Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1191: The Risk of Major Adverse Cardiovascular Events in Patients with Systemic Sclerosis: A Population-Based, Matched Cohort Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- TY
Tsai-Hung Yen, MD
Taichung Veterans General Hospital
Xitun District, Taichung City, Taiwan
Abstract Poster Presenter(s)
HSIN-HUA CHEN1 and Tsai-Hung Yen2, 1Taichung Veterans General Hospital, Taichung, Taiwan, 2Division of General Medicine, Division of Allergy, Immunology and Rheumatology, Taichung Veterans General Hospital, Taichung, Taiwan
Background/Purpose: The pathologic hallmarks of systemic sclerosis (SSc) included a non-inflammatory obliterative vasculopathy affecting small arteries and arterioles in multiple vascular beds. Whether macrovascular involvement was more prevalent in patients with SSc was still controversial. Therefore, we conducted a nationwide, population-based cohort study to assess the risk of major adverse cardiovascular events (MACE) in incident SSc patients.
Methods: Claim data from the 1997–2013 Taiwanese National Health Insurance Research Database was used to identify newly diagnosed SSc patients from 2001 to 2013. We selected age, sex and year of index date-matched (1:20) non-SSc individuals from claim data of one million representative individuals enrolled in 2000 (LHID2000) in Taiwan. Therefore, 1,611 SSc patients and 32,220 non-SSc individuals were included. From this age-sex matched population, we further selected SSc patients and non-SSc individuals via propensity-score (PS) matching (1:2) for age, sex, and selected comorbidities confounders using the greedy algorithm. Ultimately, we identified 1,379 SSc patients and 2,758 PSM-matched non-SSc individuals, with balanced baseline characteristics between groups. The primary outcome was MACE which was composed of myocardial infarction, ischemic stroke and patients undergoing percutaneous coronary intervention or coronary artery bypass graft. We calculated the incidences of MACE of both groups in the PSM population and estimated the association between SSc and the risk of MACE using a time-dependent conditional Cox regression models adjusting for level of urbanization of residence, low income, a history of MACE and concomitant medications including use of aspirin, clopidogrel, dipyridamole and warfarin shown as adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
Results: During the mean follow-up of 5.23 and 6.20 years in SSc patients and non-SSc individuals,
the incidence rates of MACE were not significantly different between groups (1,012 vs 882 cases per 105 person-years, incidence rate ratio (IRR), 1.15; 95% CI, 0.87–1.52, p = 0.337). However, SSc patients had a higher incidence of myocardial infarction (IRR, 1.76; 95% CI, 1.08-2.86) but not ischemic stroke (IRR, 0.89, 95%CI 0.61-1.29). Using the crude and adjusted time-dependent conditional Cox regression analyses, SSc was not associated with the risk of MACE (crude HR, 1.28, 95% CI, 0.91–1.82; aHR, 0.88; 95% CI, 0.49–1.58) Other predictors for MACE included a history of MACE (HR, 2.62; 95% CI, 1.08-2.86), use of clopidogrel (aHR, 19.72; 95% CI, 6.77–57.42), use of aspirin (aHR, 9.41; 95%, CI 4.43–19.99) and use of warfarin (aHR 3.91, 95% CI 1.11–13.72).
Conclusion: This nationwide, population-based cohort study did not reveal and increased risk of MACE in incident SSc patients. However, the incidence of myocardial infarction was significantly higher in SSc patients compared with PS-matched non-SSc individuals.
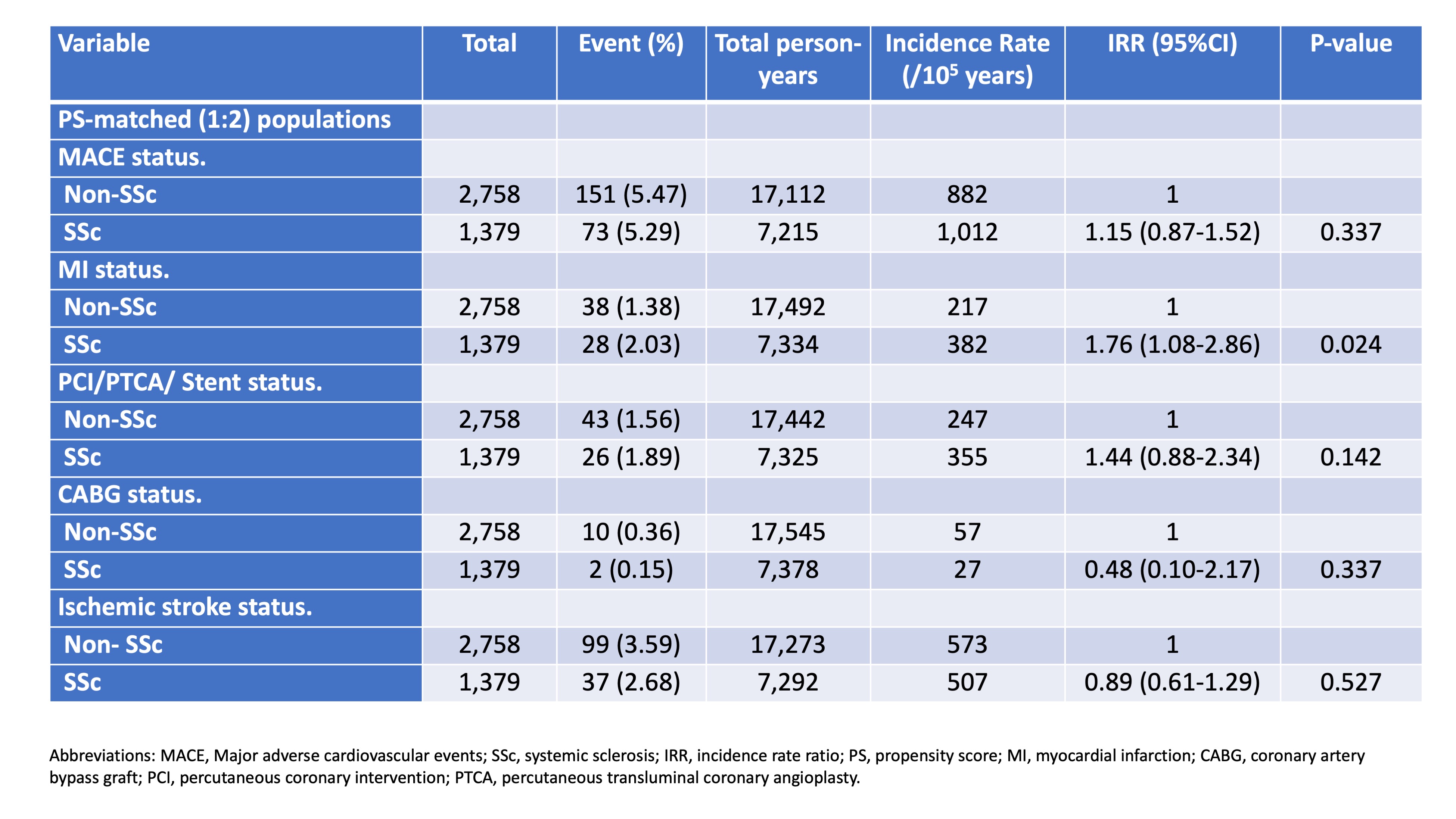 Table. Incidences of MACE in SSc patients and non-SSc individuals
Table. Incidences of MACE in SSc patients and non-SSc individuals
Disclosures: H. CHEN, None; T. Yen, None.
Background/Purpose: The pathologic hallmarks of systemic sclerosis (SSc) included a non-inflammatory obliterative vasculopathy affecting small arteries and arterioles in multiple vascular beds. Whether macrovascular involvement was more prevalent in patients with SSc was still controversial. Therefore, we conducted a nationwide, population-based cohort study to assess the risk of major adverse cardiovascular events (MACE) in incident SSc patients.
Methods: Claim data from the 1997–2013 Taiwanese National Health Insurance Research Database was used to identify newly diagnosed SSc patients from 2001 to 2013. We selected age, sex and year of index date-matched (1:20) non-SSc individuals from claim data of one million representative individuals enrolled in 2000 (LHID2000) in Taiwan. Therefore, 1,611 SSc patients and 32,220 non-SSc individuals were included. From this age-sex matched population, we further selected SSc patients and non-SSc individuals via propensity-score (PS) matching (1:2) for age, sex, and selected comorbidities confounders using the greedy algorithm. Ultimately, we identified 1,379 SSc patients and 2,758 PSM-matched non-SSc individuals, with balanced baseline characteristics between groups. The primary outcome was MACE which was composed of myocardial infarction, ischemic stroke and patients undergoing percutaneous coronary intervention or coronary artery bypass graft. We calculated the incidences of MACE of both groups in the PSM population and estimated the association between SSc and the risk of MACE using a time-dependent conditional Cox regression models adjusting for level of urbanization of residence, low income, a history of MACE and concomitant medications including use of aspirin, clopidogrel, dipyridamole and warfarin shown as adjusted hazard ratios (aHR) with 95% confidence intervals (CI).
Results: During the mean follow-up of 5.23 and 6.20 years in SSc patients and non-SSc individuals,
the incidence rates of MACE were not significantly different between groups (1,012 vs 882 cases per 105 person-years, incidence rate ratio (IRR), 1.15; 95% CI, 0.87–1.52, p = 0.337). However, SSc patients had a higher incidence of myocardial infarction (IRR, 1.76; 95% CI, 1.08-2.86) but not ischemic stroke (IRR, 0.89, 95%CI 0.61-1.29). Using the crude and adjusted time-dependent conditional Cox regression analyses, SSc was not associated with the risk of MACE (crude HR, 1.28, 95% CI, 0.91–1.82; aHR, 0.88; 95% CI, 0.49–1.58) Other predictors for MACE included a history of MACE (HR, 2.62; 95% CI, 1.08-2.86), use of clopidogrel (aHR, 19.72; 95% CI, 6.77–57.42), use of aspirin (aHR, 9.41; 95%, CI 4.43–19.99) and use of warfarin (aHR 3.91, 95% CI 1.11–13.72).
Conclusion: This nationwide, population-based cohort study did not reveal and increased risk of MACE in incident SSc patients. However, the incidence of myocardial infarction was significantly higher in SSc patients compared with PS-matched non-SSc individuals.
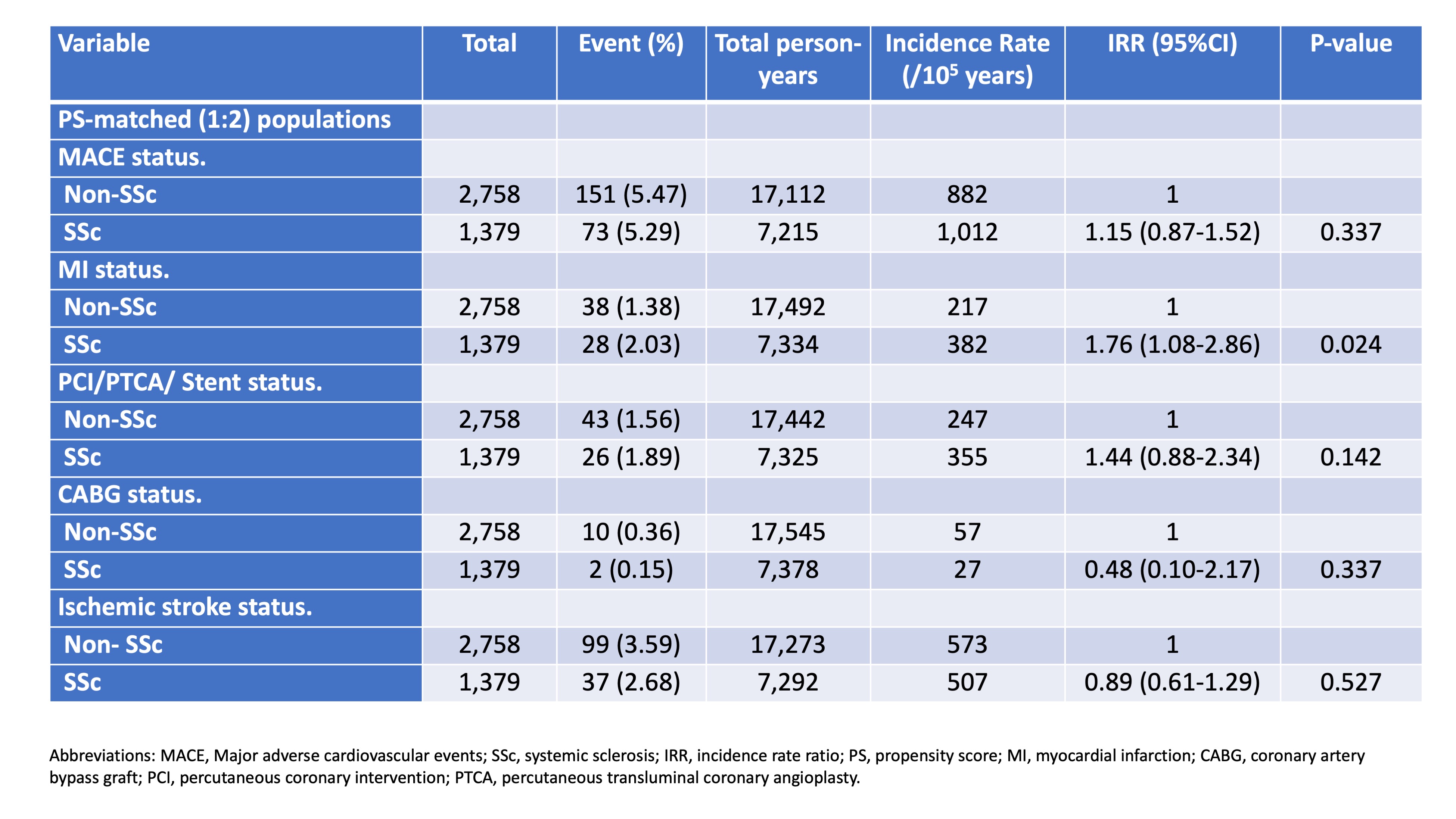 Table. Incidences of MACE in SSc patients and non-SSc individuals
Table. Incidences of MACE in SSc patients and non-SSc individualsDisclosures: H. CHEN, None; T. Yen, None.

