Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1260: Tenderness and Radiographic Progression in Rheumatoid Arthritis and Psoriatic Arthritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- IG
Irina Gessl, MD
Medical University of Vienna
Vienna, Austria
Abstract Poster Presenter(s)
Irina Gessl1, Mihaela Popescu2, Gabriela supp3, Thomas Deimel1, Paul Studenic1, Martina Durechova3, michael zauner3, Josef Smolen1 and Peter Mandl1, 1Medical University of Vienna, Vienna, Austria, 2Department of Rheumatology, Hôpital Maisonneuve-Rosemont, Montréal, QC, Canada, 3Division of Rheumatology, Department of Internal Medicine III, Medical University of Vienna, Vienna, Austria
Background/Purpose: In inflammatory arthritis swelling is regarded as a sign of synovitis and is associated with radiographic progression. However, the association of tenderness with radiographic progression is not clear. The aim of this study was to assess the predictive value of tenderness alone and with consideration of sonographic signs for synovitis, disease duration and baseline radiographic damage for subsequent radiographic progression in rheumatoid arthritis (RA) and psoriatic arthritis (PsA).
Methods: Clinical and sonographic (grey scale (GS) and power Doppler (PD)) examination of 22 joints of the hand were performed cross-sectionally in consecutive patients with RA and PsA with at least one tender joint. Radiographs were scored for erosions and joint space narrowing (JSN) at inclusion and radiographic progression of each joint was assessed after 2 years. The impact of tenderness on progression was analyzed in non-swollen joints for RA and PsA separately with logistic regression analyses. As a second step, the association of PD, GS, disease duration, C-reactive protein, baseline erosions and JSN and global joint counts with subsequent structural damage was assessed using univariate logistic regression in tender non-swollen joints again on the joint level.
Results: We included 1207 joints in 54 RA patients and 396 joints in 18 PsA patients. Tenderness was associated with subsequent radiographic progression in non-swollen joints in PsA (OR 3.44, 95%CI 1.78-6.62, p< 0.01) but not in RA (OR 1.60, 95% CI 0.99-2.48, p=0.55) (Figure 1). In tender non-swollen joints in RA patients, PD (OR 3.74, 95% CI 1.10-13.30, p=0.04) and baseline erosions (OR 4.42, 95% CI 1.22-15.95, p=0.02) had a significant impact on radiographic progression. In PsA patients, PD (OR 8.46, 95% CI 1.72-41.72, p< 0.01), baseline erosions (OR 6.71, 95% CI 1.43-31.39, p=0.02), baseline JSN (OR 7.27, 95% CI 1.47-35.89, p=0.02) and SJC (OR 1.26, 95%CI 1.07-1.48, p< 0.01) were associated with radiographic progression.
Conclusion: Our findings indicate that tenderness in non-swollen joints is associated with subsequent radiographic progression in PsA, while in RA it is a risk factor for radiographic progression only in the presence of additional factors, such as sonographic signs for synovitis.
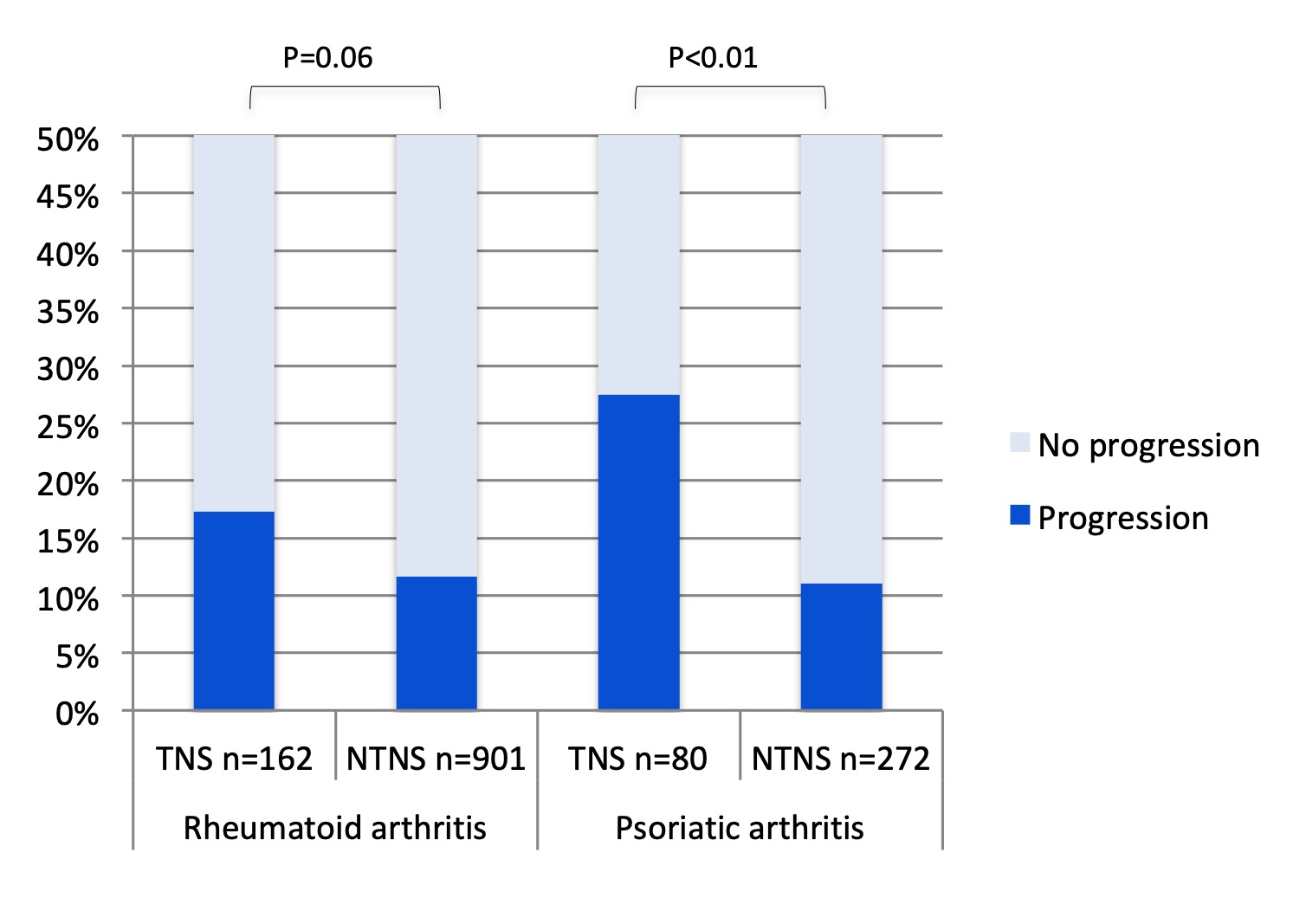 Figure 1. The proportion of joints with progression in tender non-swollen and non-tender non-swollen joints in patients with rheumatoid and psoriatic arthritis; NTNS: non-tender non-swollen; TNS: tender non-swollen
Figure 1. The proportion of joints with progression in tender non-swollen and non-tender non-swollen joints in patients with rheumatoid and psoriatic arthritis; NTNS: non-tender non-swollen; TNS: tender non-swollen
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291695-2-ANY.jpg width=440 height=557.498591549296 border=0 style=border-style: none;>
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291695-3-ANY(1).jpg width=440 height=557.498591549296 border=0 style=border-style: none;>
Disclosures: I. Gessl, Eli Lilly, Boehringer-Ingelheim, Gilead; M. Popescu, None; G. supp, None; T. Deimel, None; P. Studenic, AbbVie/Abbott; M. Durechova, None; m. zauner, None; J. Smolen, AbbVie, AstraZeneca, Eli Lilly, Novartis, Amgen, Bristol Myers Squibb, Galapagos-Gilead, Janssen, Merck-Sharp-Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, UCB; P. Mandl, None.
Background/Purpose: In inflammatory arthritis swelling is regarded as a sign of synovitis and is associated with radiographic progression. However, the association of tenderness with radiographic progression is not clear. The aim of this study was to assess the predictive value of tenderness alone and with consideration of sonographic signs for synovitis, disease duration and baseline radiographic damage for subsequent radiographic progression in rheumatoid arthritis (RA) and psoriatic arthritis (PsA).
Methods: Clinical and sonographic (grey scale (GS) and power Doppler (PD)) examination of 22 joints of the hand were performed cross-sectionally in consecutive patients with RA and PsA with at least one tender joint. Radiographs were scored for erosions and joint space narrowing (JSN) at inclusion and radiographic progression of each joint was assessed after 2 years. The impact of tenderness on progression was analyzed in non-swollen joints for RA and PsA separately with logistic regression analyses. As a second step, the association of PD, GS, disease duration, C-reactive protein, baseline erosions and JSN and global joint counts with subsequent structural damage was assessed using univariate logistic regression in tender non-swollen joints again on the joint level.
Results: We included 1207 joints in 54 RA patients and 396 joints in 18 PsA patients. Tenderness was associated with subsequent radiographic progression in non-swollen joints in PsA (OR 3.44, 95%CI 1.78-6.62, p< 0.01) but not in RA (OR 1.60, 95% CI 0.99-2.48, p=0.55) (Figure 1). In tender non-swollen joints in RA patients, PD (OR 3.74, 95% CI 1.10-13.30, p=0.04) and baseline erosions (OR 4.42, 95% CI 1.22-15.95, p=0.02) had a significant impact on radiographic progression. In PsA patients, PD (OR 8.46, 95% CI 1.72-41.72, p< 0.01), baseline erosions (OR 6.71, 95% CI 1.43-31.39, p=0.02), baseline JSN (OR 7.27, 95% CI 1.47-35.89, p=0.02) and SJC (OR 1.26, 95%CI 1.07-1.48, p< 0.01) were associated with radiographic progression.
Conclusion: Our findings indicate that tenderness in non-swollen joints is associated with subsequent radiographic progression in PsA, while in RA it is a risk factor for radiographic progression only in the presence of additional factors, such as sonographic signs for synovitis.
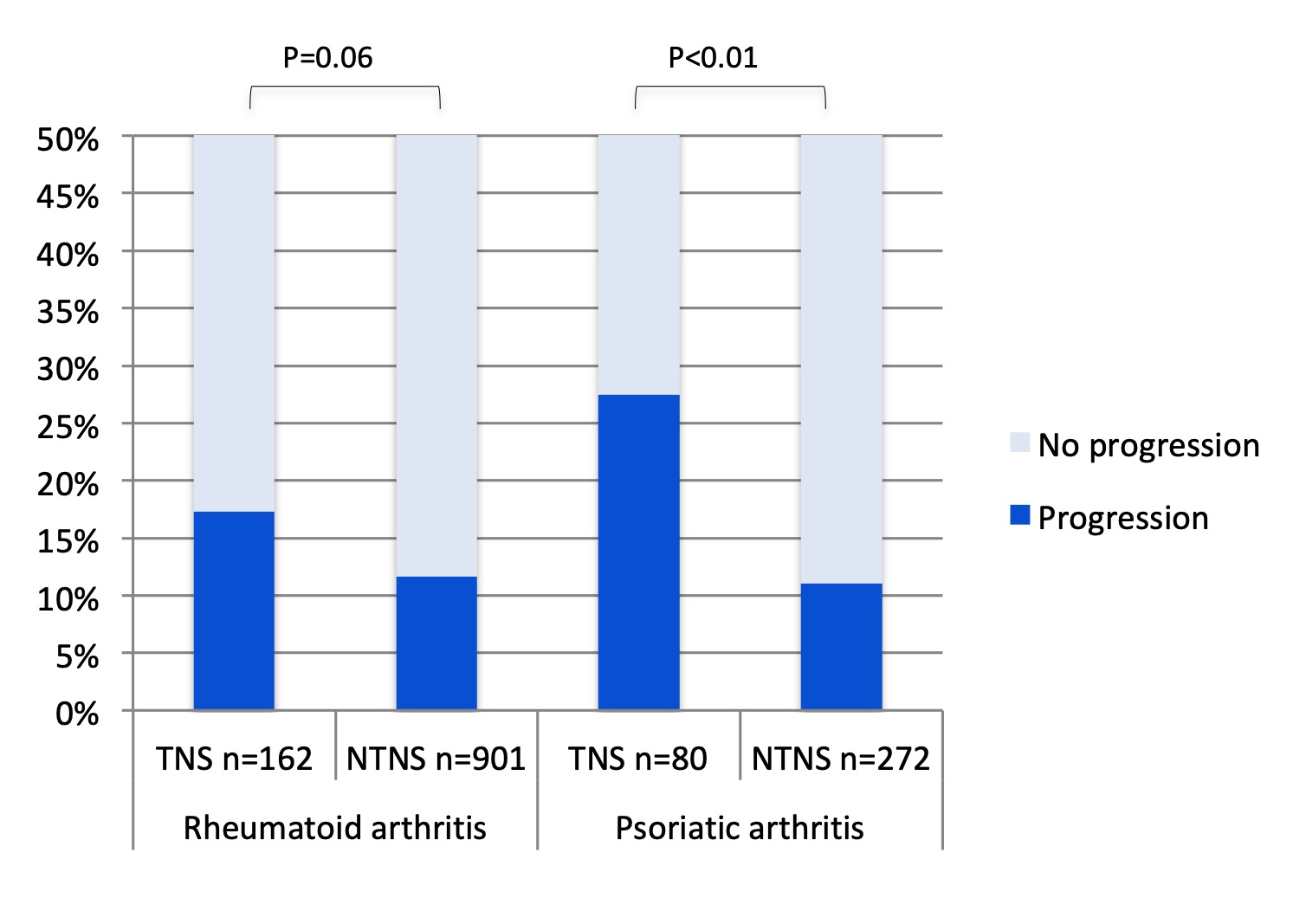 Figure 1. The proportion of joints with progression in tender non-swollen and non-tender non-swollen joints in patients with rheumatoid and psoriatic arthritis; NTNS: non-tender non-swollen; TNS: tender non-swollen
Figure 1. The proportion of joints with progression in tender non-swollen and non-tender non-swollen joints in patients with rheumatoid and psoriatic arthritis; NTNS: non-tender non-swollen; TNS: tender non-swollen<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291695-2-ANY.jpg width=440 height=557.498591549296 border=0 style=border-style: none;>
Figure 2. The proportion of tender non-swollen joints with radiographic progression in patients with rheumatoid arthritis depending on power Doppler signs for synovitis (A), disease duration (B), erosions (C) and JSN (D) at baseline x-ray and difference of baseline SJC (E) and TJC (F) of joints with and without subsequent progression. BL, baseline; early, early rheumatoid arthritis ( < 3 years disease duration), JSN, joint space narrowing; long-standing, long-standing rheumatoid arthritis (>5 years disease duration); PD, power Doppler; SJC, swollen joint count; TJC, tender joint count.
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291695-3-ANY(1).jpg width=440 height=557.498591549296 border=0 style=border-style: none;>
Figure 3. The proportion of tender non-swollen joints with progression in patients with psoriatic arthritis depending on power Doppler signs for synovitis (A), disease duration (B), erosions (C) and JSN (D) at baseline x-ray and difference of baseline 66 SJC (E) and 68 TJC (F) of joints with and without subsequent progression. BL, baseline; early, early psoriatic arthritis ( < 3 years disease duration), JSN, joint space narrowing; long-standing, long-standing psoriatic arthritis (>5 years disease duration); PD, power Doppler; SJC, swollen joint count; TJC, tender joint count.
Disclosures: I. Gessl, Eli Lilly, Boehringer-Ingelheim, Gilead; M. Popescu, None; G. supp, None; T. Deimel, None; P. Studenic, AbbVie/Abbott; M. Durechova, None; m. zauner, None; J. Smolen, AbbVie, AstraZeneca, Eli Lilly, Novartis, Amgen, Bristol Myers Squibb, Galapagos-Gilead, Janssen, Merck-Sharp-Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, UCB; P. Mandl, None.

