Back
Poster Session A
Epidemiology, health policy and outcomes
Session: (0056–0084) Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
0072: Geographical Patterns of Healthcare Utilization Among RA and OA Patients
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SP
Sofia Pedro, MS
Forward, The National Databank for Rheumatic Diseases
Wichita, KS, United States
Abstract Poster Presenter(s)
Sofia Pedro1, Luke Desilet2, Patricia Katz3 and Kaleb Michaud2, 1Forward, The National Databank for Rheumatic Diseases, Wichita, KS, 2University of Nebraska Medical Center, Omaha, NE, 3UCSF, San Rafael, CA
Background/Purpose: Rural residence has been associated with disparities in healthcare-related outcomes in both rheumatic diseases and other chronic conditions. A primary causal pathway for this may be through having greater difficulty in accessing healthcare. We sought to look at the geographical location and association on healthcare utilization.
Methods: Study participants were enrolled in the FORWARD Databank, a US-wide rheumatic disease longitudinal registry, with an RA or OA diagnosis and a completed 6-month questionnaire. Participant home address was converted into 10 codes using RUCA code version2. This was further aggregated into 3 categories: rural small isolated, large rural, and urban. Healthcare utilization variables such as medical visits and diagnostic tests were analyzed by geographical categories. Anova and chi-squares tests were initially used to look at bivariate analysis between location and utilization. Double selection LASSO with Poisson regression was used to assess the best model when modeling the association between number of medical visits and the geographical location.
Results: Of the 38,569 participants with RA, 74.5% lived in urban areas, 12.3% in large rural areas and 13.2% in small rural areas. For the 8,449 with OA, the distribution was very similar: 75.1% urban, 12.5% large rural and 12.5% small rural. Table 1 presents patients characteristics for both diagnoses. RA patients who lived in urban areas had more medical visits as well as diagnostic tests and rheumatologist visits; for OA only the number of medical visits had a similar pattern (Table 2). After adjusting for demographics, clinical measures, and treatments by using double selection LASSO, RA patients who lived on urban areas had an 19% increase in medical visits per 6 months when compared to small rural areas (Table 3). Even those who lived in large rural areas had a 6% increase on medical visits. For OA patients only when comparing urban vs rural an increase of 13% was observed.
Conclusion: We found that geographical characteristics were associated with healthcare utilization. Patients living in urban areas had considerably more medical visits and diagnostic tests in comparison with those who lived in small rural areas. Future work will examine if these differences impact disease-specific outcomes.
.jpg) Table 1. Patient characteristics by location and disease (RA and OA)
Table 1. Patient characteristics by location and disease (RA and OA)
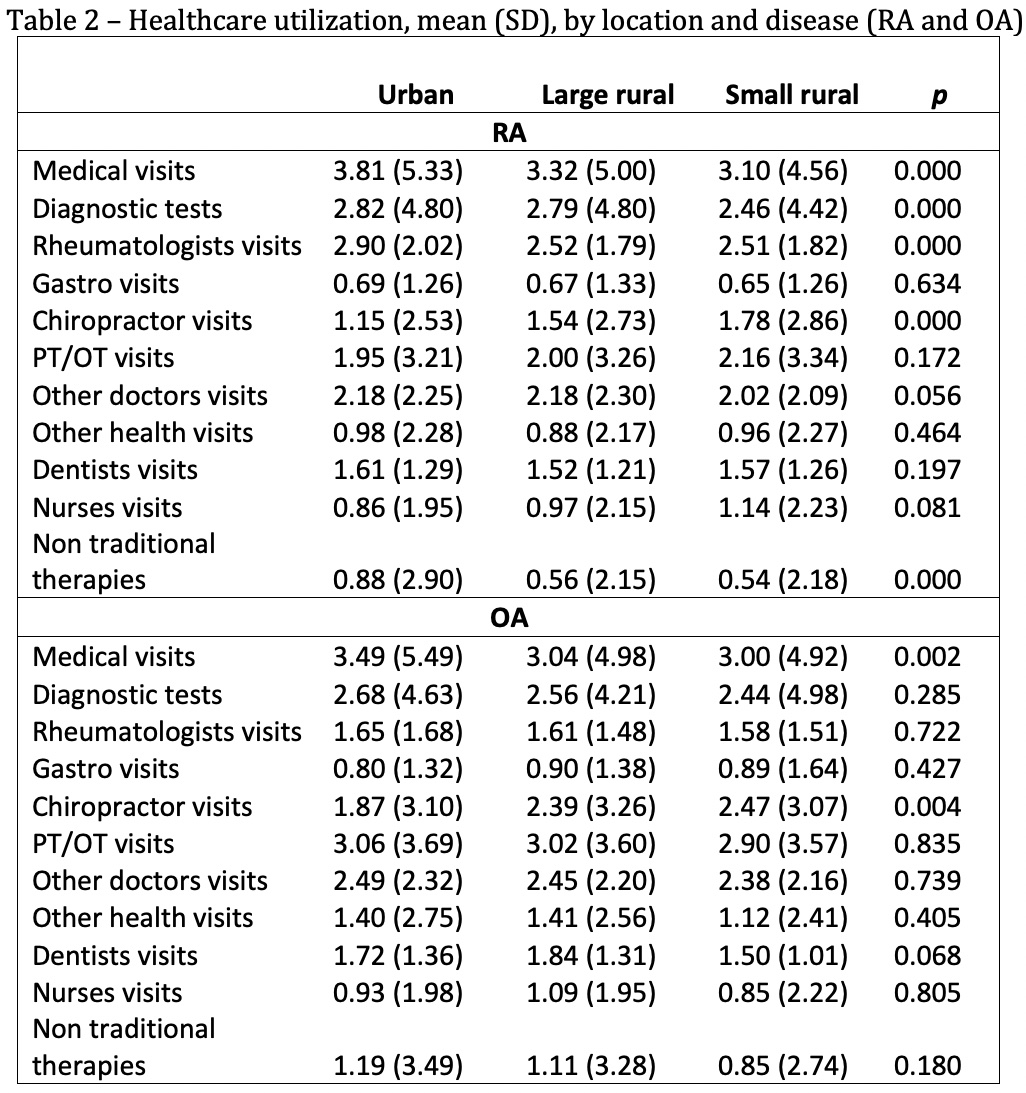 Table 2. Healthcare utilization, mean (SD), by location and disease (RA and OA)
Table 2. Healthcare utilization, mean (SD), by location and disease (RA and OA)
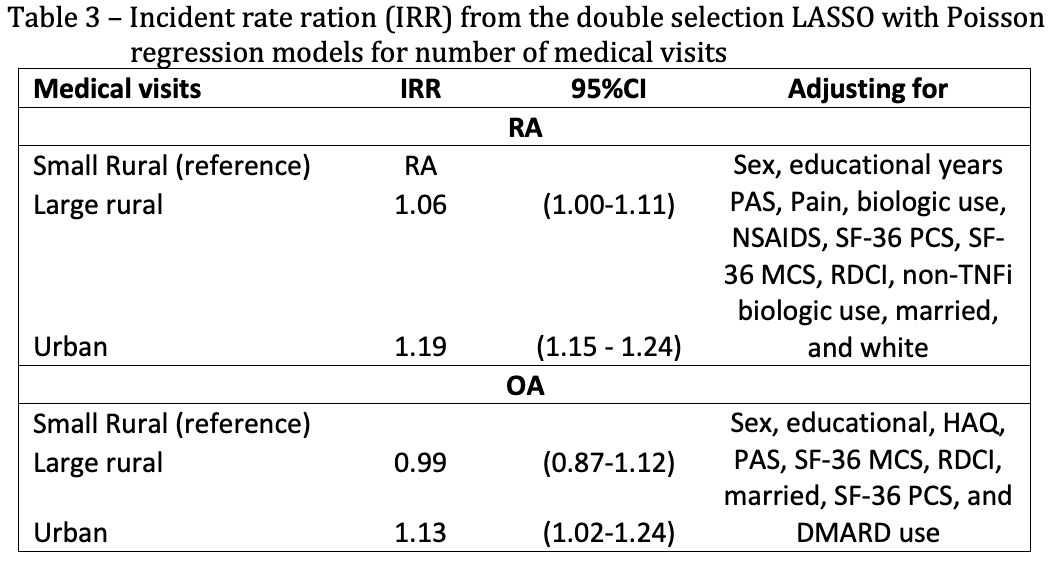 Table 3. Incident rate ration (IRR) from the double selection LASSO with Poisson regression models for number of medical visits
Table 3. Incident rate ration (IRR) from the double selection LASSO with Poisson regression models for number of medical visits
Disclosures: S. Pedro, None; L. Desilet, None; P. Katz, None; K. Michaud, None.
Background/Purpose: Rural residence has been associated with disparities in healthcare-related outcomes in both rheumatic diseases and other chronic conditions. A primary causal pathway for this may be through having greater difficulty in accessing healthcare. We sought to look at the geographical location and association on healthcare utilization.
Methods: Study participants were enrolled in the FORWARD Databank, a US-wide rheumatic disease longitudinal registry, with an RA or OA diagnosis and a completed 6-month questionnaire. Participant home address was converted into 10 codes using RUCA code version2. This was further aggregated into 3 categories: rural small isolated, large rural, and urban. Healthcare utilization variables such as medical visits and diagnostic tests were analyzed by geographical categories. Anova and chi-squares tests were initially used to look at bivariate analysis between location and utilization. Double selection LASSO with Poisson regression was used to assess the best model when modeling the association between number of medical visits and the geographical location.
Results: Of the 38,569 participants with RA, 74.5% lived in urban areas, 12.3% in large rural areas and 13.2% in small rural areas. For the 8,449 with OA, the distribution was very similar: 75.1% urban, 12.5% large rural and 12.5% small rural. Table 1 presents patients characteristics for both diagnoses. RA patients who lived in urban areas had more medical visits as well as diagnostic tests and rheumatologist visits; for OA only the number of medical visits had a similar pattern (Table 2). After adjusting for demographics, clinical measures, and treatments by using double selection LASSO, RA patients who lived on urban areas had an 19% increase in medical visits per 6 months when compared to small rural areas (Table 3). Even those who lived in large rural areas had a 6% increase on medical visits. For OA patients only when comparing urban vs rural an increase of 13% was observed.
Conclusion: We found that geographical characteristics were associated with healthcare utilization. Patients living in urban areas had considerably more medical visits and diagnostic tests in comparison with those who lived in small rural areas. Future work will examine if these differences impact disease-specific outcomes.
.jpg) Table 1. Patient characteristics by location and disease (RA and OA)
Table 1. Patient characteristics by location and disease (RA and OA)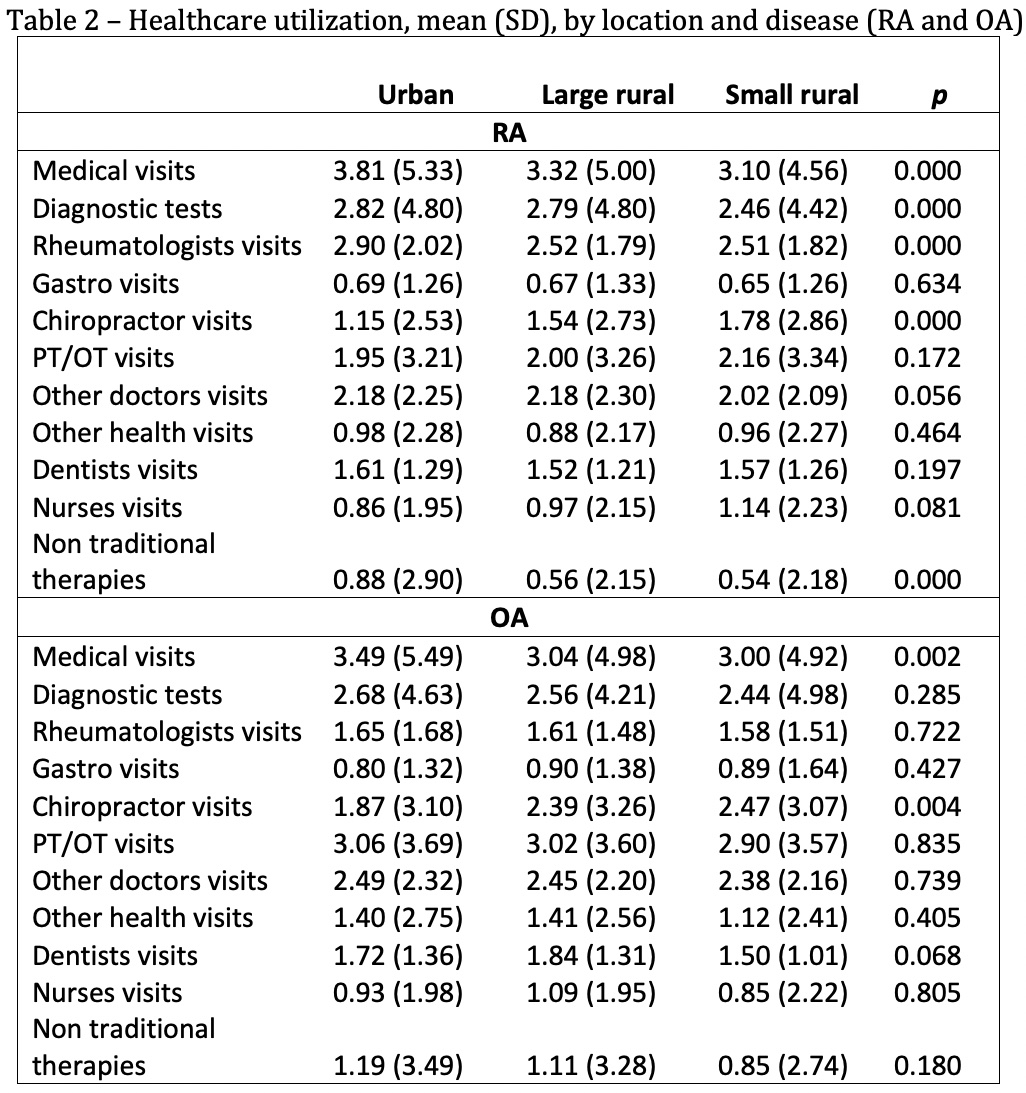 Table 2. Healthcare utilization, mean (SD), by location and disease (RA and OA)
Table 2. Healthcare utilization, mean (SD), by location and disease (RA and OA)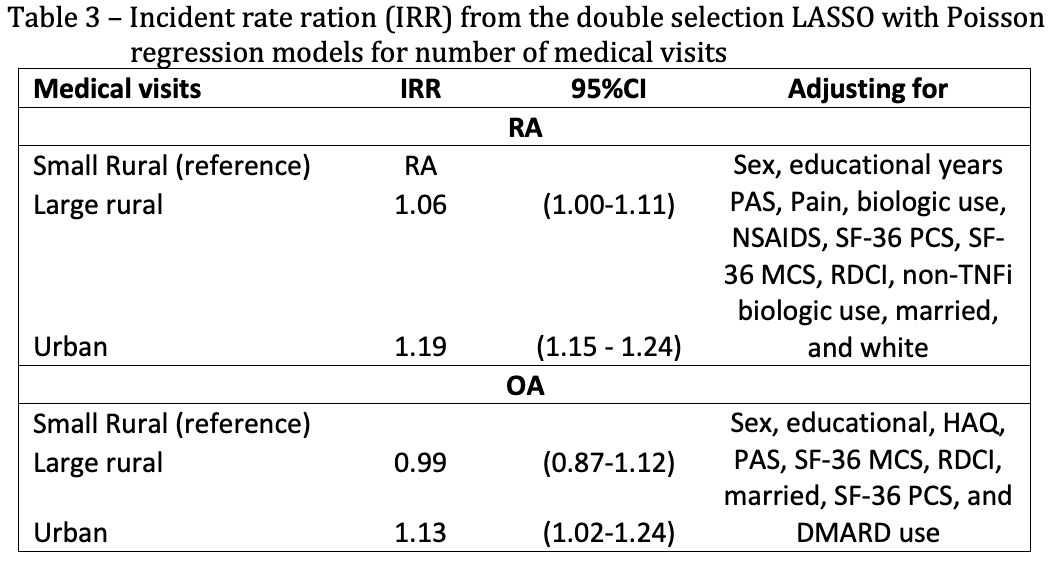 Table 3. Incident rate ration (IRR) from the double selection LASSO with Poisson regression models for number of medical visits
Table 3. Incident rate ration (IRR) from the double selection LASSO with Poisson regression models for number of medical visitsDisclosures: S. Pedro, None; L. Desilet, None; P. Katz, None; K. Michaud, None.

