Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0395: How Does Body Mass Index Affect Secukinumab Treatment Outcomes and Safety in Patients with Psoriatic Arthritis? - Real World Data from a German Observational Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- UK
Uta Kiltz, PhD
Rheumazentrum Ruhrgebiet
D-44649 Herne, Germany
Abstract Poster Presenter(s)
Uta Kiltz1, Jan Brandt-Juergens2, Peter Kästner3, Elke Riechers4, Daniel Peterlik5, Christina Budden5 and Hans-Peter Tony6, 1Rheumazentrum Ruhrgebiet, Herne, Germany, 2Rheumatologische Schwerpunktpraxis, Berlin, Germany, 3Ambulantes Rheumazentrum, Medizinisches Versorgungszentrum, Erfurt, Germany, 4Medizinische Hochschule Hannover, Hannover, Germany, 5Novartis Pharma GmbH, Nürnberg, Germany, 6Medizinische Klinik II - Rheumatologie/Immunologie, Universitätsklinikum Würzburg, Würzburg, Germany
Background/Purpose: There is a higher prevalence of obesity in patients (pts) with psoriatic disease1. The German non-interventional study AQUILA provides real-world data on the influence of body mass index (BMI) of pts with psoriatic arthritis (PsA) on therapeutic effectiveness and safety under treatment with secukinumab, a fully human monoclonal antibody that selectively inhibits IL-17A.
The aims of this interim analysis are to describe selected baseline (BL) demographics and to evaluate secukinumab treatment outcomes on disease activity and impact of disease on health and to report safety profile depending on the BMI of PsA pts.
Methods: AQUILA is an ongoing, multi-center study including up to 3000 pts with active PsA or ankylosing spondylitis. Pts were observed from BL up to week (w) 52. Real-world data were assessed prospectively and analyzed as observed. Data were collected on Psoriatic Arthritis Impact of Disease-12 items (PsAID-12 score) and Patient's Global Assessment (PGA). For calculation of proportion of pts that experienced (serious) adverse events ((S)AEs), all PsA pts were included that received at least one dose of secukinumab. This interim analysis focuses on BMI subgroups ≤25 kg/m2 (normal weight), ˃25 to ≤30 kg/m2 (overweight) and ˃30 kg/m2 (obese) in PsA pts.
Results: At BL, BMI data were available for 1228 PsA pts: 26.5% (n=325) normal weight, 35.0% (n=430) overweight and 38.5% (n=473) obese PsA pts. Proportion of men was lower in normal weight and obese PsA pts. As BMI increased, so did age and comorbidities/extraarticular manifestations (EAMs; Table 1); e.g. percentage of PsA pts with heart-related disease increased from 5.2% in normal weight to 9.3% in obese PsA pts.
Mean PsAID at BL was similar for all BMI subgroups (≤25: 4.7; ˃25-≤30: 4.9; >30: 5.4; Figure 1A). Mean improvement from BL to w52 was 1.9 (40.4%) for normal weight, 1.8 (36.7%) for overweight, and 1.7 (31.5%) for obese PsA pts.
Mean PGA developed in a similar way over time with lowest scores for normal weight and highest scores for obese PsA pts (Figure 1B). Mean improvement from BL to w52 was 2.0 (41.6%) for normal weight, 2.2 (40.7%) for overweight, and 1.8 (32.7%) for obese PsA pts.
The occurrence of AEs/SAEs with or without suspected relationship to secukinumab was most frequent in overweight and obese PsA pts. For example, the percentage of SAEs in normal weight PsA pts was 21.6%, in overweight 26.3% and in obese 25.9%. There were no unexpected safety signals in either subgroup. One male obese PsA patient died. Cause of death was not reported, however, treating physician did not suspect a causal relationship to secukinumab.
Conclusion: In a real-world setting, secukinumab improved impact of disease and patient's global assessment of disease activity in all BMI subgroups of PsA pts. However, normal weight PsA pts had numerically better PsAID and PGA scores than obese PsA pts. Altogether, real-world data of this interim analysis show that secukinumab is an effective treatment with a favorable safety profile up to 52 weeks in PsA pts in all BMI subgroups.
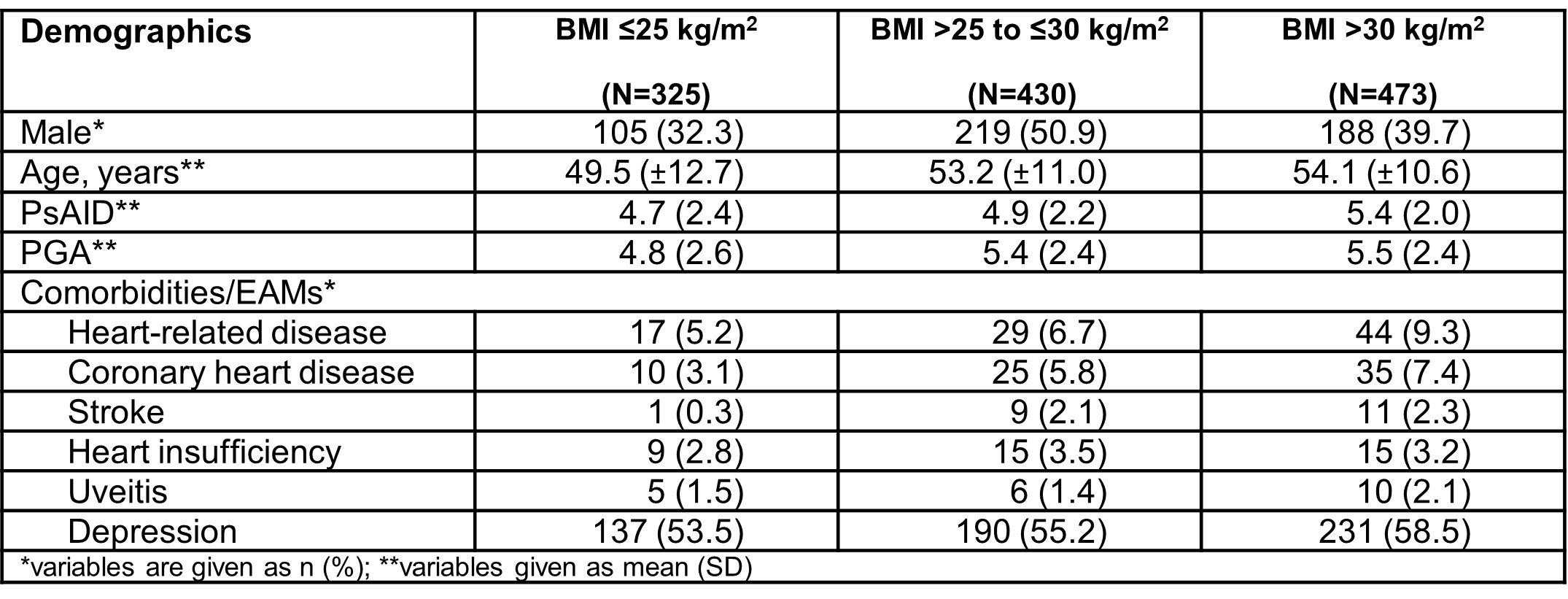 Table 1: Overview of baseline characteristics in PsA pts depending on BMI
Table 1: Overview of baseline characteristics in PsA pts depending on BMI
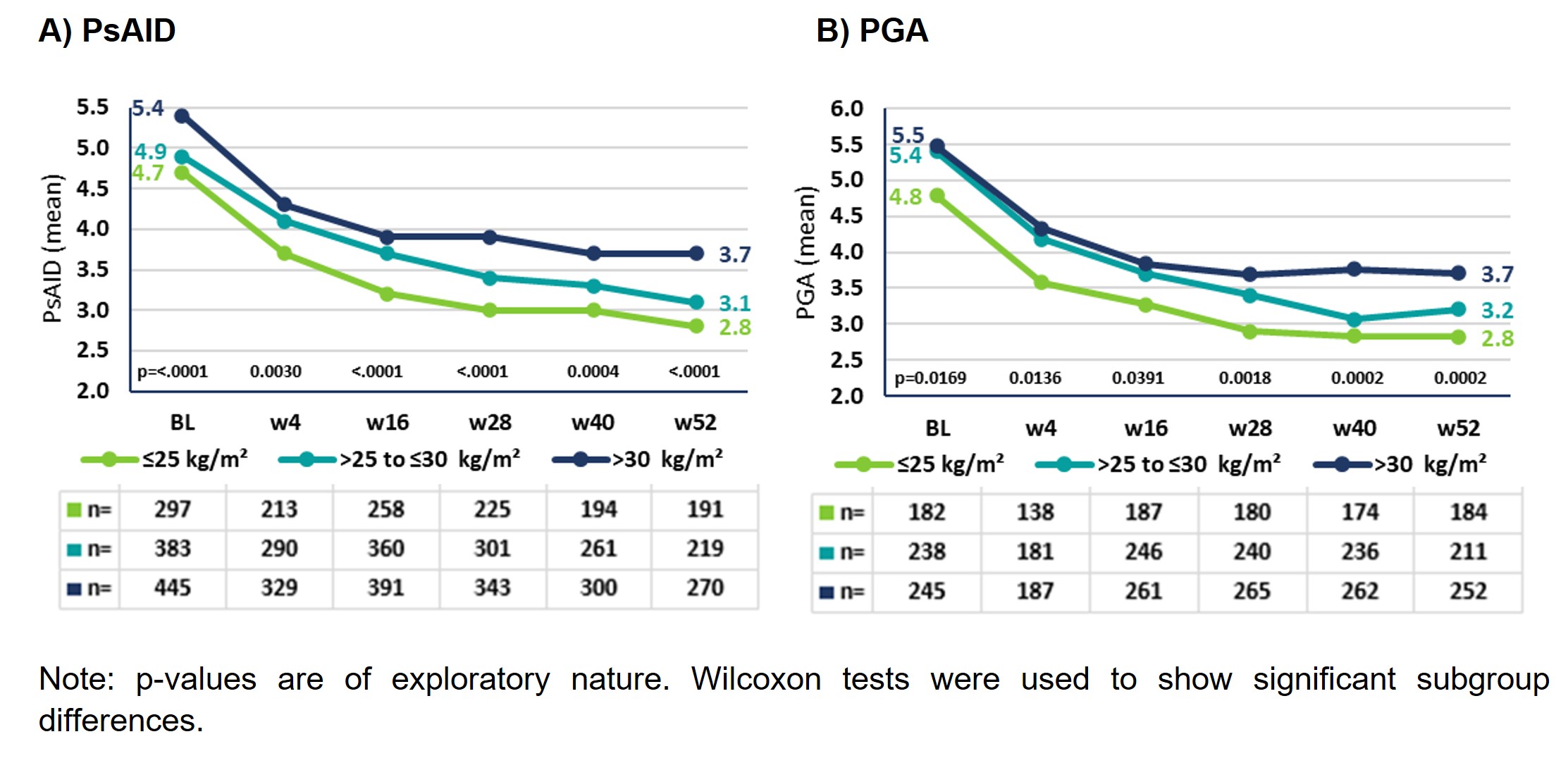 Figure 1: Impact of disease and PGA in PsA pts stratified by BMI
Figure 1: Impact of disease and PGA in PsA pts stratified by BMI
Disclosures: U. Kiltz, AbbVie, Amgen, Biogen, Fresenius, GSK, Hexal, Novartis, Pfizer, Biocad, Lilly, Grünenthal, Janssen, MSD, Roche, UCB; J. Brandt-Juergens, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Janssen, Eli Lilly, Merck/MSD, Novartis, Pfizer, Roche, UCB, Sanofi-Aventis, Medac, Gilead, Gilead, Affibody; P. Kästner, Chugai, Novartis; E. Riechers, AbbVie, Chugai, Lilly, Janssen, Novartis, Pfizer, Roche, UCB; D. Peterlik, Novartis; C. Budden, Novartis; H. Tony, AbbVie, Astra-Zeneca, BMS, Chugai, Janssen, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi.
Background/Purpose: There is a higher prevalence of obesity in patients (pts) with psoriatic disease1. The German non-interventional study AQUILA provides real-world data on the influence of body mass index (BMI) of pts with psoriatic arthritis (PsA) on therapeutic effectiveness and safety under treatment with secukinumab, a fully human monoclonal antibody that selectively inhibits IL-17A.
The aims of this interim analysis are to describe selected baseline (BL) demographics and to evaluate secukinumab treatment outcomes on disease activity and impact of disease on health and to report safety profile depending on the BMI of PsA pts.
Methods: AQUILA is an ongoing, multi-center study including up to 3000 pts with active PsA or ankylosing spondylitis. Pts were observed from BL up to week (w) 52. Real-world data were assessed prospectively and analyzed as observed. Data were collected on Psoriatic Arthritis Impact of Disease-12 items (PsAID-12 score) and Patient's Global Assessment (PGA). For calculation of proportion of pts that experienced (serious) adverse events ((S)AEs), all PsA pts were included that received at least one dose of secukinumab. This interim analysis focuses on BMI subgroups ≤25 kg/m2 (normal weight), ˃25 to ≤30 kg/m2 (overweight) and ˃30 kg/m2 (obese) in PsA pts.
Results: At BL, BMI data were available for 1228 PsA pts: 26.5% (n=325) normal weight, 35.0% (n=430) overweight and 38.5% (n=473) obese PsA pts. Proportion of men was lower in normal weight and obese PsA pts. As BMI increased, so did age and comorbidities/extraarticular manifestations (EAMs; Table 1); e.g. percentage of PsA pts with heart-related disease increased from 5.2% in normal weight to 9.3% in obese PsA pts.
Mean PsAID at BL was similar for all BMI subgroups (≤25: 4.7; ˃25-≤30: 4.9; >30: 5.4; Figure 1A). Mean improvement from BL to w52 was 1.9 (40.4%) for normal weight, 1.8 (36.7%) for overweight, and 1.7 (31.5%) for obese PsA pts.
Mean PGA developed in a similar way over time with lowest scores for normal weight and highest scores for obese PsA pts (Figure 1B). Mean improvement from BL to w52 was 2.0 (41.6%) for normal weight, 2.2 (40.7%) for overweight, and 1.8 (32.7%) for obese PsA pts.
The occurrence of AEs/SAEs with or without suspected relationship to secukinumab was most frequent in overweight and obese PsA pts. For example, the percentage of SAEs in normal weight PsA pts was 21.6%, in overweight 26.3% and in obese 25.9%. There were no unexpected safety signals in either subgroup. One male obese PsA patient died. Cause of death was not reported, however, treating physician did not suspect a causal relationship to secukinumab.
Conclusion: In a real-world setting, secukinumab improved impact of disease and patient's global assessment of disease activity in all BMI subgroups of PsA pts. However, normal weight PsA pts had numerically better PsAID and PGA scores than obese PsA pts. Altogether, real-world data of this interim analysis show that secukinumab is an effective treatment with a favorable safety profile up to 52 weeks in PsA pts in all BMI subgroups.
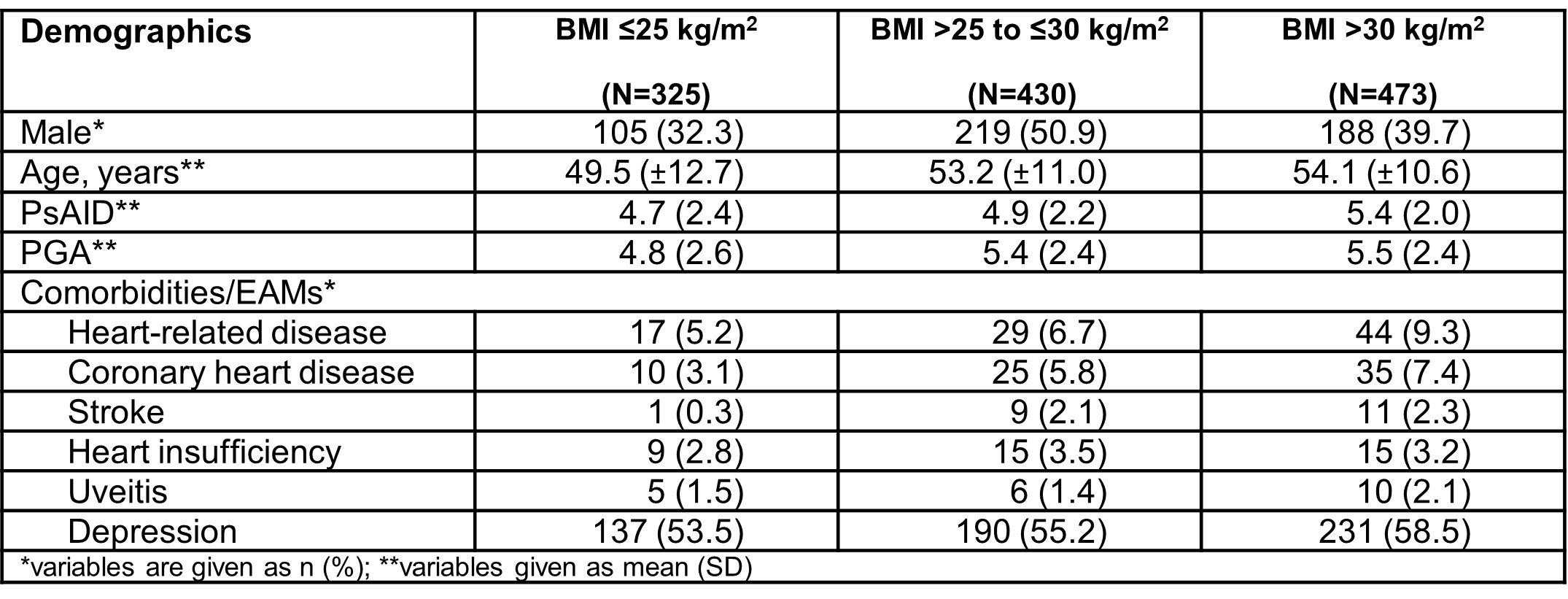 Table 1: Overview of baseline characteristics in PsA pts depending on BMI
Table 1: Overview of baseline characteristics in PsA pts depending on BMI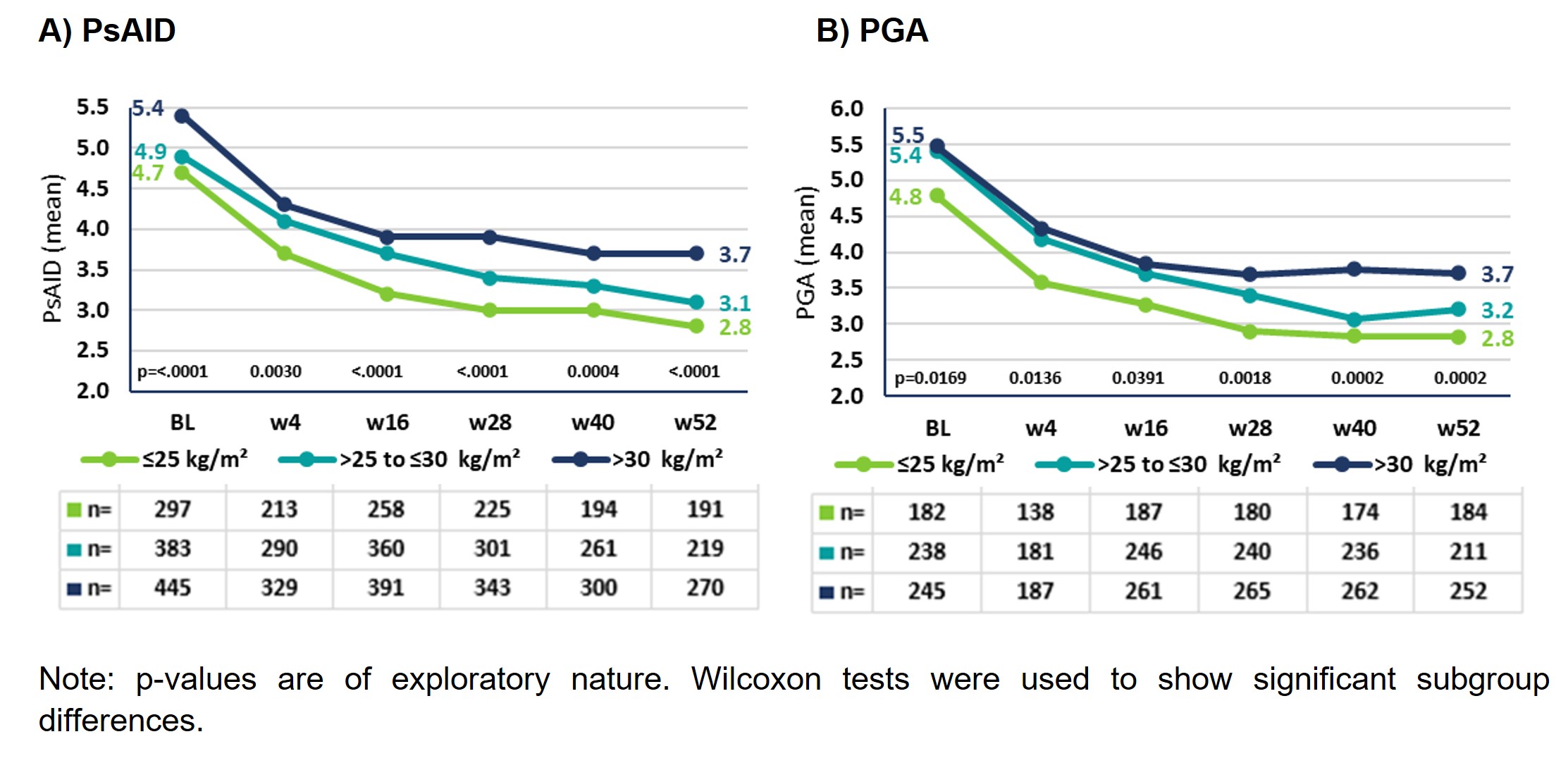 Figure 1: Impact of disease and PGA in PsA pts stratified by BMI
Figure 1: Impact of disease and PGA in PsA pts stratified by BMIDisclosures: U. Kiltz, AbbVie, Amgen, Biogen, Fresenius, GSK, Hexal, Novartis, Pfizer, Biocad, Lilly, Grünenthal, Janssen, MSD, Roche, UCB; J. Brandt-Juergens, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Janssen, Eli Lilly, Merck/MSD, Novartis, Pfizer, Roche, UCB, Sanofi-Aventis, Medac, Gilead, Gilead, Affibody; P. Kästner, Chugai, Novartis; E. Riechers, AbbVie, Chugai, Lilly, Janssen, Novartis, Pfizer, Roche, UCB; D. Peterlik, Novartis; C. Budden, Novartis; H. Tony, AbbVie, Astra-Zeneca, BMS, Chugai, Janssen, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi.

