Back
Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1486–1517) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
1512: What Is the Best Referral Strategy for Axial Spondyloarthritis? A Prospective Multicenter Study of 515 Patients with Suspicious Chronic Low Back Pain
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Nelly Ziade, MD, PhD, FRCP
Saint-Joseph University
Beirut, Lebanon
Abstract Poster Presenter(s)
Nelly Ziade1, Avin Maroof2, Bassel Elzorkany3, Nizar Ani4, ASAL ADNAN RIDHA5, Ahmed Abogamal6, Sahar Saad7, Lina El Kibbi8, Samar Al emadi9, Atheer Al Ansari10, Antonella Abi Najm1, Tonine Younan1, Khalil Kharrat1, Joseph Maarrawi1, Amer Sebaaly1, Rami El Rachkidi1, Torsten Witte11 and Xenofon Baraliakos12, 1Saint-Joseph University, Beirut, Lebanon, 2Rizgary Teaching Hospital - Erbil, Erbil, Iraq, 3Department of Rheumatology, Cairo University, Cairo, Egypt, 4Baghdad College of Medicine, Baghdad, Iraq, 5Baghdad Teaching Hospital, Baghdad, Iraq, 6Saudi German Hospital Dubai, Dubai, United Arab Emirates, 7King Hamad University Hospital, Al Sayh, Bahrain, 8Specialized Medical Center, Riyadh, Saudi Arabia, 9Hamad Medical Corporation, Doha, Qatar, 10Mediclinic, Abu Dhabi, United Arab Emirates, 11MH-Hannover, Hannover, Germany, 12Rheumazentrum Ruhrgebiet Herne, Herne, Germany
Background/Purpose: The diagnosis of axial spondyloarthritis (axSpA) is often delayed, due to the referral issues and, in certain regions of the world, the low prevalence of HLA-B27. The objectives of the study were to assess the value of the referral strategies for axSpA in patients with suspicious chronic low back pain (LBP) and to identify the predictive factors of axSpA.
Methods: The study was multicentric, prospective, and conducted in LBP first-line clinics (rheumatology, internal medicine, family medicine, orthopedic surgery, neurosurgery, and neurology). Adult patients aged under 45 years were included in case of LBP "suspicious" of inflammatory nature according to the primary physician and requiring referral to the rheumatologist. The diagnostic properties of the available referral strategies for axSpA (Brandt I, II, III, Hermann, RADAR, RADAR 2/3, MASTER, Braun, CAFASPA and ASAS) and those of Inflammatory Back Pain (IBP) (Calin, Berlin and ASAS classification criteria) were calculated taking the final diagnosis of the reference rheumatologist as the gold standard. A multivariable logistic regression identified the clinical predictive factors of axSpA.
Results: The study included 515 patients from 7 Middle Eastern countries from April 2020 to April 2022. The diagnosis of axSpA was confirmed in 249 patients (48%), refuted in 222 patients (43%), and remained uncertain in 44 patients (9%). The average age of patients was 34.8 years [SD 7.1], 46.1% were males, and the average symptom duration was 5.9 years [SD 4.9] (Table 1). The ASAS criteria were fulfilled in 83.1% of axSpA patients and 2.7% of patients without axSpA. The optimal reference strategy (highest positive likelihood ratio (LR+ 3.3) was the MASTER strategy (Table 2), which comprises IBP, good response to NSAIDs, positive HLA-B27, and SpA family history. Considering strategies not including HLA-B27, the RADAR 2/3 strategy (IBP, good response to NSAIDs, any extra-musculoskeletal manifestation (EMMs)) had a good LR+ of 2.9. The optimal IBP classification criteria were the ASAS criteria (LR+ 2.0). The most predictive factors for a positive axSpA diagnosis were an MRI sacroiliitis, positive HLA-B27, high CRP level, psoriasis, IBP, and longer symptom duration. When considering only clinical features, the most predictive factors were uveitis, IBP, family SpA, psoriasis, enthesitis, and male gender (Table 3).
Conclusion: The optimal reference strategy was the MASTER strategy, a simple strategy based on IBP, good response to NSAIDs, a positive HLA-B27, and family history of SpA. Among clinical factors, IBP and EMMs (uveitis, psoriasis), and family SpA had a crucial role in predicting the diagnosis of axSpA. Increasing physicians' awareness of these clinical features may enhance referral and expedite early diagnosis of axSpA.
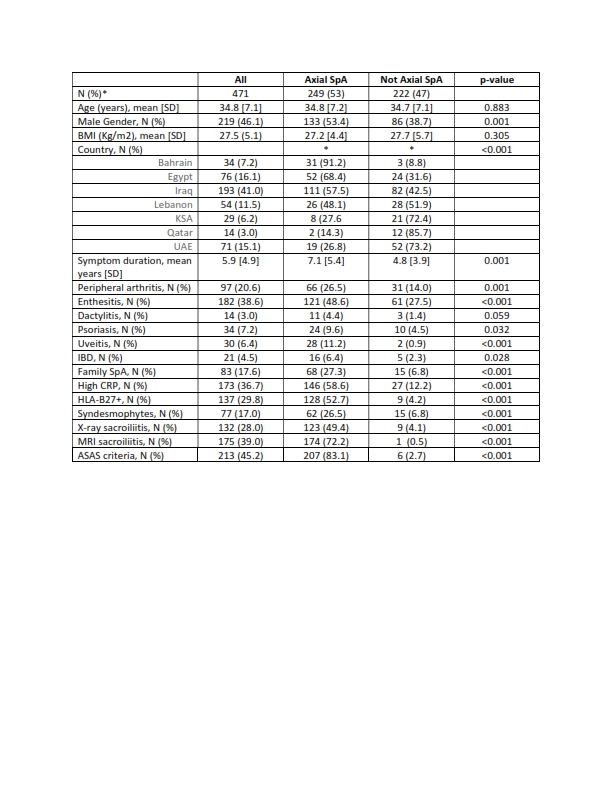 Table 1. Patients’ Characteristics
Table 1. Patients’ Characteristics
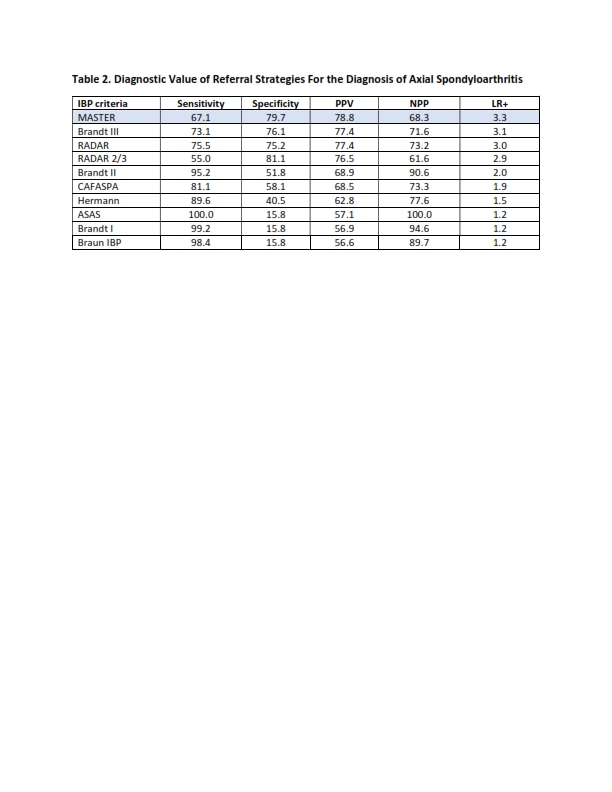 Table 2. Diagnostic Value of Referral Strategies For the Diagnosis of Axial Spondyloarthritis
Table 2. Diagnostic Value of Referral Strategies For the Diagnosis of Axial Spondyloarthritis
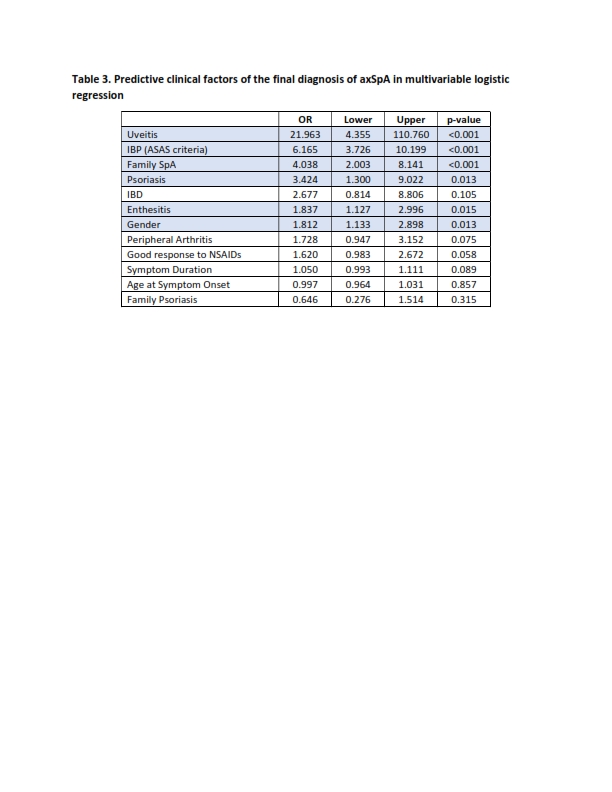 Table 3. Predictive clinical factors of the final diagnosis of axSpA in multivariable logistic regression
Table 3. Predictive clinical factors of the final diagnosis of axSpA in multivariable logistic regression
Disclosures: N. Ziade, Pfizer, Roche, AbbVie/Abbott, Eli Lilly, Boehringer-Ingelheim, Janssen; A. Maroof, None; B. Elzorkany, AbbVie, Amgen, Bristol-Myers Squibb, Eva, Hekma, Janssen, Eli Lilly, MSD, New Bridge, Novartis, Pfizer Inc, Roche, Sanofi-Aventis, Servier; N. Ani, None; A. RIDHA, None; A. Abogamal, None; S. Saad, None; L. El Kibbi, None; S. Al emadi, None; A. Al Ansari, None; A. Abi Najm, None; T. Younan, None; K. Kharrat, None; J. Maarrawi, None; A. Sebaaly, None; R. El Rachkidi, None; T. Witte, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Chugai, Janssen, Lilly, MSD, Mylan, Novartis, Pfizer, Roche, UCB, Galapagos; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi.
Background/Purpose: The diagnosis of axial spondyloarthritis (axSpA) is often delayed, due to the referral issues and, in certain regions of the world, the low prevalence of HLA-B27. The objectives of the study were to assess the value of the referral strategies for axSpA in patients with suspicious chronic low back pain (LBP) and to identify the predictive factors of axSpA.
Methods: The study was multicentric, prospective, and conducted in LBP first-line clinics (rheumatology, internal medicine, family medicine, orthopedic surgery, neurosurgery, and neurology). Adult patients aged under 45 years were included in case of LBP "suspicious" of inflammatory nature according to the primary physician and requiring referral to the rheumatologist. The diagnostic properties of the available referral strategies for axSpA (Brandt I, II, III, Hermann, RADAR, RADAR 2/3, MASTER, Braun, CAFASPA and ASAS) and those of Inflammatory Back Pain (IBP) (Calin, Berlin and ASAS classification criteria) were calculated taking the final diagnosis of the reference rheumatologist as the gold standard. A multivariable logistic regression identified the clinical predictive factors of axSpA.
Results: The study included 515 patients from 7 Middle Eastern countries from April 2020 to April 2022. The diagnosis of axSpA was confirmed in 249 patients (48%), refuted in 222 patients (43%), and remained uncertain in 44 patients (9%). The average age of patients was 34.8 years [SD 7.1], 46.1% were males, and the average symptom duration was 5.9 years [SD 4.9] (Table 1). The ASAS criteria were fulfilled in 83.1% of axSpA patients and 2.7% of patients without axSpA. The optimal reference strategy (highest positive likelihood ratio (LR+ 3.3) was the MASTER strategy (Table 2), which comprises IBP, good response to NSAIDs, positive HLA-B27, and SpA family history. Considering strategies not including HLA-B27, the RADAR 2/3 strategy (IBP, good response to NSAIDs, any extra-musculoskeletal manifestation (EMMs)) had a good LR+ of 2.9. The optimal IBP classification criteria were the ASAS criteria (LR+ 2.0). The most predictive factors for a positive axSpA diagnosis were an MRI sacroiliitis, positive HLA-B27, high CRP level, psoriasis, IBP, and longer symptom duration. When considering only clinical features, the most predictive factors were uveitis, IBP, family SpA, psoriasis, enthesitis, and male gender (Table 3).
Conclusion: The optimal reference strategy was the MASTER strategy, a simple strategy based on IBP, good response to NSAIDs, a positive HLA-B27, and family history of SpA. Among clinical factors, IBP and EMMs (uveitis, psoriasis), and family SpA had a crucial role in predicting the diagnosis of axSpA. Increasing physicians' awareness of these clinical features may enhance referral and expedite early diagnosis of axSpA.
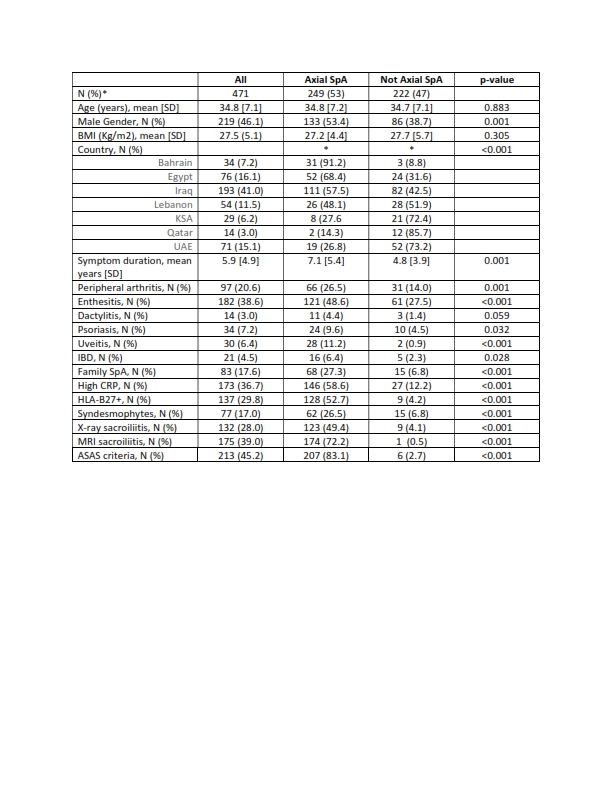 Table 1. Patients’ Characteristics
Table 1. Patients’ Characteristics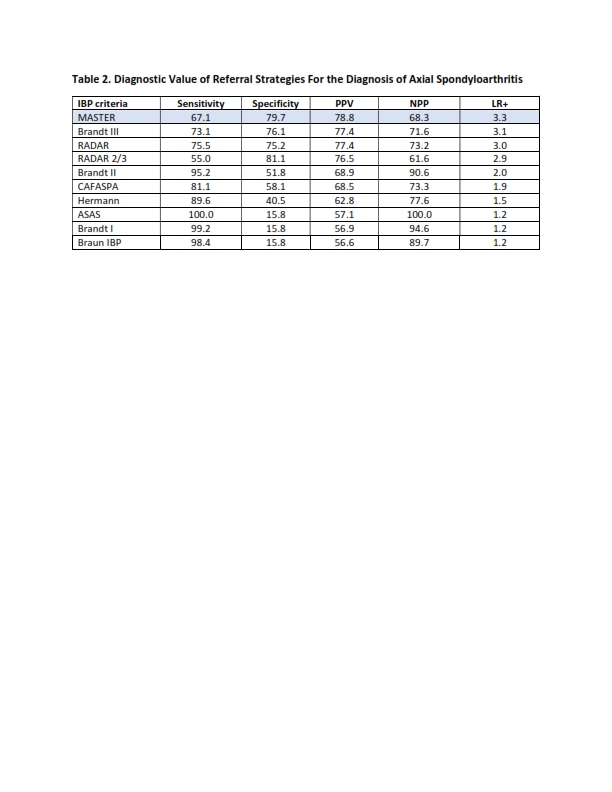 Table 2. Diagnostic Value of Referral Strategies For the Diagnosis of Axial Spondyloarthritis
Table 2. Diagnostic Value of Referral Strategies For the Diagnosis of Axial Spondyloarthritis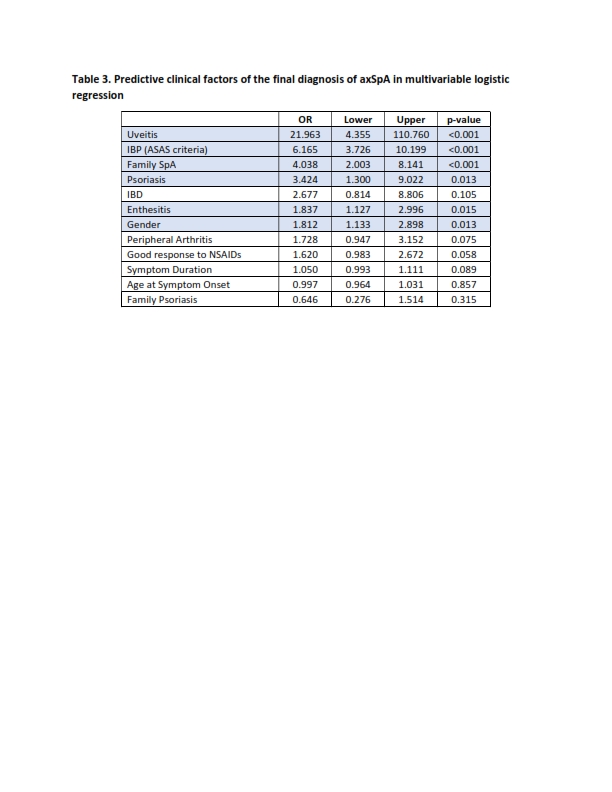 Table 3. Predictive clinical factors of the final diagnosis of axSpA in multivariable logistic regression
Table 3. Predictive clinical factors of the final diagnosis of axSpA in multivariable logistic regressionDisclosures: N. Ziade, Pfizer, Roche, AbbVie/Abbott, Eli Lilly, Boehringer-Ingelheim, Janssen; A. Maroof, None; B. Elzorkany, AbbVie, Amgen, Bristol-Myers Squibb, Eva, Hekma, Janssen, Eli Lilly, MSD, New Bridge, Novartis, Pfizer Inc, Roche, Sanofi-Aventis, Servier; N. Ani, None; A. RIDHA, None; A. Abogamal, None; S. Saad, None; L. El Kibbi, None; S. Al emadi, None; A. Al Ansari, None; A. Abi Najm, None; T. Younan, None; K. Kharrat, None; J. Maarrawi, None; A. Sebaaly, None; R. El Rachkidi, None; T. Witte, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Chugai, Janssen, Lilly, MSD, Mylan, Novartis, Pfizer, Roche, UCB, Galapagos; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi.

