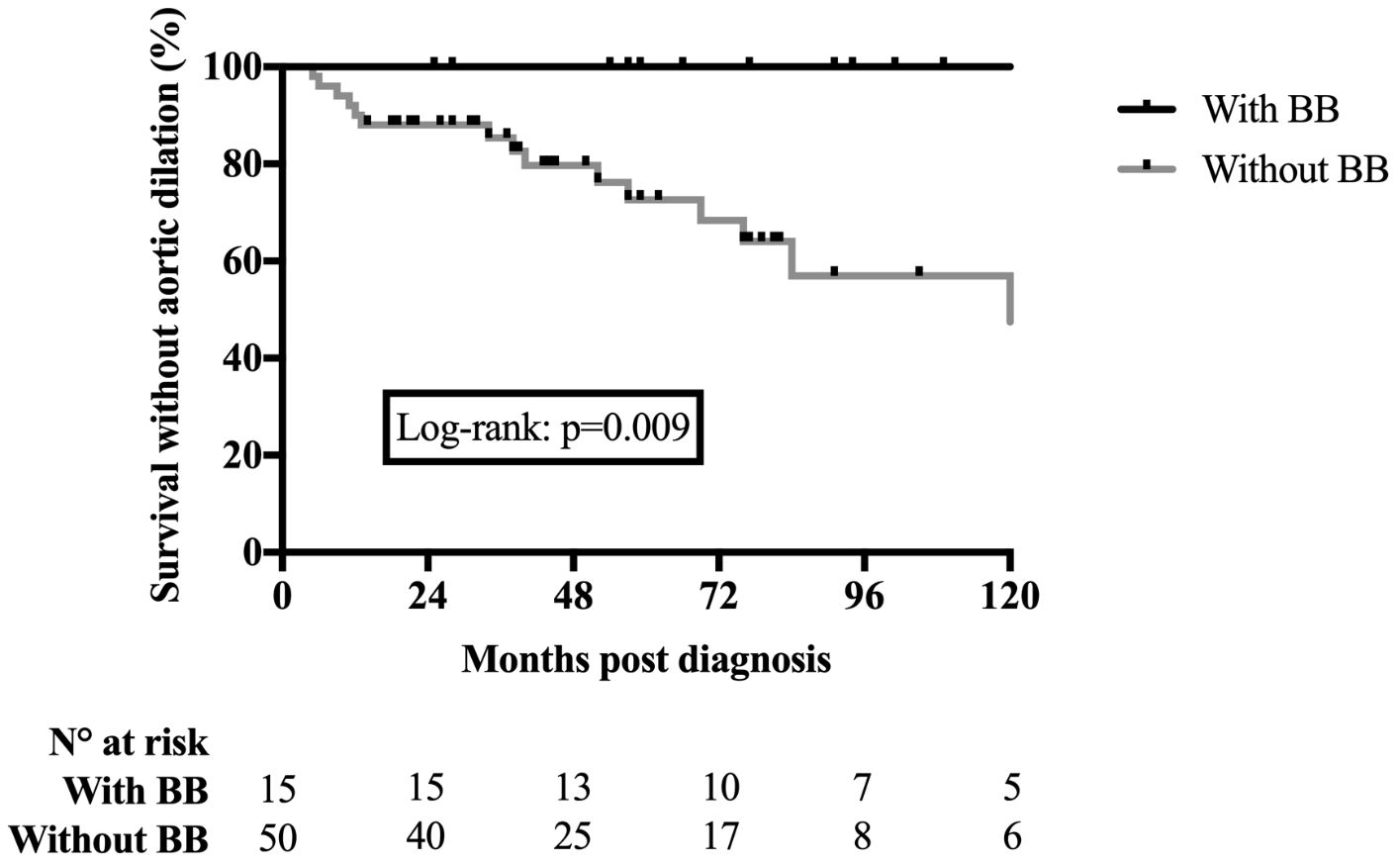 Figure 1. Survival without aortic dilation in patients with GCA-related large vessel vasculitis, with or without beta-blockers.
Figure 1. Survival without aortic dilation in patients with GCA-related large vessel vasculitis, with or without beta-blockers.
Disclosures: H. De Boysson, None; A. DUMONT, None; S. DESHAYES, None; A. Nguyen, SANOFI GENZYME; A. Aouba, Roche.
Background/Purpose: We analyzed whether the use of beta-blockers in addition to conventional care in patients with Giant cell arteritis (GCA) and large vessel vasculitis (LVV) can help reduce the risk of aortic dilatation.
Methods: We conducted a monocentric retrospective study including 65 consecutive patients with GCA-related LVV who all underwent a control of aorta morphology during follow-up. We created a vascular score ranging from 0, i.e. no cardiovascular (CV) risk factor or event, to 1, i.e. multiple CV risk factors and events, to quantify the impact of CV risk factors and/or previous CV events on the prescription of beta-blockers, as well as on the risk of aortic dilation development.
Results: The characteristics at diagnosis of the 65 GCA patients with LVV are indicated in Table 1. At the time of GCA diagnosis, 15 (23%) patients took beta-blockers which they continued thereafter. The vascular score was significantly higher in patients who received beta-blockers (0.25 [0.125–0.625] in patients with beta-blockers vs. 0.125 [0–0.625] in patients without, p< 0.0001; Table 1). No difference regarding GCA characteristics and treatment was observed when comparing patients with and without beta-blockers (Table 1).
The median follow-up was 91 [25–163] months in GCA patients with beta-blockers, and 61 [14–248] months in GCA patients without beta-blockers (p=0.13). The last control imaging of the aorta was performed in all patients 26 [6–144] months after the first imaging.
A new aortic dilation, not observed on the first imaging, was detected in 15 (23%) patients and none of them were receiving beta-blockers. Survival without new aortic dilation in patients with and without beta-blockers is shown in Figure 1 (log-rank: p=0.009). These 15 patients did not exhibit a higher vascular score than patients without aortic dilation (0.125 [0–0.375] in patients who developed an aortic dilation vs. 0.125 [0–0.625] in those without aortic dilation, p=0.38). Aortic dilation was detected 38 [6–120] months after the first imaging and developed on an aortic segment which was inflamed on the first imaging, of the thoracic section in 14 and of the abdominal section in 1.
The death rate was not different in patients with and without beta-blockers, as well as in patients with and without aortic dilation.
Conclusion: This study is the first to suggest that beta-blockers in addition to conventional care in patients with GCA and LVV may help reduce the risk of aortic dilatation during follow-up, as in non-inflammatory aortic diseases.
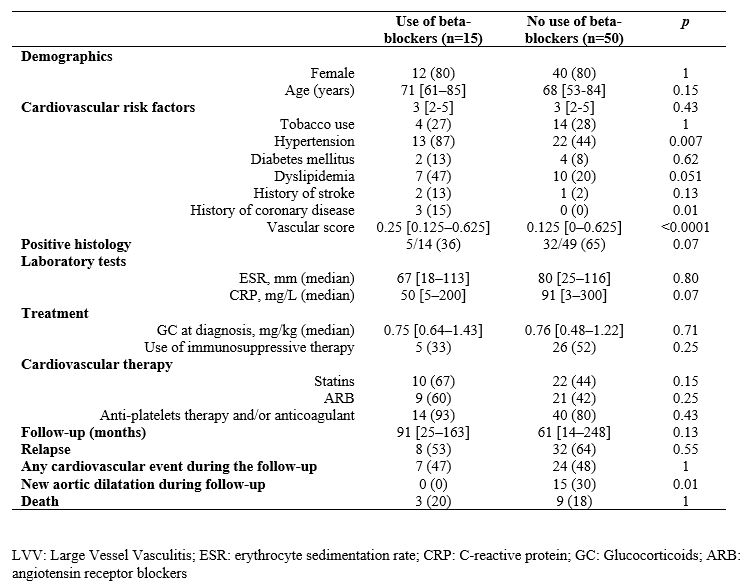 Table 1. Characteristics at baseline and during the follow-up of GCA patients with large vessel vasculitis, with and without beta-blockers
Table 1. Characteristics at baseline and during the follow-up of GCA patients with large vessel vasculitis, with and without beta-blockers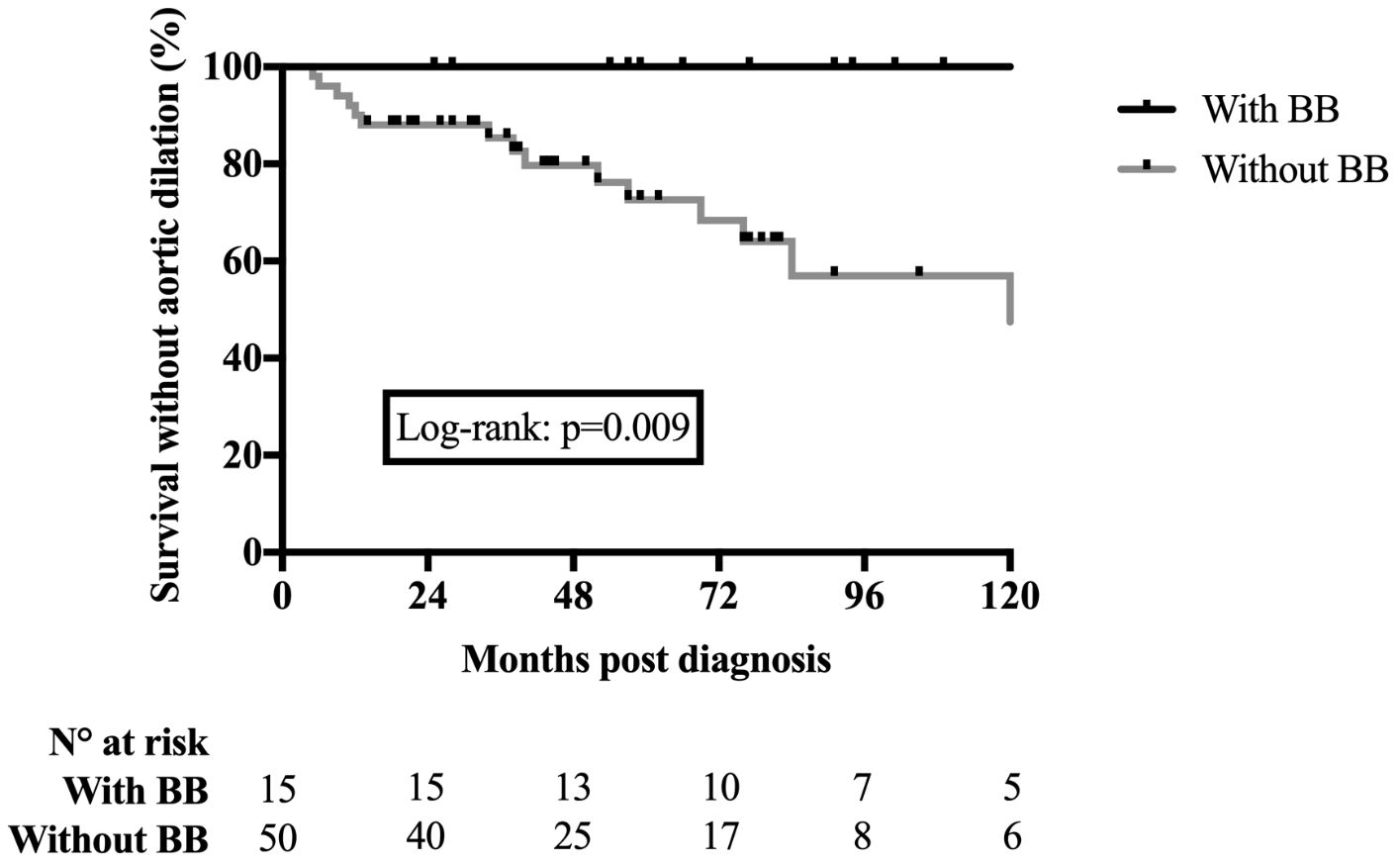 Figure 1. Survival without aortic dilation in patients with GCA-related large vessel vasculitis, with or without beta-blockers.
Figure 1. Survival without aortic dilation in patients with GCA-related large vessel vasculitis, with or without beta-blockers.Disclosures: H. De Boysson, None; A. DUMONT, None; S. DESHAYES, None; A. Nguyen, SANOFI GENZYME; A. Aouba, Roche.

