Back
Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1486–1517) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
1498: The Association Between Sonographic Enthesitis with Sonographic Synovitis and Tenosynovitis in Psoriatic Arthritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AP
Ari Polachek, MD
Sourasky Medical Center, Tel-Aviv, Israel
Petah-Tikva, Israel
Abstract Poster Presenter(s)
gavriel Balulu1, Victoria Furer1, Jonathan Wollman2, David Levartovsky1, Valerie Aloush1, Ofir Elalouf1, Hagit Sarbagil-Maman3, Liran Mendel2, Sara Borok1, Daphna Paran1, Ori Elkayam3 and Ari Polachek1, 1Tel Aviv Medical Center, Tel Aviv, Israel, 2Department of Rheumatology, Tel Aviv Sourasky Medical Center, Tel Aviv University, Tel Aviv, Israel, 3Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
Background/Purpose: Enthesitis is considered a hallmark of psoriatic arthritis (PsA). Ultrasound (US) is considered a more accurate tool for the assessment of enthesitis compared to physical examination. Data on the relationship between sonographic enthesitis and other sonographic features, such as synovitis or tenosynovitis, are limited. Hence, the aim of the study was to explore the association of sonographic enthesitis with sonographic synovitis and tenosynovitis in patients with PsA. In addition, to examine the association of sonographic enthesitis with clinical characteristics.
Methods: The study population included consecutive prospectively recruited PsA patients that fulfilled the classification for psoriatic arthritis (CASPAR criteria). Each patient was assessed by a detailed clinical evaluation and comprehensive sonographic assessment (gray scale and Doppler), including 52 joints, 40 tendons, and 14 points of entheses (according to the MASEI index plus lateral epicondyles) performed at the same day by an experienced sonographer blinded to the clinical data. The US scores calculation was based on the MAdrid Sonography Enthesitis Index (MASEI) scoring system for enthesitis, EULAR synovitis score for synovitis, and a sum of gray scale and Doppler scoring for tenosynovitis. The US enthesitis score was further categorized to inflammatory (hypoechogenicity, thickening, bursitis and Doppler) and structural category (enthesophytes/calcifications and erosions). The statistical analysis included descriptive data as well as linear regression models for association analyses.
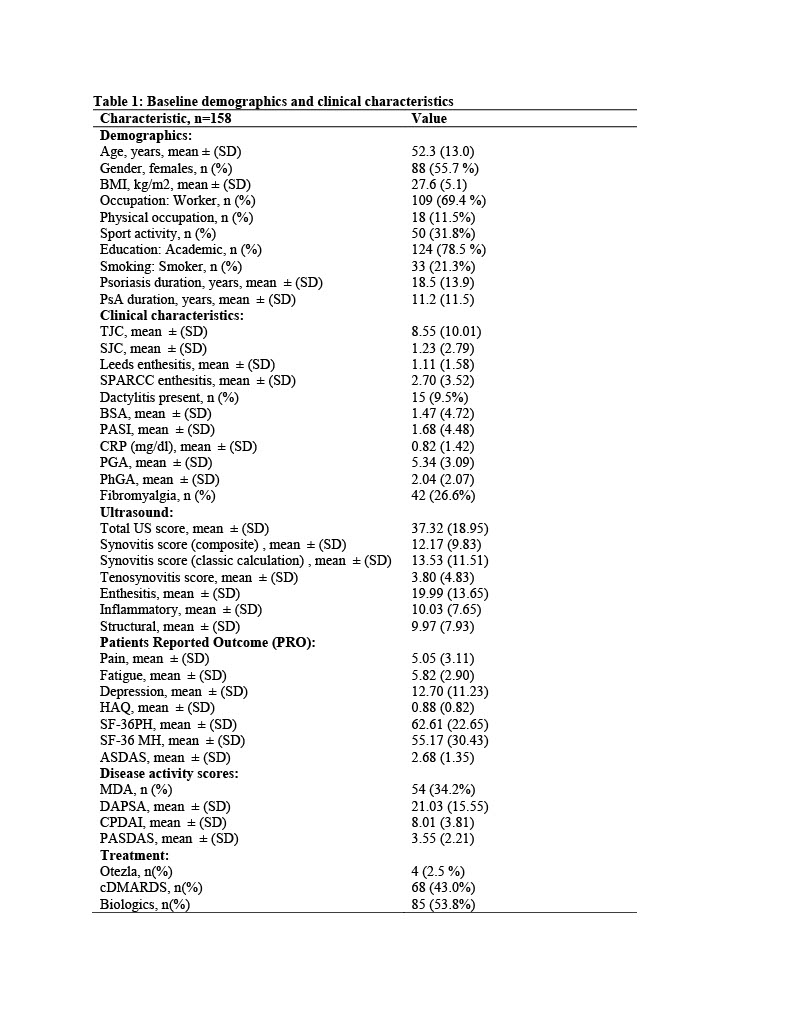
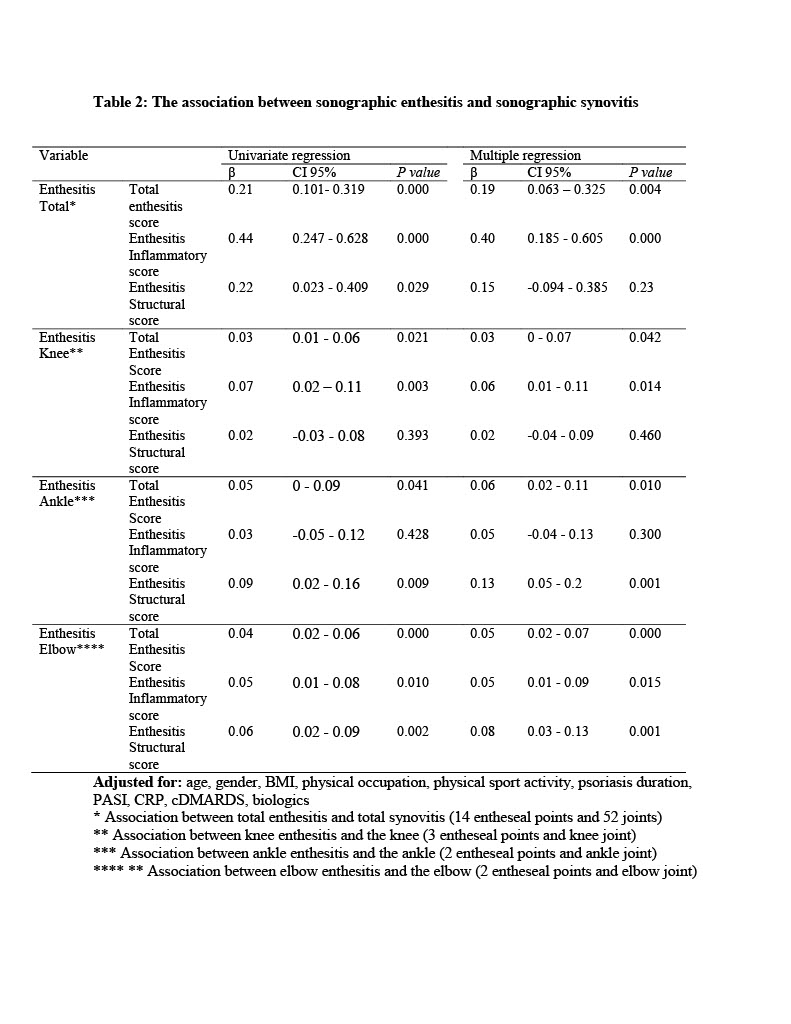
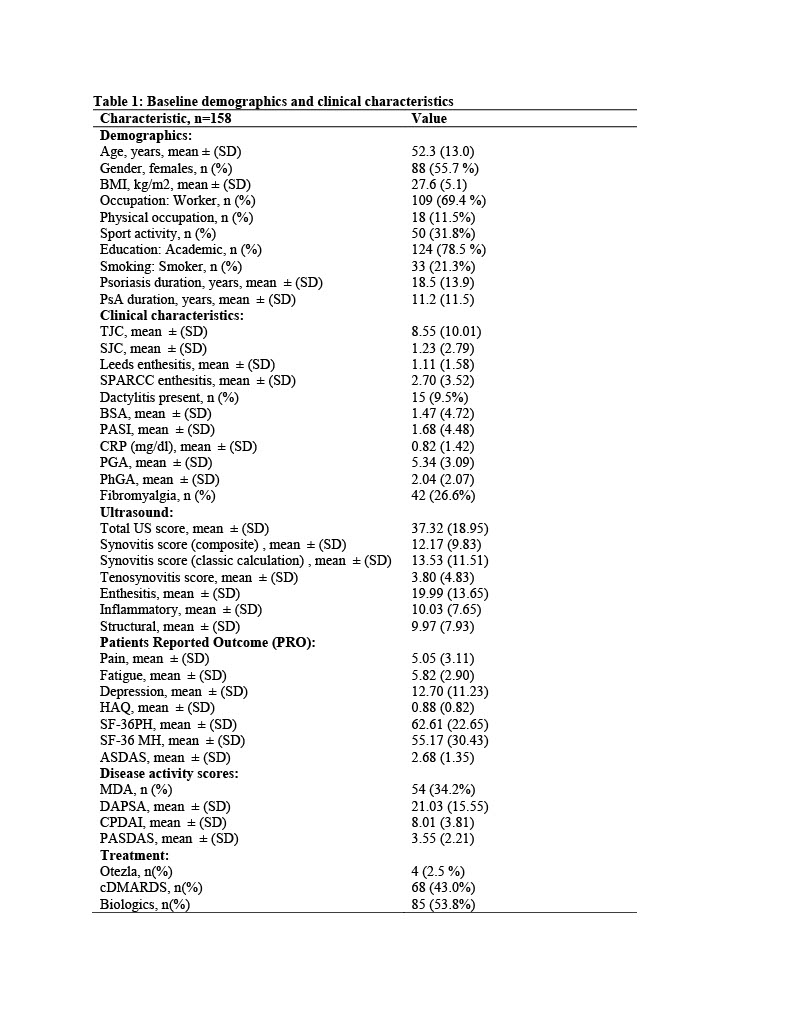
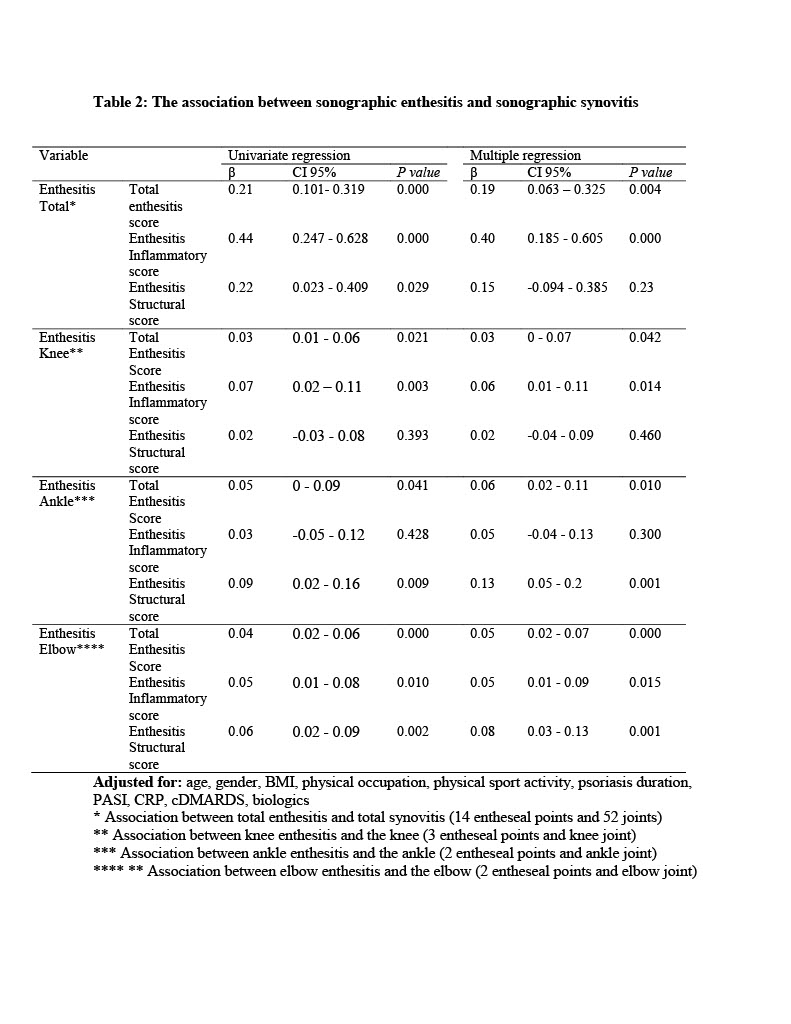
Results: One hundred and fifty-eight PsA patients were analyzed, including 55.7% females, with a mean ± SD age of 52.3 ± 13 years and PsA duration of 11.2 ± 11.5 years (Table 1). Multivariate linear regression analyses showed an independent association between sonographic enthesitis and sonographic synovitis (β=0.19, p=0.004) and between sonographic enthesitis and sonographic tenosynovitis (β=0.1, p=0.003) (Table 2). These associations derived from the sonographic enthesitis inflammatory subcategory (p< 0.01). Further multivariate linear regression analyses on the level of specific joints and related entheses showed an independent association between sonographic elbow enthesitis (insertion of common extensor tendon and triceps) and sonographic elbow synovitis (β=0.05, p=0.001), sonographic knee enthesitis (insertion of quadriceps, distal patella and tibial tuberosity) and sonographic knee synovitis (β=0.03, p=0.04), and sonographic ankle enthesitis (insertion of Achilles and plantar fascia) and sonographic ankle synovitis (β=0.06, p=0.01) (Table 2). Finally, sonographic enthesitis was significantly and independently associated with male gender, older age, physical occupation, swollen join count (SJC) and CRP (Table 3).
Conclusion: Sonographic enthesitis is associated with sonographic synovitis and tenosynovitis. Hence, sonographic enthesitis may signify a marker for inflammatory activity in other musculoskeletal domains.
.jpg)
Disclosures: g. Balulu, None; V. Furer, None; J. Wollman, None; D. Levartovsky, None; V. Aloush, None; O. Elalouf, None; H. Sarbagil-Maman, None; L. Mendel, None; S. Borok, None; D. Paran, None; O. Elkayam, Pfizer, Eli Lilly, AbbVie/Abbott, Novartis, Janssen, Boehringer-Ingelheim; A. Polachek, None.
Background/Purpose: Enthesitis is considered a hallmark of psoriatic arthritis (PsA). Ultrasound (US) is considered a more accurate tool for the assessment of enthesitis compared to physical examination. Data on the relationship between sonographic enthesitis and other sonographic features, such as synovitis or tenosynovitis, are limited. Hence, the aim of the study was to explore the association of sonographic enthesitis with sonographic synovitis and tenosynovitis in patients with PsA. In addition, to examine the association of sonographic enthesitis with clinical characteristics.
Methods: The study population included consecutive prospectively recruited PsA patients that fulfilled the classification for psoriatic arthritis (CASPAR criteria). Each patient was assessed by a detailed clinical evaluation and comprehensive sonographic assessment (gray scale and Doppler), including 52 joints, 40 tendons, and 14 points of entheses (according to the MASEI index plus lateral epicondyles) performed at the same day by an experienced sonographer blinded to the clinical data. The US scores calculation was based on the MAdrid Sonography Enthesitis Index (MASEI) scoring system for enthesitis, EULAR synovitis score for synovitis, and a sum of gray scale and Doppler scoring for tenosynovitis. The US enthesitis score was further categorized to inflammatory (hypoechogenicity, thickening, bursitis and Doppler) and structural category (enthesophytes/calcifications and erosions). The statistical analysis included descriptive data as well as linear regression models for association analyses.
Results: One hundred and fifty-eight PsA patients were analyzed, including 55.7% females, with a mean ± SD age of 52.3 ± 13 years and PsA duration of 11.2 ± 11.5 years (Table 1). Multivariate linear regression analyses showed an independent association between sonographic enthesitis and sonographic synovitis (β=0.19, p=0.004) and between sonographic enthesitis and sonographic tenosynovitis (β=0.1, p=0.003) (Table 2). These associations derived from the sonographic enthesitis inflammatory subcategory (p< 0.01). Further multivariate linear regression analyses on the level of specific joints and related entheses showed an independent association between sonographic elbow enthesitis (insertion of common extensor tendon and triceps) and sonographic elbow synovitis (β=0.05, p=0.001), sonographic knee enthesitis (insertion of quadriceps, distal patella and tibial tuberosity) and sonographic knee synovitis (β=0.03, p=0.04), and sonographic ankle enthesitis (insertion of Achilles and plantar fascia) and sonographic ankle synovitis (β=0.06, p=0.01) (Table 2). Finally, sonographic enthesitis was significantly and independently associated with male gender, older age, physical occupation, swollen join count (SJC) and CRP (Table 3).
Conclusion: Sonographic enthesitis is associated with sonographic synovitis and tenosynovitis. Hence, sonographic enthesitis may signify a marker for inflammatory activity in other musculoskeletal domains.
.jpg)
Disclosures: g. Balulu, None; V. Furer, None; J. Wollman, None; D. Levartovsky, None; V. Aloush, None; O. Elalouf, None; H. Sarbagil-Maman, None; L. Mendel, None; S. Borok, None; D. Paran, None; O. Elkayam, Pfizer, Eli Lilly, AbbVie/Abbott, Novartis, Janssen, Boehringer-Ingelheim; A. Polachek, None.

