Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1203: The Association Between Anti-Citrullinated Peptide Antibodies and Subclinical Interstitial Lung Disease in Community-Dwelling Adults: The Multi-Ethnic Study of Atherosclerosis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JL
Jenna Lanz, MD
Columbia University Medical Center
New York, NY, United States
Abstract Poster Presenter(s)
Jenna Lanz1, Jan Hughes-Austin2, Anna Podolanczuk3, John Kim4, John Austin5, William Robinson6, Ganesh Raghu7, Eric Hoffman8, John Newell Jr8, Jubal Watts Jr9, P. Hrudaya Nath9, Sushilkumar Sonavane10, R. Graham Barr5 and Elana Bernstein1, 1Columbia University, New York, NY, 2University of California, San Diego, San Diego, CA, 3Weill Cornell Medical College, New York, NY, 4University of Virginia School of Medicine, Charlottesville, VA, 5Columbia University Medical Center, New York, NY, 6Stanford University School of Medicine, Palo Alto, CA, 7University of Washington, Seattle, WA, 8University of Iowa, Iowa City, IA, 9University of Alabama at Birmingham, Birmingham, AL, 10Mayo Clinic, Rochester, MN
Background/Purpose: We previously demonstrated a significant association between serum anti-CCP levels and prevalence of interstitial lung abnormalities (ILA) in community-dwelling adults. A greater number of positive anti-citrullinated protein antibodies (ACPAs) has been associated with a greater interstitial lung disease (ILD) extent in adults with RA. The aim of this study was to determine whether greater numbers of positive ACPAs are associated with ILA in community-dwelling adults.
Methods: The Multi-Ethnic Study of Atherosclerosis (MESA) is a multi-center, prospective cohort study of 6814 adults aged 45-84 when recruited in 2000-2002 (Exam 1) from 6 US sites. 29 ACPAs (Table 1) were measured via Bio-Plex bead array in 1949 participants at Exams 2 or 3 (2003-2005) as part of the MESA Abdominal Aortic Calcium ancillary study. 2430 full lung CTs from Exam 5 (2010-2012) had ILA assessments performed by 1 of 5 trained thoracic radiologists. ILA was defined as the presence of ground glass abnormalities, reticular abnormalities, nonemphysematous cysts, honeycombing, and traction bronchiectasis affecting >5% of any lung zone in a non-dependent fashion. A positive ACPA was defined as a titer > 75th percentile. The number of positive ACPA was modeled as the independent continuous variable of interest in a logistic regression model with ILA as the dependent variable, adjusting for age, sex, race/ethnicity, education, cigarette pack-years, and smoking status.
Results: 868 participants had ACPAs measured at Exams 2 or 3 and underwent full lung CT at Exam 5. Median age was 58 (IQR 52-66) years. 50% were female, 42% White, 21% African American, 13% Chinese American, and 24% Hispanic (Table 2). Median number of positive ACPA was 2 (IQR 1-13). 100 participants (11.5%) had ILA on CT. We detected an inverse relationship between number of positive ACPA and odds of ILA in univariate and multivariable models. In the unadjusted model, each 1 unit increase in number of positive ACPA was associated with a 37% decrease in odds of ILA (OR 0.63, 95% CI 0.39 – 1.03, p= 0.06). In a fully adjusted model, each 1 unit increase in number of positive ACPA was associated with an 18% decrease in odds of ILA (OR 0.82, 95% CI 0.67 – 0.98, p= 0.047). In a fully adjusted model, the p-value for interaction between number of positive ACPA and race/ethnicity was 0.04. In fully adjusted models, each 1 unit increase in number of positive ACPA was associated with a 40% decrease in odds of ILA among African American participants (OR 0.60, 95% CI 0.37 – 0.95, p=0.03) and a 42% decrease in odds of ILA among Hispanic participants (OR 0.58, 95% CI 0.37 – 0.90, p=0.02; Table 3). There was no significant association between number of positive ACPA and ILA among White or Chinese American participants.
Conclusion: In this large population-based multi-ethnic study, an expanded ACPA repertoire was associated with a lower burden of ILA on CT, especially among African American and Hispanic participants. This finding was unexpected given the known positive relationship between ILD and an expanded ACPA repertoire in adults with RA. Further studies are necessary to explore whether ACPAs may reduce the risk of ILD in African American and Hispanic adults.
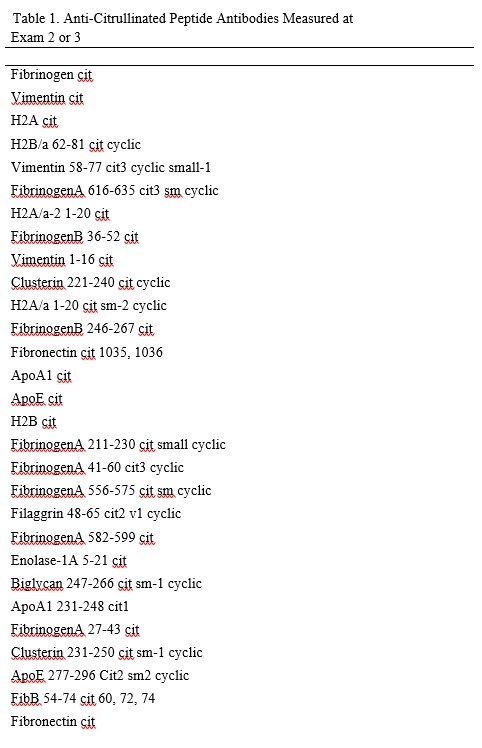 Table 1. Anti-Citrullinated Peptide Antibodies Measured at Exam 2 or 3
Table 1. Anti-Citrullinated Peptide Antibodies Measured at Exam 2 or 3
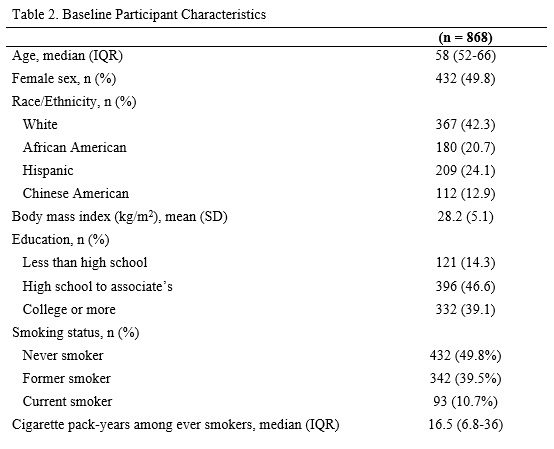 Table 2. Baseline Participant Characteristics
Table 2. Baseline Participant Characteristics
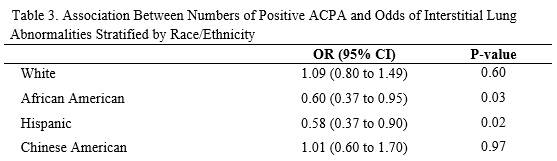 Table 3. Association Between Numbers of Positive ACPA and Odds of Interstitial Lung Abnormalities Stratified by Race/Ethnicity
Table 3. Association Between Numbers of Positive ACPA and Odds of Interstitial Lung Abnormalities Stratified by Race/Ethnicity
Disclosures: J. Lanz, None; J. Hughes-Austin, None; A. Podolanczuk, Boehringer-Ingelheim, Roche, Imvaria, Regeneron; J. Kim, None; J. Austin, None; W. Robinson, None; G. Raghu, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Roche, Genentech; E. Hoffman, None; J. Newell Jr, VIDA, Elsevier Publishing; J. Watts Jr, Boehringer-Ingelheim, Genentech; P. Nath, None; S. Sonavane, None; R. Barr, None; E. Bernstein, Boehringer-Ingelheim, Kadmon, Pfizer.
Background/Purpose: We previously demonstrated a significant association between serum anti-CCP levels and prevalence of interstitial lung abnormalities (ILA) in community-dwelling adults. A greater number of positive anti-citrullinated protein antibodies (ACPAs) has been associated with a greater interstitial lung disease (ILD) extent in adults with RA. The aim of this study was to determine whether greater numbers of positive ACPAs are associated with ILA in community-dwelling adults.
Methods: The Multi-Ethnic Study of Atherosclerosis (MESA) is a multi-center, prospective cohort study of 6814 adults aged 45-84 when recruited in 2000-2002 (Exam 1) from 6 US sites. 29 ACPAs (Table 1) were measured via Bio-Plex bead array in 1949 participants at Exams 2 or 3 (2003-2005) as part of the MESA Abdominal Aortic Calcium ancillary study. 2430 full lung CTs from Exam 5 (2010-2012) had ILA assessments performed by 1 of 5 trained thoracic radiologists. ILA was defined as the presence of ground glass abnormalities, reticular abnormalities, nonemphysematous cysts, honeycombing, and traction bronchiectasis affecting >5% of any lung zone in a non-dependent fashion. A positive ACPA was defined as a titer > 75th percentile. The number of positive ACPA was modeled as the independent continuous variable of interest in a logistic regression model with ILA as the dependent variable, adjusting for age, sex, race/ethnicity, education, cigarette pack-years, and smoking status.
Results: 868 participants had ACPAs measured at Exams 2 or 3 and underwent full lung CT at Exam 5. Median age was 58 (IQR 52-66) years. 50% were female, 42% White, 21% African American, 13% Chinese American, and 24% Hispanic (Table 2). Median number of positive ACPA was 2 (IQR 1-13). 100 participants (11.5%) had ILA on CT. We detected an inverse relationship between number of positive ACPA and odds of ILA in univariate and multivariable models. In the unadjusted model, each 1 unit increase in number of positive ACPA was associated with a 37% decrease in odds of ILA (OR 0.63, 95% CI 0.39 – 1.03, p= 0.06). In a fully adjusted model, each 1 unit increase in number of positive ACPA was associated with an 18% decrease in odds of ILA (OR 0.82, 95% CI 0.67 – 0.98, p= 0.047). In a fully adjusted model, the p-value for interaction between number of positive ACPA and race/ethnicity was 0.04. In fully adjusted models, each 1 unit increase in number of positive ACPA was associated with a 40% decrease in odds of ILA among African American participants (OR 0.60, 95% CI 0.37 – 0.95, p=0.03) and a 42% decrease in odds of ILA among Hispanic participants (OR 0.58, 95% CI 0.37 – 0.90, p=0.02; Table 3). There was no significant association between number of positive ACPA and ILA among White or Chinese American participants.
Conclusion: In this large population-based multi-ethnic study, an expanded ACPA repertoire was associated with a lower burden of ILA on CT, especially among African American and Hispanic participants. This finding was unexpected given the known positive relationship between ILD and an expanded ACPA repertoire in adults with RA. Further studies are necessary to explore whether ACPAs may reduce the risk of ILD in African American and Hispanic adults.
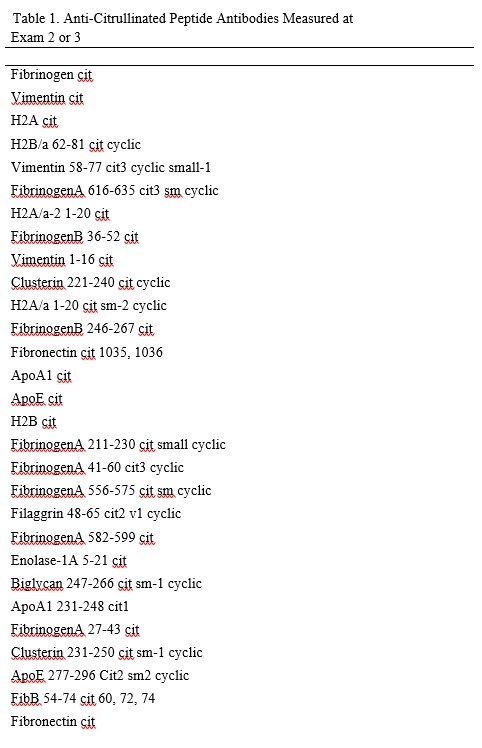 Table 1. Anti-Citrullinated Peptide Antibodies Measured at Exam 2 or 3
Table 1. Anti-Citrullinated Peptide Antibodies Measured at Exam 2 or 3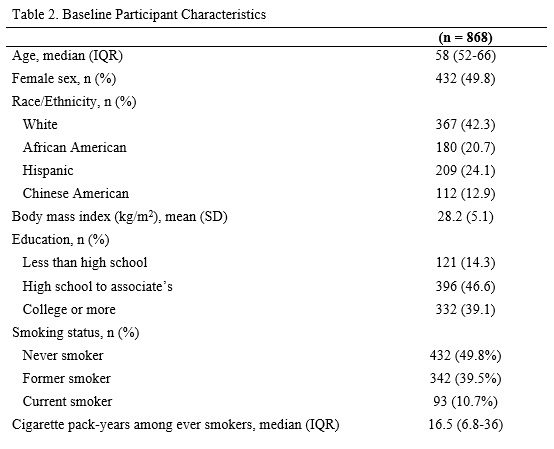 Table 2. Baseline Participant Characteristics
Table 2. Baseline Participant Characteristics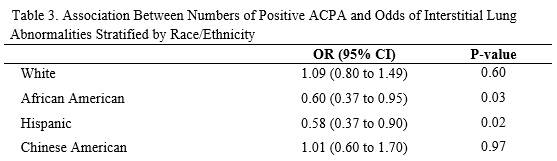 Table 3. Association Between Numbers of Positive ACPA and Odds of Interstitial Lung Abnormalities Stratified by Race/Ethnicity
Table 3. Association Between Numbers of Positive ACPA and Odds of Interstitial Lung Abnormalities Stratified by Race/EthnicityDisclosures: J. Lanz, None; J. Hughes-Austin, None; A. Podolanczuk, Boehringer-Ingelheim, Roche, Imvaria, Regeneron; J. Kim, None; J. Austin, None; W. Robinson, None; G. Raghu, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Roche, Genentech; E. Hoffman, None; J. Newell Jr, VIDA, Elsevier Publishing; J. Watts Jr, Boehringer-Ingelheim, Genentech; P. Nath, None; S. Sonavane, None; R. Barr, None; E. Bernstein, Boehringer-Ingelheim, Kadmon, Pfizer.

