Back
Poster Session A
Vasculitis
Session: (0432–0457) Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
0445: Cardiovascular Burden in Patients with ANCA-Associated and Non-ANCA Associated Vasculitis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
- AA
Ana B Arevalo, MD
University of Chicago
Chicago, IL, United States
Abstract Poster Presenter(s)
Ana Arevalo1, Palak Shah2, Harshvardhan Zala3, Faris Haddadin4, Monil Majmundar5 and Andrea Ramirez Gomez1, 1University of Chicago, Chicago, IL, 2Metropolitan Hospital Center, New York Medical College, New York, NY, 3Icahn School of Medicine at Mount Sinai, New York, NY, 4Baylor College of Medicine, Houston, TX, 5University of Kansas Medical Center, Kansas City, KS
Background/Purpose: Several studies have reported that patients with ANCA-associated vasculitis (AAV) are at increased risk of cardiovascular complications from accelerated atherosclerosis with an excess cardiovascular (CV) risk of 65%. HTN and diabetes mellitus (DM) are two of the most reported treatment-related complications observed at long-term follow-up. However, the risk of CV disease is greater in AAV and cannot be explained through traditional CV risk factors alone. ANCA are harmful antibodies that are directly involved in blood vessel damage through neutrophil and complement cascade activation, but it is unclear if they are directly responsible for the higher rate of CV complications in AAV. Therefore, we aimed to compare ANCA-associated and non-ANCA-associated vasculitis and their associations with mortality and CV outcomes.
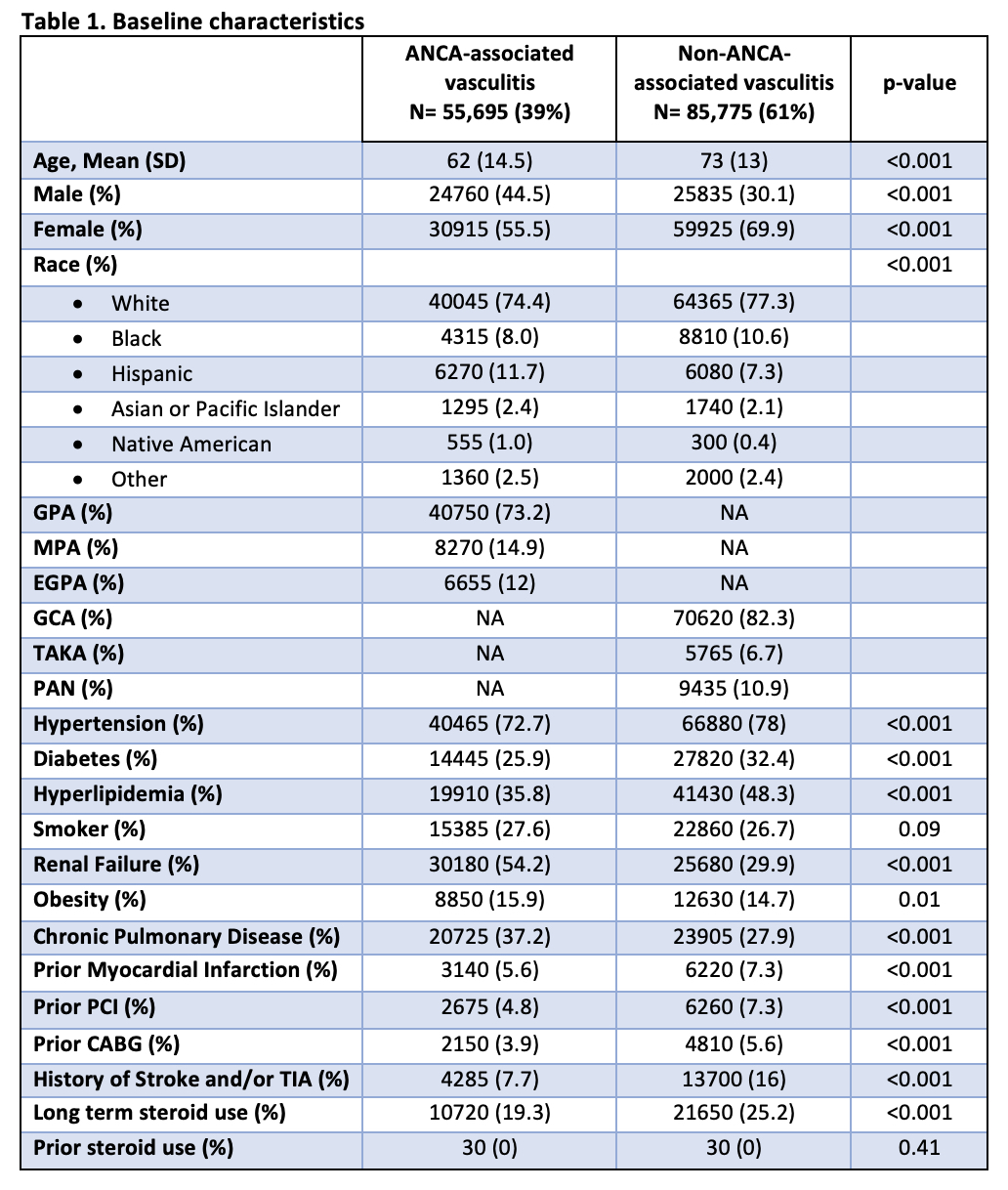
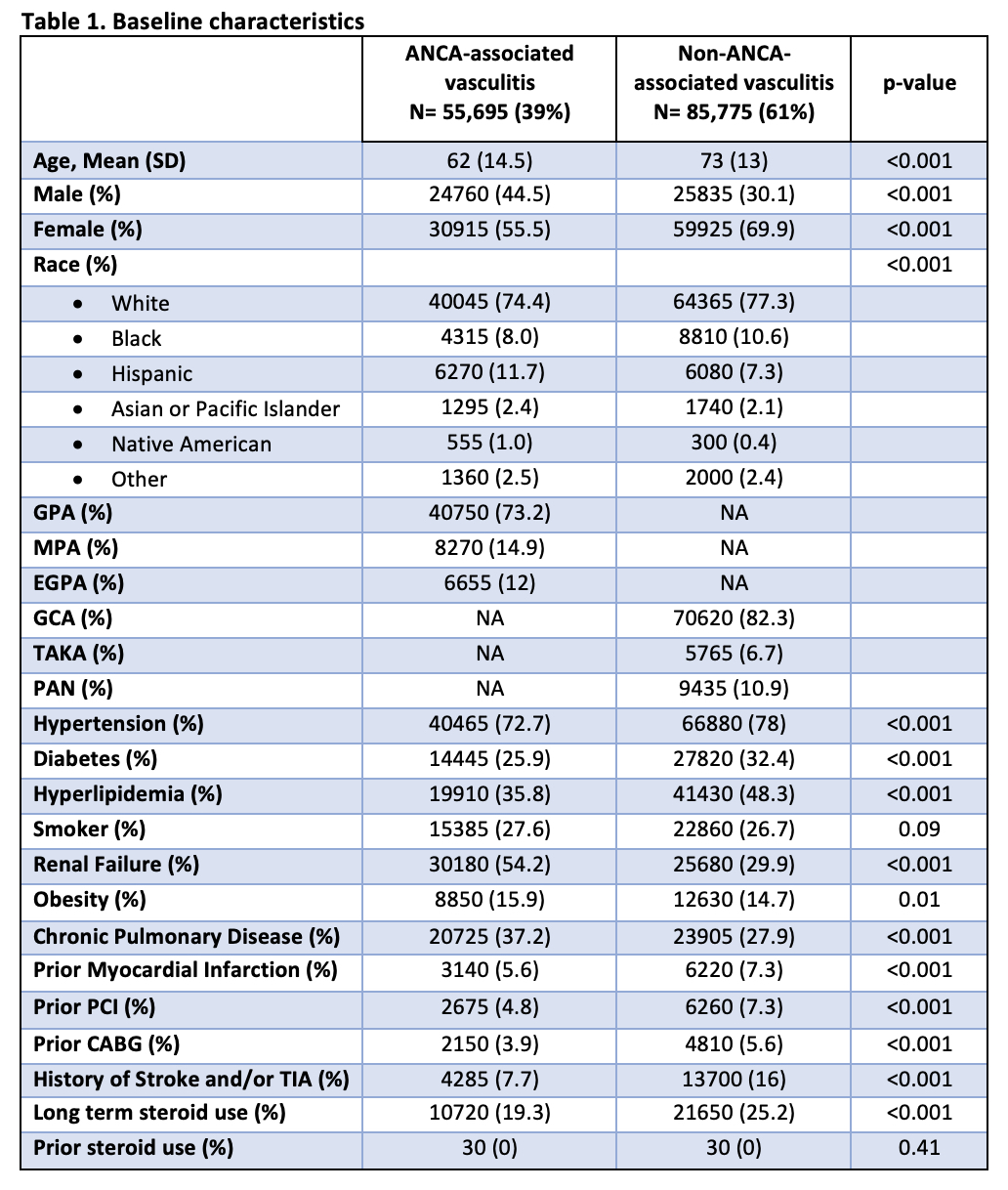
Methods: In this retrospective cohort study, we identified patients with ANCA-associated and non-ANCA-associated vasculitis based on ICD-10 codes, using the Nationwide Inpatient Sample database (NIS) from 2016 to 2019. We included all-cause mortality, atrial fibrillation (Afib), ST-elevation (STEMI) and non-ST elevation myocardial infarction (NSTEMI), heart failure (HF), cerebrovascular accident (CVA), and peripheral arterial disease (PAD) as our outcomes of interest. We implemented logistic regression analysis in the univariable and multivariable models. In the multivariable model, we adjusted all outcomes for potential confounders, including age, sex, ethnicity, obesity, anemia, diabetes, hypertension, renal failure, history of smoking or alcohol abuse, prior history of MI, primary coronary intervention (PCI), or coronary artery bypass grafting (CABG), coagulopathy, liver disease, chronic pulmonary disease, ischemic cardiomyopathy, Elixhauser comorbidity index, hypothyroidism, cancer, history of defibrillator or pacemaker, and long-term use of steroids, anticoagulants, antiplatelet or antithrombotic agents. The analysis was done using the STATA software, version 17.0 (SE).<
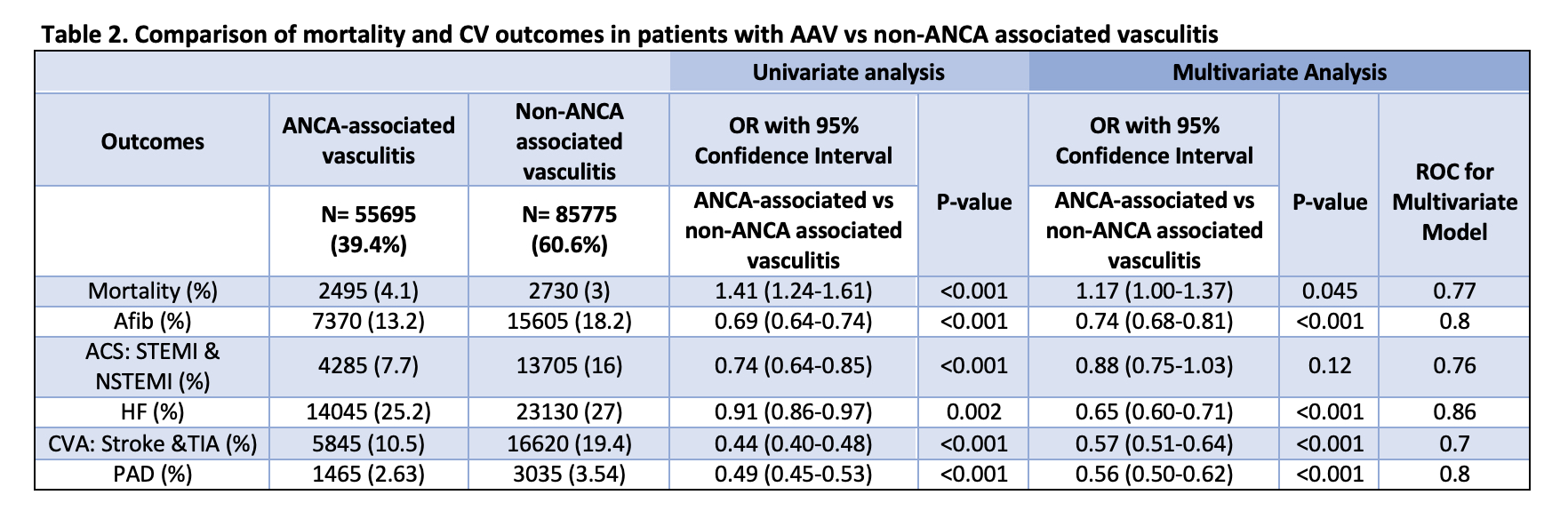
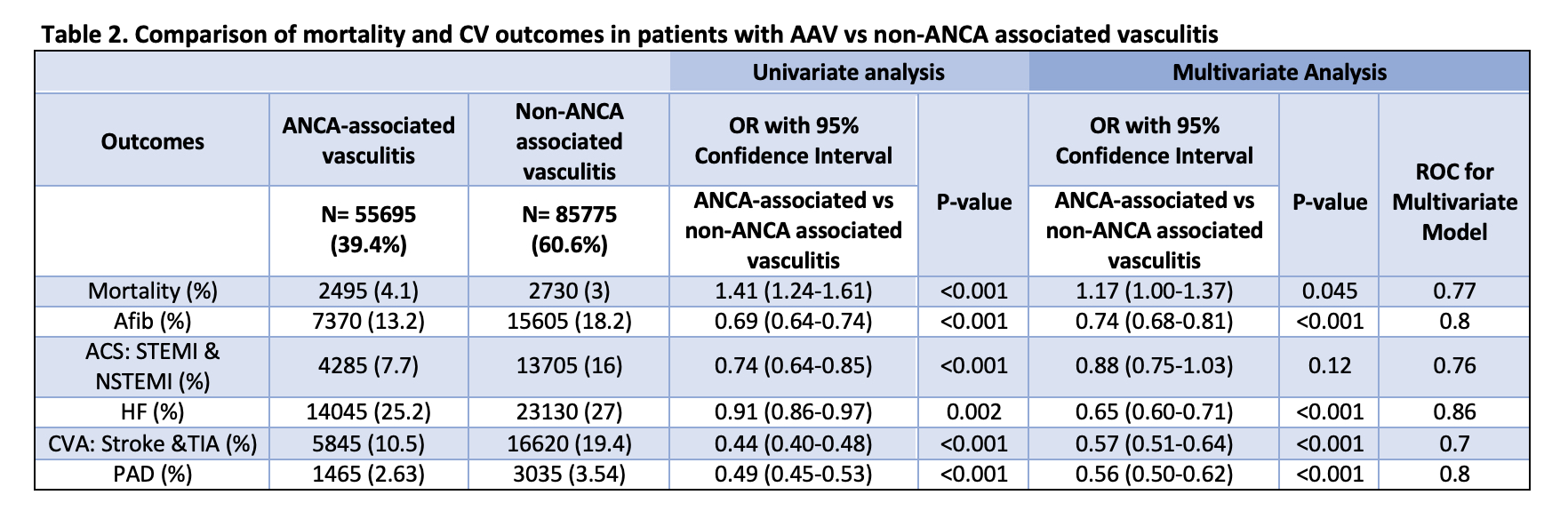
Results: We identified 141,470 patients with vasculitis, of whom 55,695 (39%) had AAV and 85,775 (61%) had non-ANCA associated vasculitis. Our results showed that patients with AAV had a higher mortality (OR: 1.17; 95%-CI 1.00-1.37; p-value = 0.045) when compared to patients with non-ANCA associated vasculitis even after adjusting for potential confounders. There was no difference in risk of ACS between the two groups (OR: 0.88; 95%-CI 0.75-1.03; p-value = 0.12). AAV was associated with a lower risk of Afib (OR: 0.74; 95%-CI 0.68-0.81; p-value < 0.001), HF (OR: 0.65; 95%-CI 0.60-0.71; p-value < 0.001), CVA (OR: 0.57; 95%-CI 0.51-0.64; p-value < 0.001) and PAD (OR: 0.56; 95%-CI 0.50-0.62; p-value < 0.001) when compared with patients with non-ANCA vasculitis.
Conclusion: Patients with AAV had a higher risk of in-hospital mortality. However, patients with non-ANCA vasculitis had a higher prevalence of Afib, ACS, HF, CVA, and PAD which may be related to their older age and larger vessel involvement. These results suggest that ANCA antibodies alone are not responsible for increased CV disease in this population.
Disclosures: A. Arevalo, None; P. Shah, None; H. Zala, None; F. Haddadin, None; M. Majmundar, None; A. Ramirez Gomez, None.
Background/Purpose: Several studies have reported that patients with ANCA-associated vasculitis (AAV) are at increased risk of cardiovascular complications from accelerated atherosclerosis with an excess cardiovascular (CV) risk of 65%. HTN and diabetes mellitus (DM) are two of the most reported treatment-related complications observed at long-term follow-up. However, the risk of CV disease is greater in AAV and cannot be explained through traditional CV risk factors alone. ANCA are harmful antibodies that are directly involved in blood vessel damage through neutrophil and complement cascade activation, but it is unclear if they are directly responsible for the higher rate of CV complications in AAV. Therefore, we aimed to compare ANCA-associated and non-ANCA-associated vasculitis and their associations with mortality and CV outcomes.
Methods: In this retrospective cohort study, we identified patients with ANCA-associated and non-ANCA-associated vasculitis based on ICD-10 codes, using the Nationwide Inpatient Sample database (NIS) from 2016 to 2019. We included all-cause mortality, atrial fibrillation (Afib), ST-elevation (STEMI) and non-ST elevation myocardial infarction (NSTEMI), heart failure (HF), cerebrovascular accident (CVA), and peripheral arterial disease (PAD) as our outcomes of interest. We implemented logistic regression analysis in the univariable and multivariable models. In the multivariable model, we adjusted all outcomes for potential confounders, including age, sex, ethnicity, obesity, anemia, diabetes, hypertension, renal failure, history of smoking or alcohol abuse, prior history of MI, primary coronary intervention (PCI), or coronary artery bypass grafting (CABG), coagulopathy, liver disease, chronic pulmonary disease, ischemic cardiomyopathy, Elixhauser comorbidity index, hypothyroidism, cancer, history of defibrillator or pacemaker, and long-term use of steroids, anticoagulants, antiplatelet or antithrombotic agents. The analysis was done using the STATA software, version 17.0 (SE).<
Results: We identified 141,470 patients with vasculitis, of whom 55,695 (39%) had AAV and 85,775 (61%) had non-ANCA associated vasculitis. Our results showed that patients with AAV had a higher mortality (OR: 1.17; 95%-CI 1.00-1.37; p-value = 0.045) when compared to patients with non-ANCA associated vasculitis even after adjusting for potential confounders. There was no difference in risk of ACS between the two groups (OR: 0.88; 95%-CI 0.75-1.03; p-value = 0.12). AAV was associated with a lower risk of Afib (OR: 0.74; 95%-CI 0.68-0.81; p-value < 0.001), HF (OR: 0.65; 95%-CI 0.60-0.71; p-value < 0.001), CVA (OR: 0.57; 95%-CI 0.51-0.64; p-value < 0.001) and PAD (OR: 0.56; 95%-CI 0.50-0.62; p-value < 0.001) when compared with patients with non-ANCA vasculitis.
Conclusion: Patients with AAV had a higher risk of in-hospital mortality. However, patients with non-ANCA vasculitis had a higher prevalence of Afib, ACS, HF, CVA, and PAD which may be related to their older age and larger vessel involvement. These results suggest that ANCA antibodies alone are not responsible for increased CV disease in this population.
Disclosures: A. Arevalo, None; P. Shah, None; H. Zala, None; F. Haddadin, None; M. Majmundar, None; A. Ramirez Gomez, None.

