Back
Poster Session A
Vasculitis
Session: (0432–0457) Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
0450: Incidence of Solid and Hematologic Tumors in Patients with ANCA: A 10-year Retrospective Cohort Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- eb
enrico brunetta
IRCCS Humanitas Research Hospital, Rheumatology and Clinical Immunology
Basiglio, Milan, Italy
Abstract Poster Presenter(s)
Enrico Brunetta1, Giacomo Ramponi2, marco folci2, Maria De Santis3, Giacomo Maria Guidelli1, Angela Ceribelli4, Nicoletta Luciano1, Marta Caprioli5, Arianna Sonaglia1 and Carlo Selmi6, 1IRCCS Humanitas Research Hospital, Rheumatology and Clinical Immunology, Rozzano, Italy, 2IRCCS Humanitas Research Hospital, Internal Medicine, Rozzano, Italy, 3Humanitas University, IRCCS Humanitas Research Hospital, Rheumatology and Clinical Immunology, Pieve Emanuele, Italy, 4Humanitas Research Hospital, Humanitas University, Rozzano (MI) Italy, Borgo San Giacomo, Italy, 5IRCCS Humanitas Research Hospital, Rheumatology and Clinical Immunology, Pavia, Italy, 6IRCCS Humanitas Research Hospital, Humanitas University, Rozzano (MI), Italy, Rozzano, Italy
Background/Purpose: Serum antineutrophil cytoplasmic antibodies (ANCA) are significantly associated with the development of ANCA-associated vasculitides (AAV) but may also be detected in patients with other rheumatologic conditions, chronic infections, among others. Patients with AAV are at higher risk for the onset of malignancies, likely related to the carcinogenic effects of treatment with cyclophosphamide. This has been confirmed by the lower incidence rate of cancer among these patients since when the mainstay of treatment shifted to rituximab. However, the association of ANCA positivity regardless of AAV or other disorders and the development of malignancies has been scarcely investigated.
We investigated the incidence of hematologic or solid cancer in 1,024 subjects with known ANCA status regardless of the indication for the test over 10 years. Our aim was to evaluate whether the presence of serum ANCA, notwithstanding the clinical phenotype, is associated with cancer incidence rate.
Methods: Our retrospective cohort study included 1,024 subjects who underwent ANCA testing at a single centre over 10 years. Time to event was defined as the time from ANCA test until the date of tumour diagnosis or censoring. We compared the incidence of cancer among the ANCA-positive (n=256, including 53 cANCA and 203 pANCA) and ANCA-negative (n=768) patients matched with propensity score (age, gender, time of blood draw), and we evaluated the competing-risks regression model (Fine and Gray) for the two groups.
Results: Out of 61 subjects who were diagnosed with cancer, 49 were ANCA-negative and 12 were ANCA-positive (pANCA positive). The most frequent tumors included hematological (20%) and lung (13%) cancers. Competing-risks regression was limited to ANCA-negative and pANCA-positive patients, due to the lack of cANCA patients with cancer. No relationship was found between pANCA status and incidence of cancer considering adjustment for sex, age and time of blood draw (HR 0.97; 95% CI 0.52-1.83). We were not able to adjust for smoking, drugs and number of comorbidities of each patient. After excluding patients with AAV (36 patients) from the competing-risks regression, results were unchanged (HR 1.00; 95% CI 0.52-1.92).
Conclusion: Serum ANCA positivity is not associated per se with an increased risk of malignancy. Our results further support the plausibility of the hypothesis according to which carcinogenicity in AAV reported in earlier studies was mainly related to the effects of immunosuppressive treatment, in particular with cyclophosphamide.
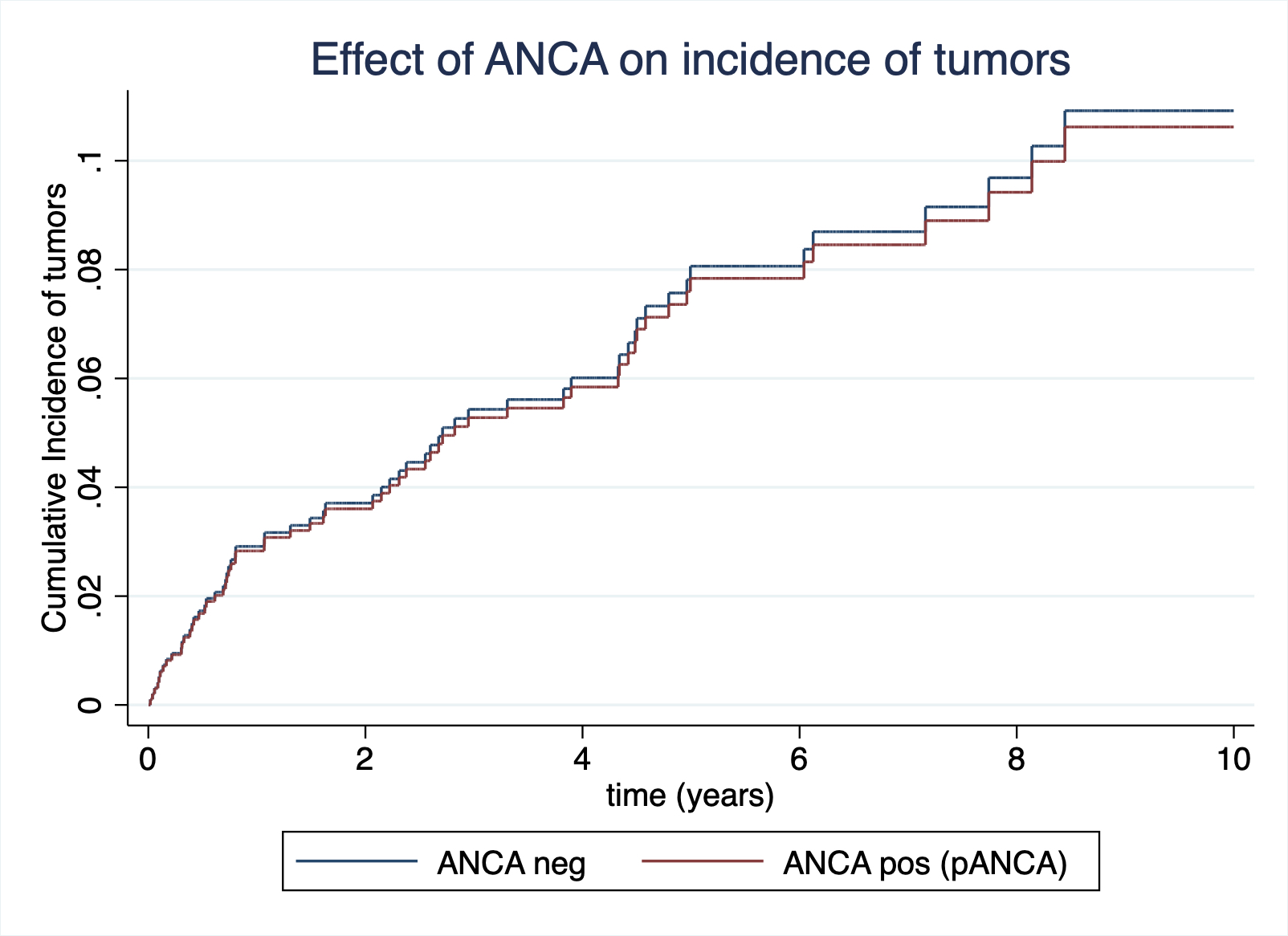 The estimated cumulative incidence curves for negative ANCA and pANCA patients, adjusted for sex, age and time of blood draw (Competing-risks regression model; Fine and Gray)
The estimated cumulative incidence curves for negative ANCA and pANCA patients, adjusted for sex, age and time of blood draw (Competing-risks regression model; Fine and Gray)
Disclosures: E. Brunetta, None; G. Ramponi, None; m. folci, None; M. De Santis, None; G. Guidelli, None; A. Ceribelli, None; N. Luciano, None; M. Caprioli, None; A. Sonaglia, None; C. Selmi, None.
Background/Purpose: Serum antineutrophil cytoplasmic antibodies (ANCA) are significantly associated with the development of ANCA-associated vasculitides (AAV) but may also be detected in patients with other rheumatologic conditions, chronic infections, among others. Patients with AAV are at higher risk for the onset of malignancies, likely related to the carcinogenic effects of treatment with cyclophosphamide. This has been confirmed by the lower incidence rate of cancer among these patients since when the mainstay of treatment shifted to rituximab. However, the association of ANCA positivity regardless of AAV or other disorders and the development of malignancies has been scarcely investigated.
We investigated the incidence of hematologic or solid cancer in 1,024 subjects with known ANCA status regardless of the indication for the test over 10 years. Our aim was to evaluate whether the presence of serum ANCA, notwithstanding the clinical phenotype, is associated with cancer incidence rate.
Methods: Our retrospective cohort study included 1,024 subjects who underwent ANCA testing at a single centre over 10 years. Time to event was defined as the time from ANCA test until the date of tumour diagnosis or censoring. We compared the incidence of cancer among the ANCA-positive (n=256, including 53 cANCA and 203 pANCA) and ANCA-negative (n=768) patients matched with propensity score (age, gender, time of blood draw), and we evaluated the competing-risks regression model (Fine and Gray) for the two groups.
Results: Out of 61 subjects who were diagnosed with cancer, 49 were ANCA-negative and 12 were ANCA-positive (pANCA positive). The most frequent tumors included hematological (20%) and lung (13%) cancers. Competing-risks regression was limited to ANCA-negative and pANCA-positive patients, due to the lack of cANCA patients with cancer. No relationship was found between pANCA status and incidence of cancer considering adjustment for sex, age and time of blood draw (HR 0.97; 95% CI 0.52-1.83). We were not able to adjust for smoking, drugs and number of comorbidities of each patient. After excluding patients with AAV (36 patients) from the competing-risks regression, results were unchanged (HR 1.00; 95% CI 0.52-1.92).
Conclusion: Serum ANCA positivity is not associated per se with an increased risk of malignancy. Our results further support the plausibility of the hypothesis according to which carcinogenicity in AAV reported in earlier studies was mainly related to the effects of immunosuppressive treatment, in particular with cyclophosphamide.
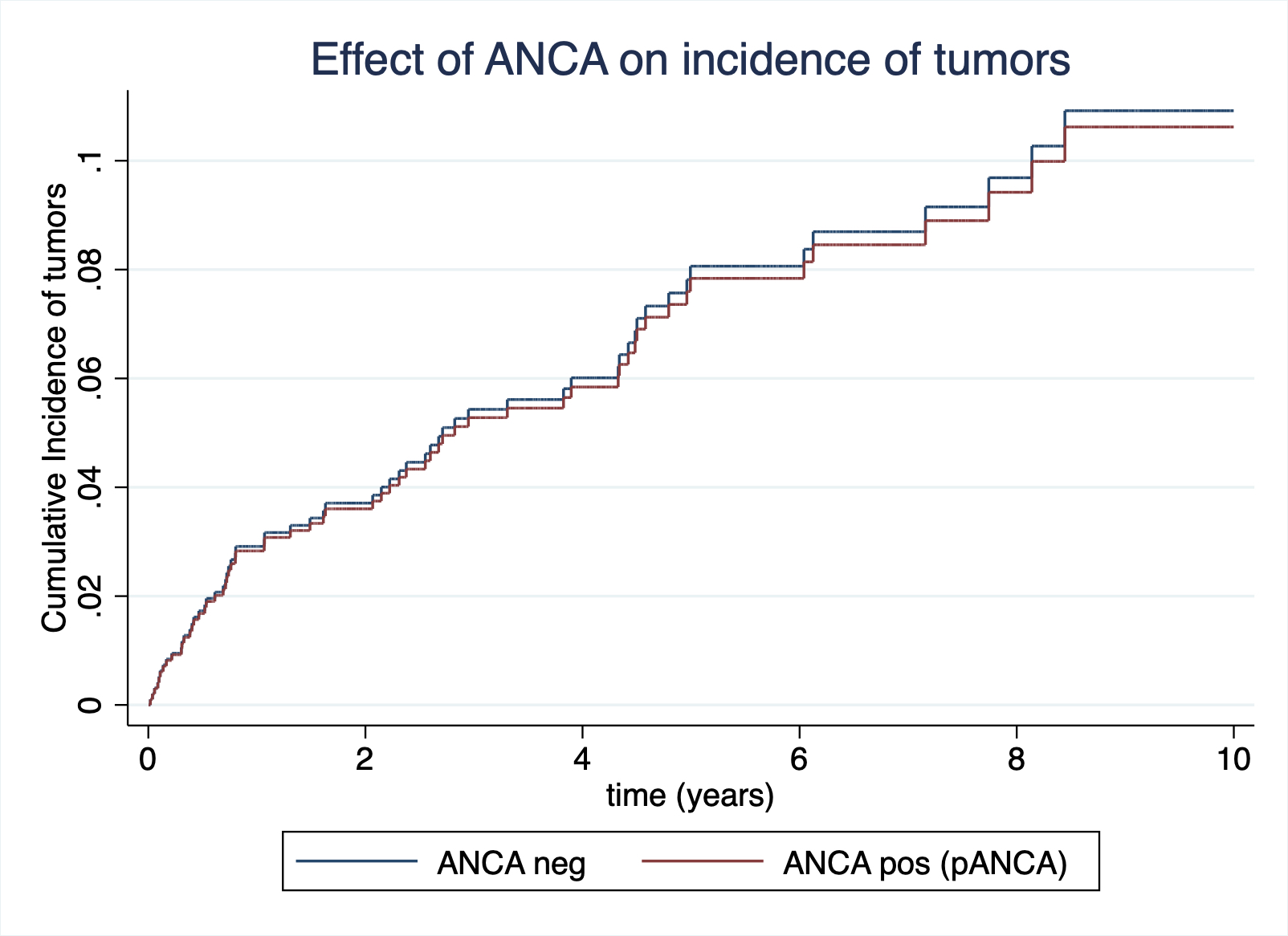 The estimated cumulative incidence curves for negative ANCA and pANCA patients, adjusted for sex, age and time of blood draw (Competing-risks regression model; Fine and Gray)
The estimated cumulative incidence curves for negative ANCA and pANCA patients, adjusted for sex, age and time of blood draw (Competing-risks regression model; Fine and Gray)Disclosures: E. Brunetta, None; G. Ramponi, None; m. folci, None; M. De Santis, None; G. Guidelli, None; A. Ceribelli, None; N. Luciano, None; M. Caprioli, None; A. Sonaglia, None; C. Selmi, None.

