Back
Poster Session C
Pediatric autoimmune diseases: Kawasaki disease, juvenile dermatomyositis and juvenile localized scleroderma
Session: (1360–1386) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
1372: Telemedicine Use in the Assessment of Juvenile Dermatomyositis and Polymyositis: A Survey of Caregivers and Patients
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- YG
Y. Ingrid Goh, PhD
The Hospital for Sick Children
Toronto, ON, Canada
Abstract Poster Presenter(s)
Stacey Tarvin1, Y. Ingrid Goh2, Nicole Taylor3, Bianca Lang4, Marietta De Guzman5, Julie Fuller6, Kristin Houghton7, Susan Kim8, Vanessa Carbone9, Kathryn Cook10, Tanya Slater9, Angela Robinson11, Liza McCann12, Charalampia Papadopoulou13, Clarissa Pilkington14, Phoebe Rushe15 and Peter Blier16, 1Riley Hospital for Children at Indiana University Health, Indianapolis, IN, 2Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute, Toronto, ON, Canada, 3University of Indianapolis, Indianapolis, IN, 4Dalhousie University - Halifax, Halifax, NS, Canada, 5Baylor College of Medicine/ Texas Children's Hospital, Houston, TX, 6UT Southwestern, Frisco, TX, 7University of British Columbia - Vancouver, Vancouver, BC, Canada, 8UCSF Benioff Children's Hospital, San Francisco, CA, 9The Hospital for Sick Children, Toronto, ON, Canada, 10Akron Children's Hospital, Copley, OH, 11Cleveland Clinic, Cleveland, OH, 12Alder Hey Children's NHS Foundation Trust, Liverpool, United Kingdom, 13UCL Institute of Child Health, and Great Ormond Street Hospital NHS Foundation Trust, Section Head Infection, Immunology, and Rheumatology, London, United Kingdom, 14Great Ormond Street Hospital, London, United Kingdom, 15Royal Liverpool University Hospital, Liverpool, United Kingdom, 16Retired, Amherst, MA
Background/Purpose: Care of patients with juvenile myositis (JM) involves complex assessments performed by highly trained specialists. Restrictions surrounding the COVID-19 pandemic resulted in many patients using telemedicine to obtain care. We examined the experience and opinions of JM patients and their caregivers with telemedicine care.
Methods: A REDCap survey link was distributed to Cure JM Foundation members and advertised worldwide by Childhood Arthritis Rheumatology Research Alliance and Paediatric Rheumatology European Society via email, social media, and word of mouth, from February-May 2022. Quantitative data were analyzed using descriptive statistics and qualitative data were thematically analyzed.
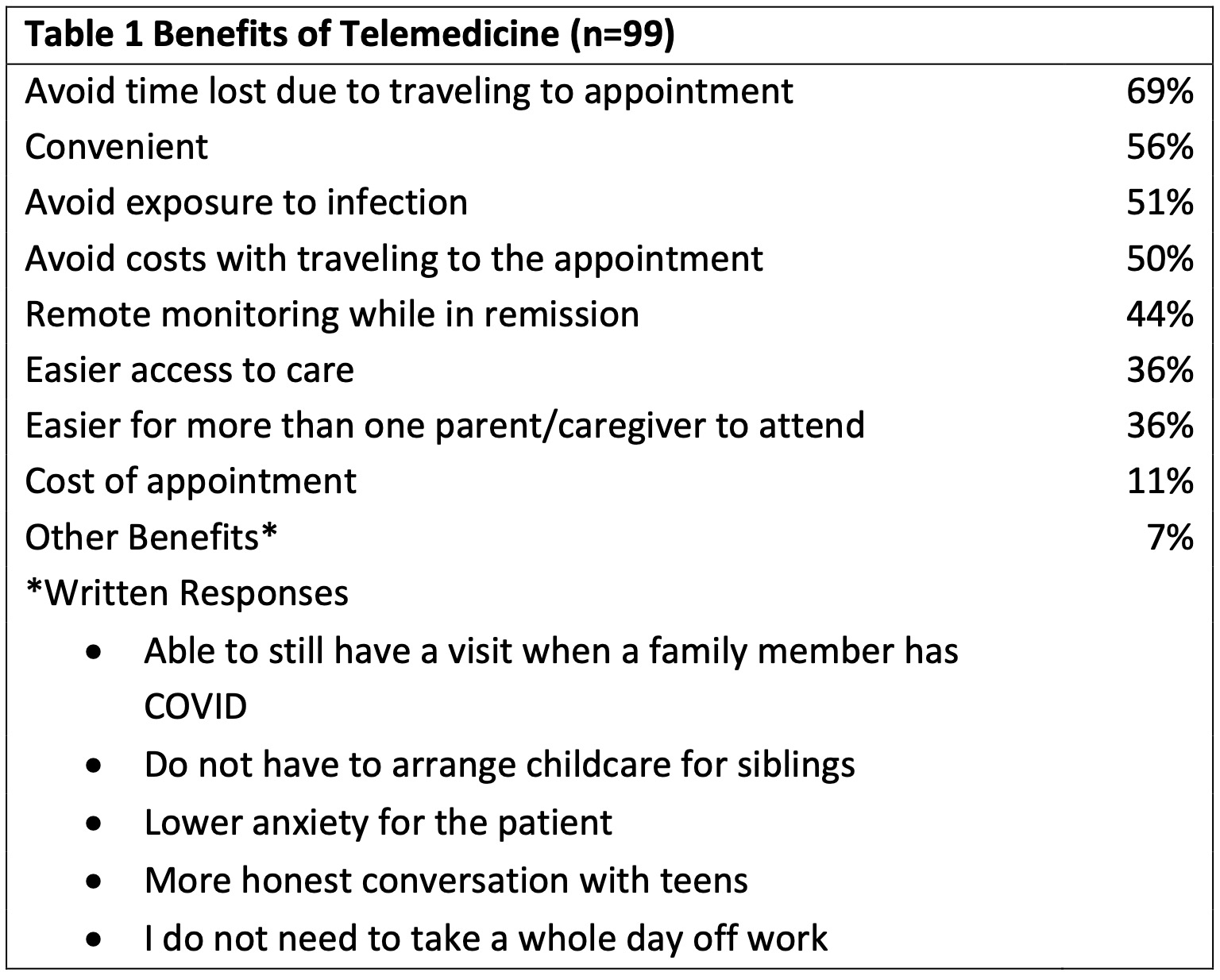
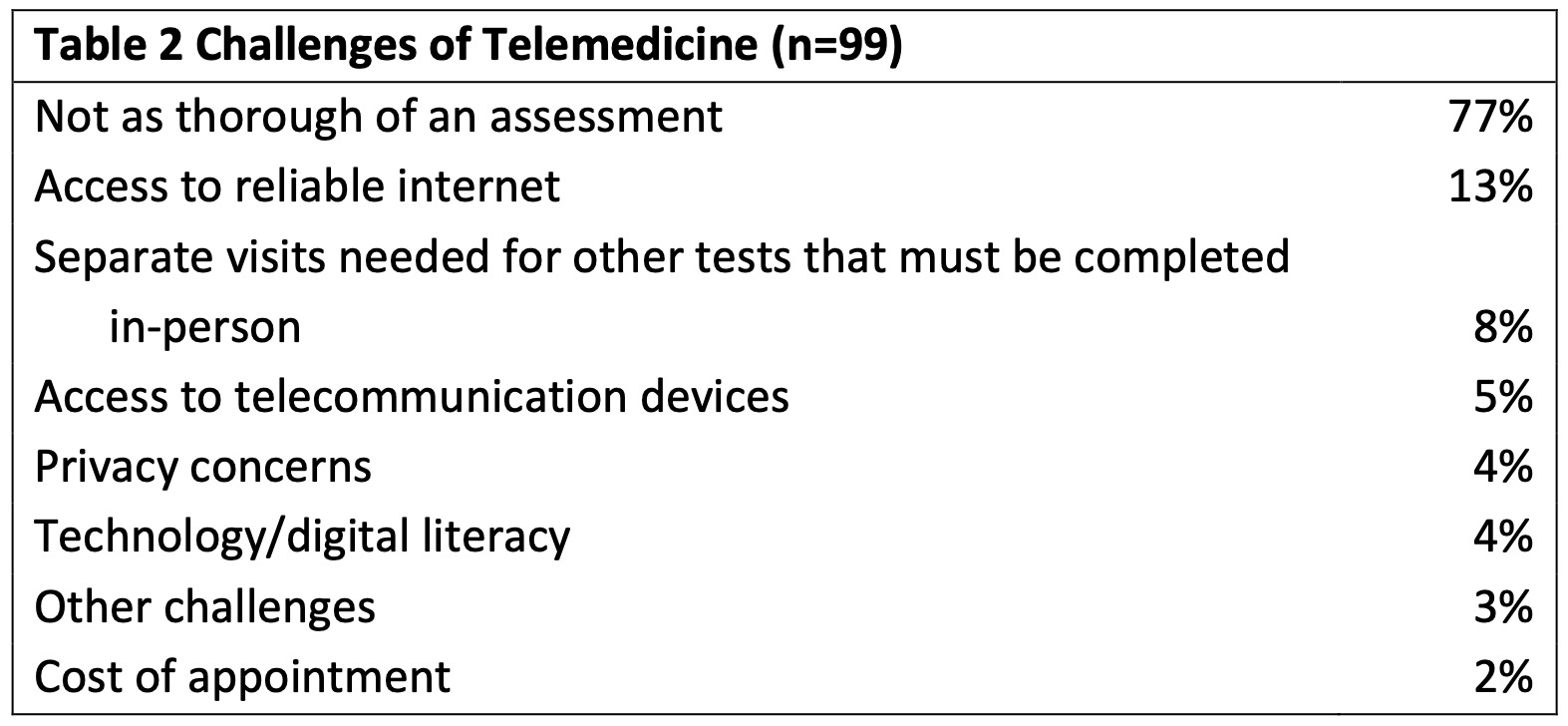
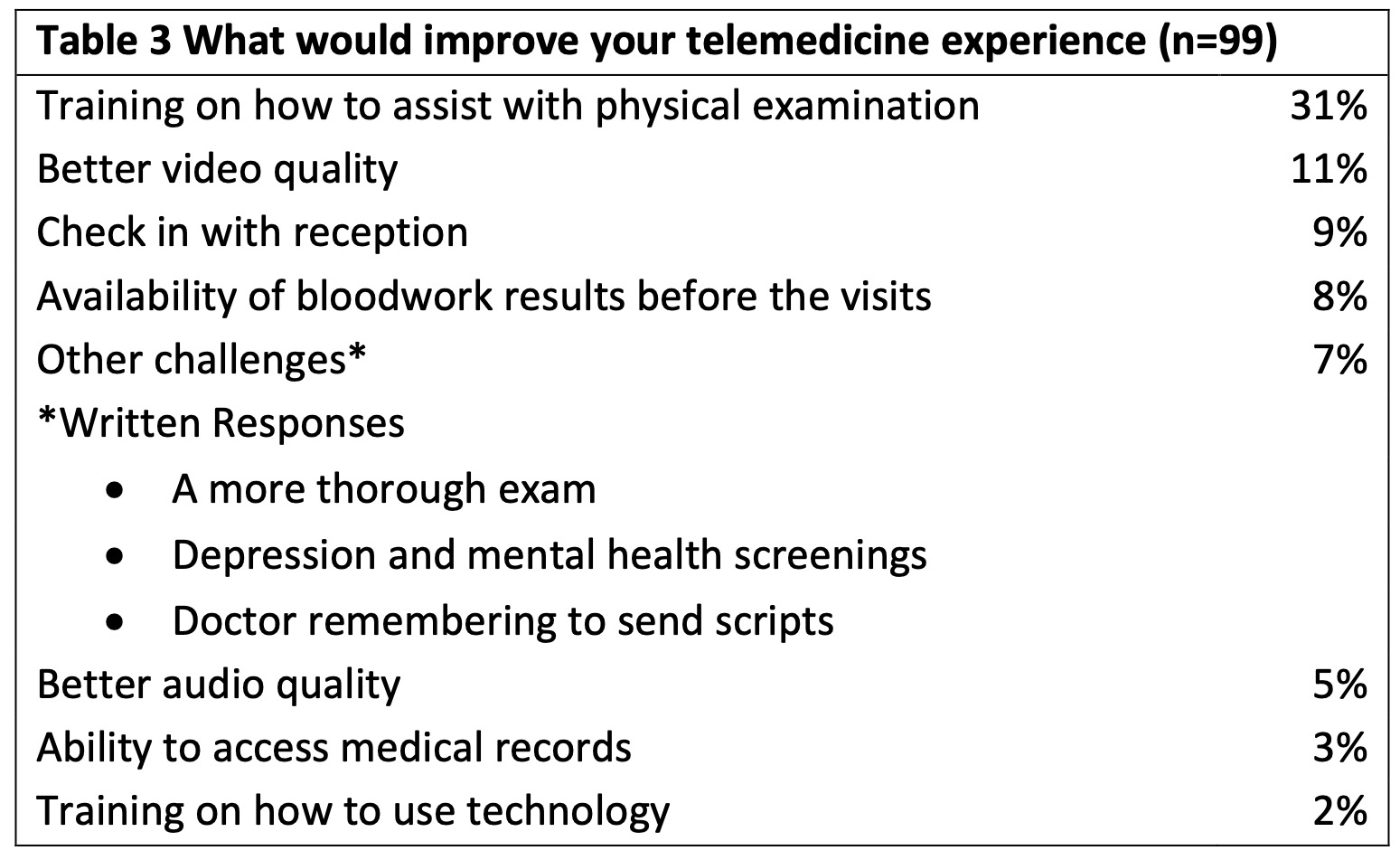
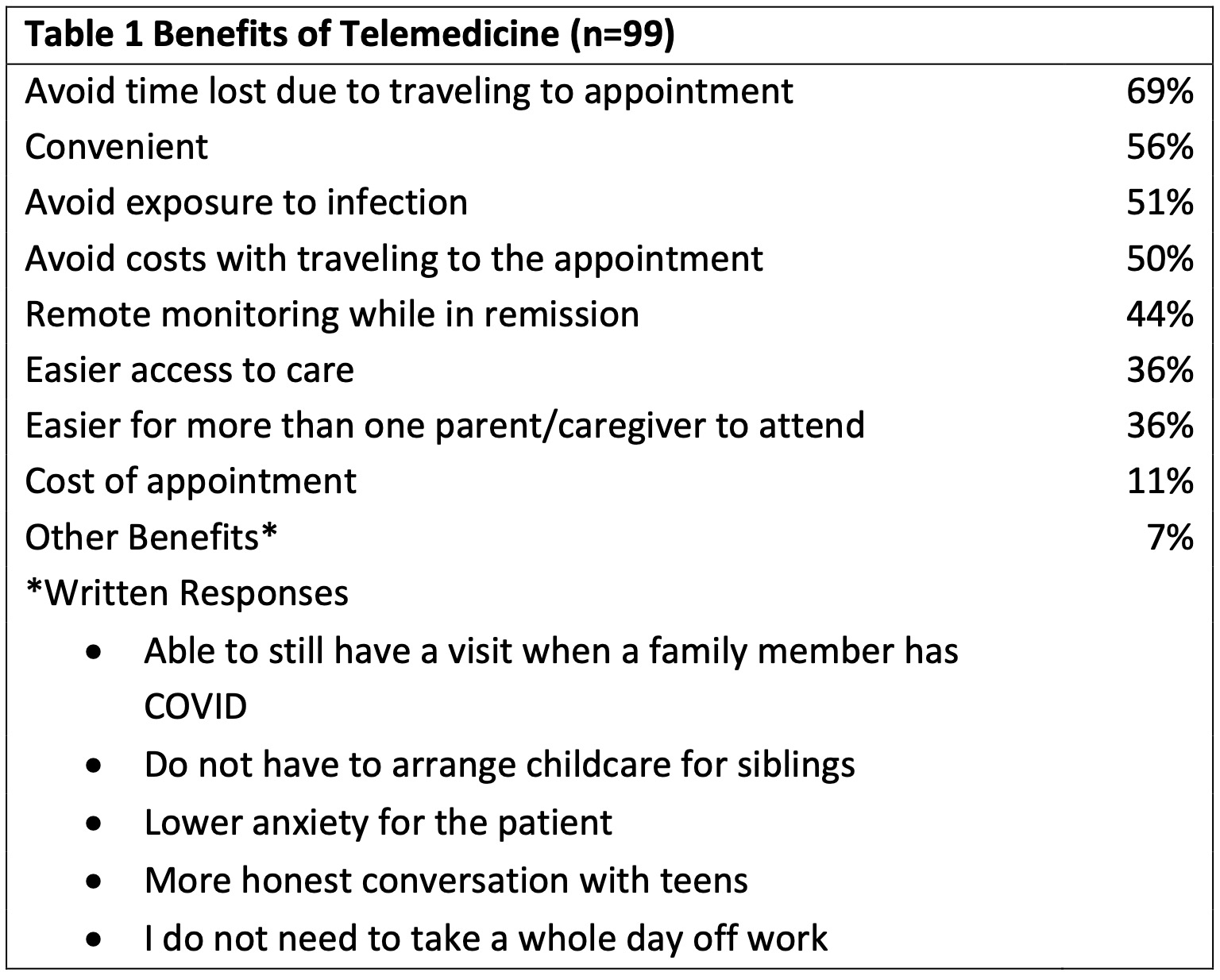
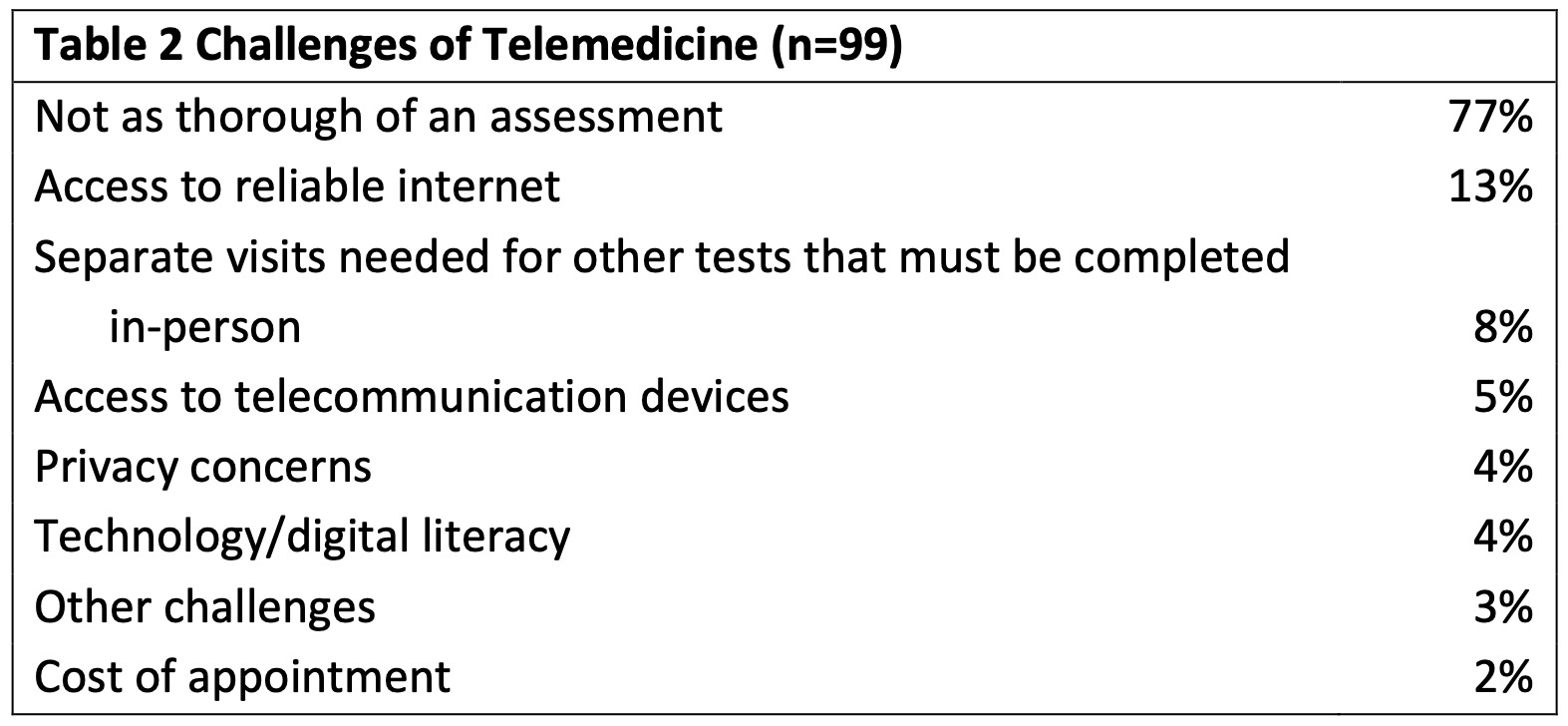
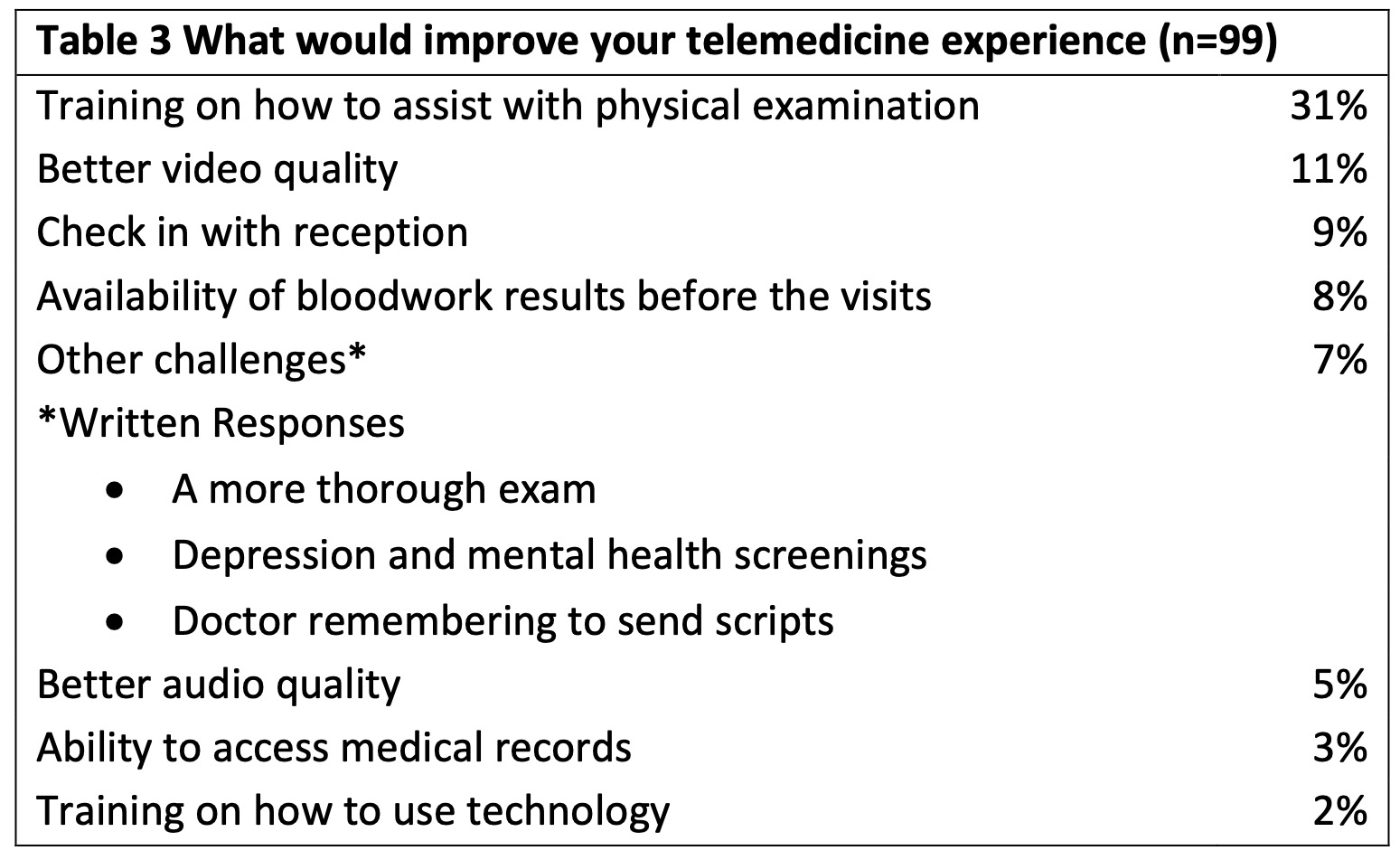
Results: 99 patients and caregivers aged > 18 years participated. The majority of respondents were from the United States. 65% learned of the survey from CureJM, 10% from a rheumatology provider and 11% through social media or "other." 65% had participated in a telemedicine visit. 40% of those respondents had 2-4 visits. Of those visits, 61% were conducted over a video conferencing system. Access to technology was an issue for a minority of responding families, with 79% of respondents having devices available to access telemedicine visits and 81% with reliable home internet. Only 5% of respondents indicated access to telecommunication devices was a challenge and 13% indicated trouble with reliable internet. In terms of at home assessment, 56% indicated comfort assessing skin, muscle or joints at home. 31% said no additional training was necessary for them to assess their child at home but when offered, an average of 42% of respondents indicated a desire for more training in skin, muscle strength, and/or joint assessment. Benefits, challenges, and desired improvements of telemedicine were assessed (Tables 1, 2, 3). 58% of respondents were familiar with the Childhood Myositis Assessment Scale (CMAS) and 36% indicated the CMAS was "always" performed at in person visits vs. 9% in telemedicine visits. 28% of respondents indicated that the CMAS "always or often" accurately reflects JM disease activity. 37% of respondents indicated a "remote" CMAS would be a good tool to have for telemedicine visits and 75% were willing to learn the CMAS and perform it as part of a telemedicine visit. 43% of respondents indicated they were satisfied with the care received over telemedicine visits. 23% were not comfortable receiving care via telemedicine. 26% of respondents indicated wanting only in-person visits while 62% said a combination of telemedicine or in-person visits was acceptable.
Conclusion: JM patients and/or caregivers utilized telemedicine care during the pandemic and some were satisfied with this platform. The majority of respondents expressed concern regarding the thoroughness of the care received using telemedicine and many respondents indicated that further training of patients/caregivers to aid in clinical assessment would be helpful. These findings suggest that while there is a role for telemedicine in the future care of JM patients, it would benefit from developing or improving remote assessment tools for JM.
Disclosures: S. Tarvin, None; Y. Goh, None; N. Taylor, None; B. Lang, Moderna; M. De Guzman, None; J. Fuller, None; K. Houghton, None; S. Kim, None; V. Carbone, None; K. Cook, None; T. Slater, None; A. Robinson, None; L. McCann, None; C. Papadopoulou, None; C. Pilkington, None; P. Rushe, None; P. Blier, None.
Background/Purpose: Care of patients with juvenile myositis (JM) involves complex assessments performed by highly trained specialists. Restrictions surrounding the COVID-19 pandemic resulted in many patients using telemedicine to obtain care. We examined the experience and opinions of JM patients and their caregivers with telemedicine care.
Methods: A REDCap survey link was distributed to Cure JM Foundation members and advertised worldwide by Childhood Arthritis Rheumatology Research Alliance and Paediatric Rheumatology European Society via email, social media, and word of mouth, from February-May 2022. Quantitative data were analyzed using descriptive statistics and qualitative data were thematically analyzed.
Results: 99 patients and caregivers aged > 18 years participated. The majority of respondents were from the United States. 65% learned of the survey from CureJM, 10% from a rheumatology provider and 11% through social media or "other." 65% had participated in a telemedicine visit. 40% of those respondents had 2-4 visits. Of those visits, 61% were conducted over a video conferencing system. Access to technology was an issue for a minority of responding families, with 79% of respondents having devices available to access telemedicine visits and 81% with reliable home internet. Only 5% of respondents indicated access to telecommunication devices was a challenge and 13% indicated trouble with reliable internet. In terms of at home assessment, 56% indicated comfort assessing skin, muscle or joints at home. 31% said no additional training was necessary for them to assess their child at home but when offered, an average of 42% of respondents indicated a desire for more training in skin, muscle strength, and/or joint assessment. Benefits, challenges, and desired improvements of telemedicine were assessed (Tables 1, 2, 3). 58% of respondents were familiar with the Childhood Myositis Assessment Scale (CMAS) and 36% indicated the CMAS was "always" performed at in person visits vs. 9% in telemedicine visits. 28% of respondents indicated that the CMAS "always or often" accurately reflects JM disease activity. 37% of respondents indicated a "remote" CMAS would be a good tool to have for telemedicine visits and 75% were willing to learn the CMAS and perform it as part of a telemedicine visit. 43% of respondents indicated they were satisfied with the care received over telemedicine visits. 23% were not comfortable receiving care via telemedicine. 26% of respondents indicated wanting only in-person visits while 62% said a combination of telemedicine or in-person visits was acceptable.
Conclusion: JM patients and/or caregivers utilized telemedicine care during the pandemic and some were satisfied with this platform. The majority of respondents expressed concern regarding the thoroughness of the care received using telemedicine and many respondents indicated that further training of patients/caregivers to aid in clinical assessment would be helpful. These findings suggest that while there is a role for telemedicine in the future care of JM patients, it would benefit from developing or improving remote assessment tools for JM.
Disclosures: S. Tarvin, None; Y. Goh, None; N. Taylor, None; B. Lang, Moderna; M. De Guzman, None; J. Fuller, None; K. Houghton, None; S. Kim, None; V. Carbone, None; K. Cook, None; T. Slater, None; A. Robinson, None; L. McCann, None; C. Papadopoulou, None; C. Pilkington, None; P. Rushe, None; P. Blier, None.

