Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0384: Inflammation Is Associated with Incident Hypertension in Patients with Axial Spondyloarthritis: A Longitudinal Cohort Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JS
Jenny Lin Hong Shi, PhD
The Chinese University of Hong Kong
Hong Kong, Hong Kong, China
Abstract Poster Presenter(s)
Jenny Lin Hong Shi1, Steven H Lam2, Ho So3, Edmund Li1, Tena Li1, Cheuk Chun Szeto1 and Lai-shan Tam1, 1The Chinese University of Hong Kong, Hong Kong, China, 2The Chinese university of Hong Kong, Hong Kong, Hong Kong, 3The Faculty of Medicine, CUHK, Hong Kong, Hong Kong
Background/Purpose: In the general population, hypertension (HT) is reported as one of the most important risk and modifiable factors to develop CVD. It is well recognized that inflammatory rheumatic diseases had increased risk of cardiovascular disease (CVD) burden. But limited studies exploring the relationship between axial spondyloarthritis (axSpA) and hypertension (HT) were reported.
Methods: This is a retrospective cohort study performed in axSpA patients who were recruited from 2001-2019 in the rheumatology clinic of PWH. Patients with established HT diagnosis and/or anti-hypertensives at baseline were excluded. They were followed from 2001 to 2020, till the occurrence of first diagnosis of IHT or end of study or the loss of follow-up. Baseline clinical and demographic data, drug history and traditional CV risk factors were compared between groups with and without IHT. Baseline and time-varying Cox regression analyses adjusting for age, sex, and BMI, were used to assess the relationship between drug history, inflammatory burden and IHT.
Results: 413 patients [34(25-43) years, male: 319 (77.2%)] were recruited. After a median follow up of 12 (6-17) years, 58 patients (14%) developed IHT (IHT+group). At baseline, in the multivariable Cox regression model, only baseline disease duration was an independent predictor for IHT. In the time-varying univariable Cox regression, increased ESR level and high inflammatory state (ESR≧20) over time were significant predictors for the development of IHT. Regarding drug use, paracetamol as well as use of csDMARDs, especially sulfasalazine were significantly associated with a higher risk of developing IHT (p< 0.001). While in multivariate analysis, baseline disease duration remained as the only significant predictor to increase risk of future IHT. ESR as an inflammatory marker had only borderline statistical significance in predicting the development of IHT, while ESR³20, the use of csDMARDs or sulfasalazine or paracetamol were no longer statistically significant.
Conclusion: Higher inflammatory burden as reflected by a longer baseline disease duration was a predictor associated with IHT after adjusting for traditional CV risk factors. Higher ESR level may also play a role in the development of IHT in these patients.
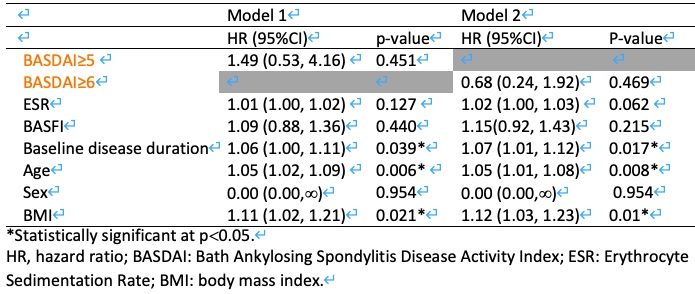 Table 1. Multivariable analysis with Cox proportional hazard regression for baseline predictors of IHT.
Table 1. Multivariable analysis with Cox proportional hazard regression for baseline predictors of IHT.
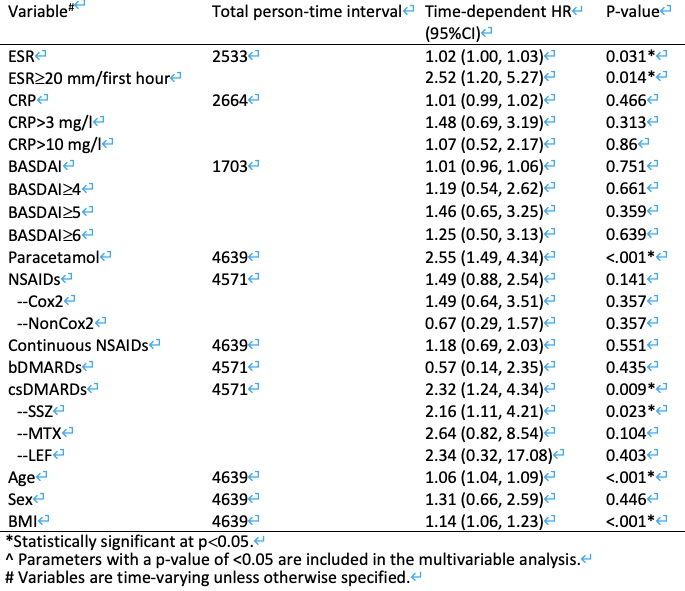 Table 2. Univariable analysis with time-dependent Cox proportional hazard regression for the predictors of incident hypertension (IHT).
Table 2. Univariable analysis with time-dependent Cox proportional hazard regression for the predictors of incident hypertension (IHT).
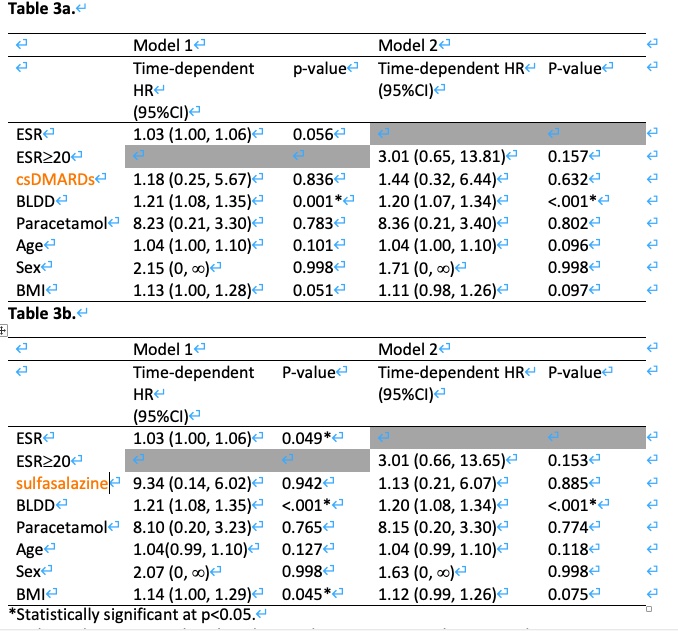 Table 3. Multivariable analysis with time-dependent Cox proportional hazard regression for the predictors of IHT.
Table 3. Multivariable analysis with time-dependent Cox proportional hazard regression for the predictors of IHT.
Disclosures: J. Shi, None; S. Lam, None; H. So, None; E. Li, None; T. Li, None; C. Szeto, None; L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca.
Background/Purpose: In the general population, hypertension (HT) is reported as one of the most important risk and modifiable factors to develop CVD. It is well recognized that inflammatory rheumatic diseases had increased risk of cardiovascular disease (CVD) burden. But limited studies exploring the relationship between axial spondyloarthritis (axSpA) and hypertension (HT) were reported.
Methods: This is a retrospective cohort study performed in axSpA patients who were recruited from 2001-2019 in the rheumatology clinic of PWH. Patients with established HT diagnosis and/or anti-hypertensives at baseline were excluded. They were followed from 2001 to 2020, till the occurrence of first diagnosis of IHT or end of study or the loss of follow-up. Baseline clinical and demographic data, drug history and traditional CV risk factors were compared between groups with and without IHT. Baseline and time-varying Cox regression analyses adjusting for age, sex, and BMI, were used to assess the relationship between drug history, inflammatory burden and IHT.
Results: 413 patients [34(25-43) years, male: 319 (77.2%)] were recruited. After a median follow up of 12 (6-17) years, 58 patients (14%) developed IHT (IHT+group). At baseline, in the multivariable Cox regression model, only baseline disease duration was an independent predictor for IHT. In the time-varying univariable Cox regression, increased ESR level and high inflammatory state (ESR≧20) over time were significant predictors for the development of IHT. Regarding drug use, paracetamol as well as use of csDMARDs, especially sulfasalazine were significantly associated with a higher risk of developing IHT (p< 0.001). While in multivariate analysis, baseline disease duration remained as the only significant predictor to increase risk of future IHT. ESR as an inflammatory marker had only borderline statistical significance in predicting the development of IHT, while ESR³20, the use of csDMARDs or sulfasalazine or paracetamol were no longer statistically significant.
Conclusion: Higher inflammatory burden as reflected by a longer baseline disease duration was a predictor associated with IHT after adjusting for traditional CV risk factors. Higher ESR level may also play a role in the development of IHT in these patients.
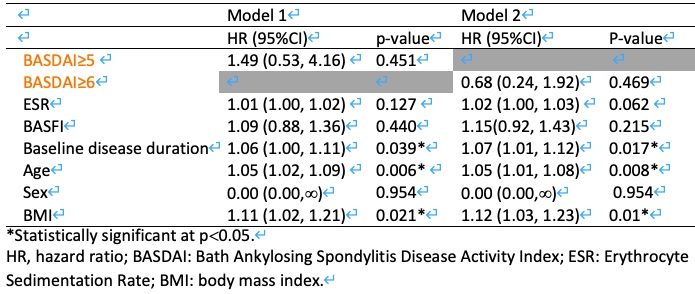 Table 1. Multivariable analysis with Cox proportional hazard regression for baseline predictors of IHT.
Table 1. Multivariable analysis with Cox proportional hazard regression for baseline predictors of IHT.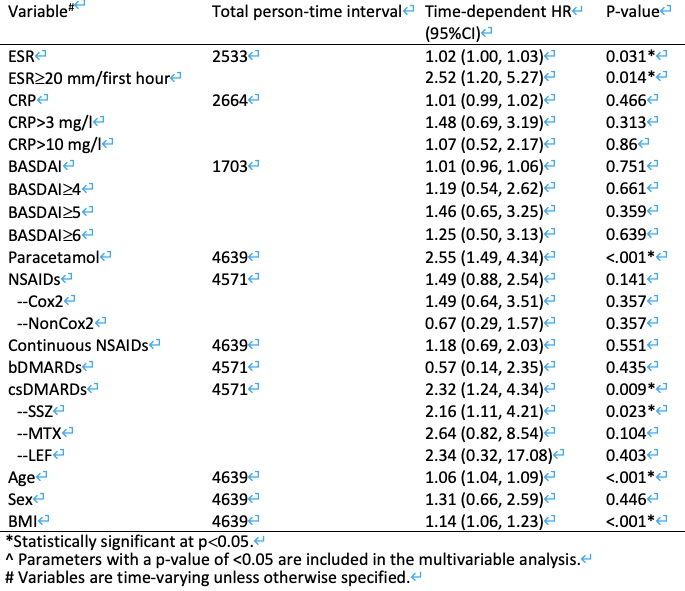 Table 2. Univariable analysis with time-dependent Cox proportional hazard regression for the predictors of incident hypertension (IHT).
Table 2. Univariable analysis with time-dependent Cox proportional hazard regression for the predictors of incident hypertension (IHT).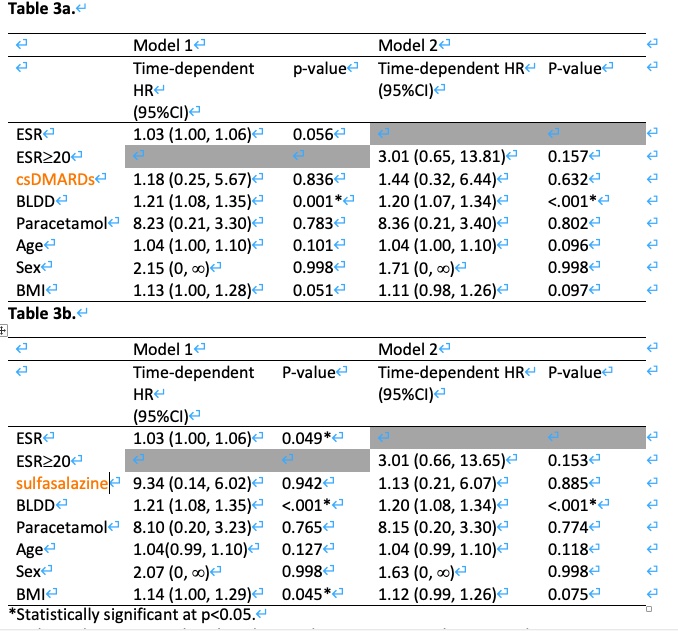 Table 3. Multivariable analysis with time-dependent Cox proportional hazard regression for the predictors of IHT.
Table 3. Multivariable analysis with time-dependent Cox proportional hazard regression for the predictors of IHT.Disclosures: J. Shi, None; S. Lam, None; H. So, None; E. Li, None; T. Li, None; C. Szeto, None; L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca.

