Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0476: Permanent Vision Loss in Giant Cell Arteritis: Why the Incidence Remains High
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- TD
Thomas Daikeler, MD
university hospital
Basel, Switzerland
Abstract Poster Presenter(s)
Andrea Hemmig1, Markus Aschwanden2, Sabine Seiler1, Christoph Berger3, Philipp Köhn1, Noemi Mensch1, Daniel Staub2, Mihaela Stegert1, Stephan Imfeld2 and Thomas Daikeler1, 1Department of Rheumatology, University Hospital Basel, Basel, Switzerland, 2Department of Angiology, University Hospital Basel, Basel, Switzerland, 3Departments of Dermatology, Rheumatology and Internal Medicine, University Center for Immunology, University Hospital Basel, Basel, Switzerland
Background/Purpose: Permanent vision loss (PVL) remains the most feared complication of giant cell arteritis (GCA). In recent years, fast track clinic approaches for early GCA diagnosis have been described to reduce the incidence of PVL (1). We aim to examine patient and referral characteristics and trends in the incidence of PVL over the past 15 years.
Methods: Retrospective analysis of a longitudinal cohort of patients with suspected GCA treated at the University Hospital Basel between December 2006 and May 2021. We analyzed demographic data, symptoms, laboratory and imaging findings, and treatment. Time from first symptom to vision loss, to first physician contact and to steroid initiation was assessed. Only patients who were followed for at least 6 months after GCA diagnosis were included. PVL was defined as persisting complete or partial vision loss in at least one eye.
Results: The cohort includes 740 patients with suspicion of GCA. Of those, 311 patients were newly diagnosed with GCA. 282 (mean age 72.9 ± 8.3 years, 64% females) fulfilled inclusion criteria. Among these, 47 patients (17%) developed PVL. In 43 (91%) patients, PVL manifested at GCA diagnosis whereas in 4 (9%) patients, PVL developed more than one month after diagnosis (median time from GCA diagnosis to first visual symptom 59.5 days (IQR 42.3-90.5 days)). AION was the most common cause of PVL (Table 1). Characteristics of patients with and without PVL are similar to previous reports (Table 2). Patients with PVL were older, had more frequent hypertension, diabetes, and jaw claudication. Polymyalgia symptoms at diagnosis were less frequent among PVL patients. The incidence of PVL over 15 years remained constant (Figure 1).
Of the patients who developed PVL, the majority sought first medical contact because of new-onset visual symptoms (n=40, 85%). However, 27 (57%) patients with PVL reported having other cranial or systemic symptoms before the onset of visual manifestations with a median time from first symptom until first contact with their general practitioners (GP) of 21.0 days (IQR 9.5-31 days). The median time from first GP contact until steroid initiation was 0.0 days (IQR 0-1 days) in all patients who developed PVL.
Conclusion: In most patients, PVL manifested at diagnosis and only few cases developed PVL while being under treatment. Known risk factors for arteriosclerosis are significantly associated with PVL in our cohort. Despite immediate initiation of steroid treatment after first GP contact, incidence of PVL at GCA diagnosis does not decline since 2006, because in most patients PVL manifests before the first contact with GPs. However, more than half of the patients with PVL reported GCA symptoms other than ocular, which occurred a median of 25.0 days before the onset of visual disturbances. Thus, earlier diagnosis and treatment is possible. Education of patients and public as well as training of GPs is needed to shorten the time from first GCA associated symptom to start of treatment and hence to reduce the frequency of PVL.
References:
1. Monti S, Bartoletti A, Bellis E, Delvino P, Montecucco C. Fast-Track Ultrasound Clinic for the Diagnosis of Giant Cell Arteritis Changes the Prognosis of the Disease but Not the Risk of Future Relapse. Front Med (Lausanne). 2020;7:589794.
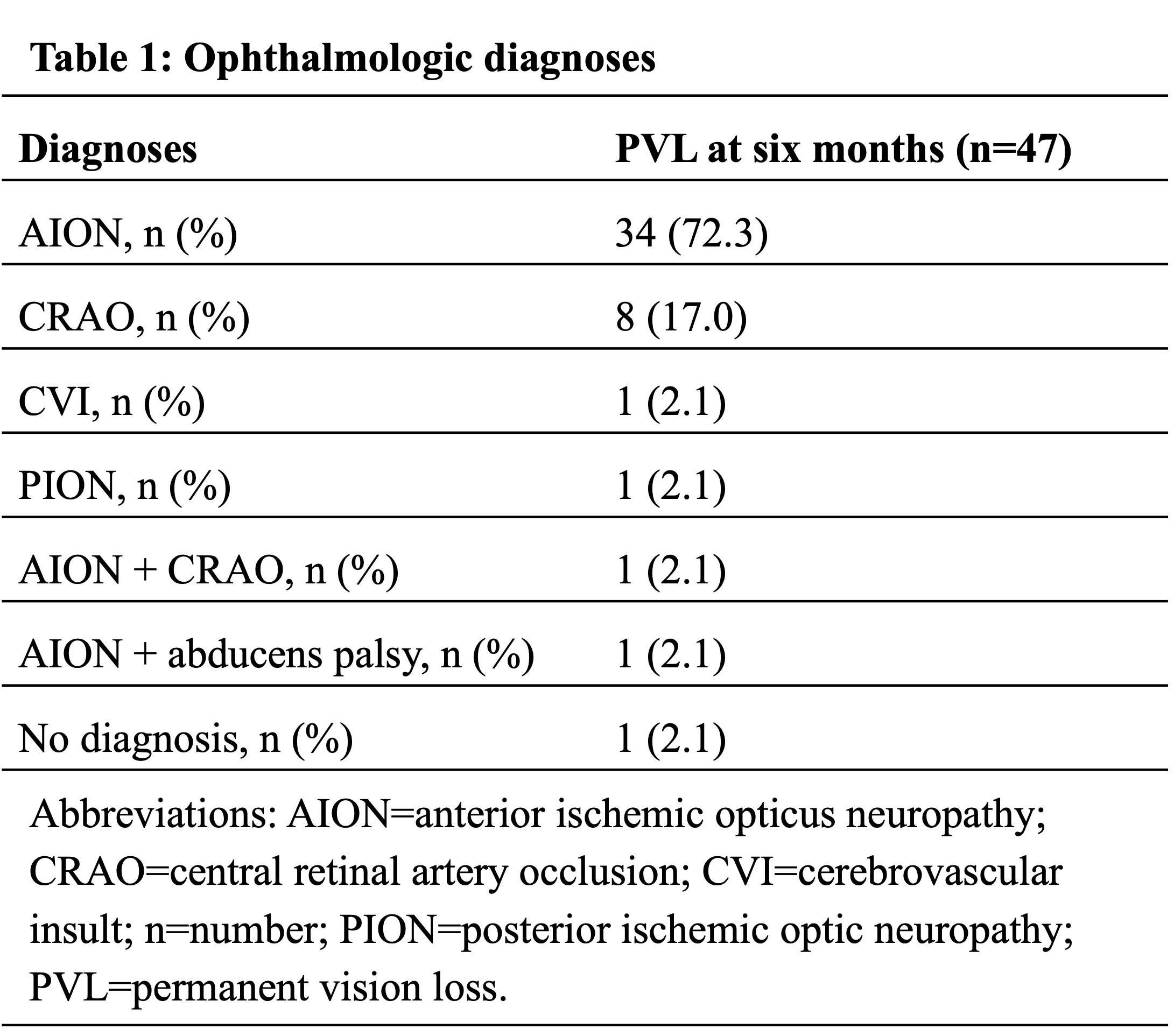
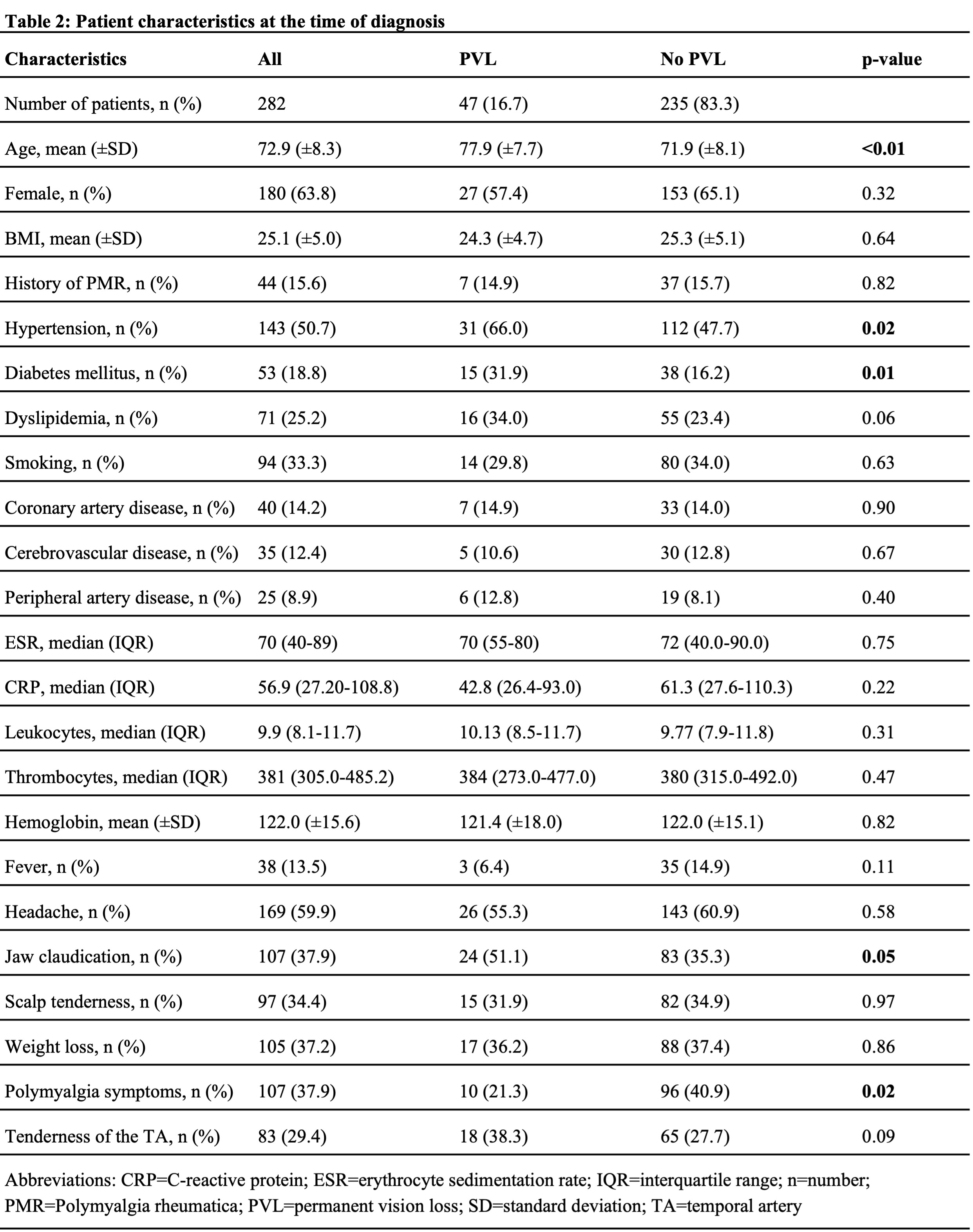
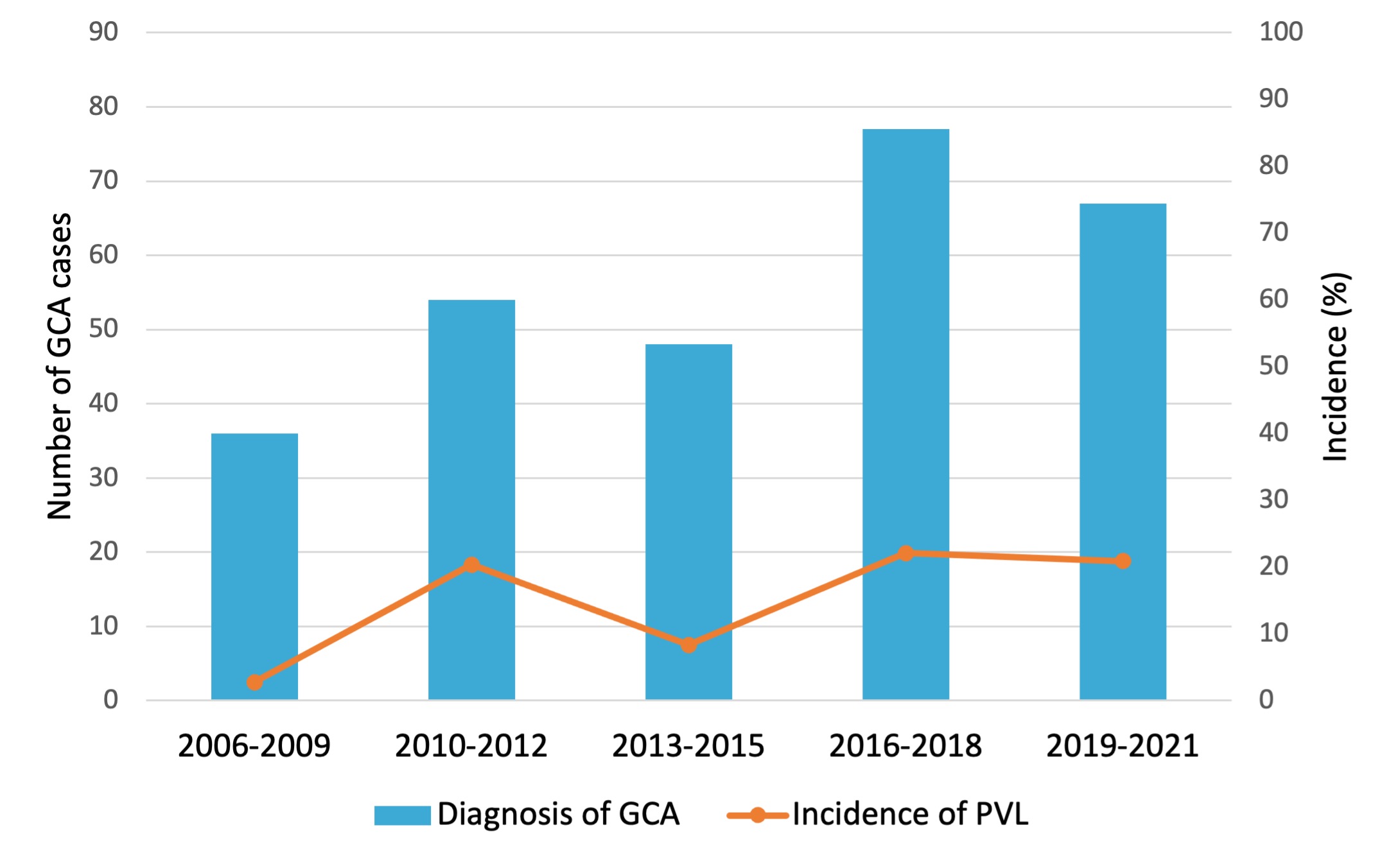 Figure 1: Incidence of PVL over the last 15 years.
Figure 1: Incidence of PVL over the last 15 years.
Disclosures: A. Hemmig, None; M. Aschwanden, None; S. Seiler, None; C. Berger, None; P. Köhn, None; N. Mensch, None; D. Staub, None; M. Stegert, None; S. Imfeld, None; T. Daikeler, None.
Background/Purpose: Permanent vision loss (PVL) remains the most feared complication of giant cell arteritis (GCA). In recent years, fast track clinic approaches for early GCA diagnosis have been described to reduce the incidence of PVL (1). We aim to examine patient and referral characteristics and trends in the incidence of PVL over the past 15 years.
Methods: Retrospective analysis of a longitudinal cohort of patients with suspected GCA treated at the University Hospital Basel between December 2006 and May 2021. We analyzed demographic data, symptoms, laboratory and imaging findings, and treatment. Time from first symptom to vision loss, to first physician contact and to steroid initiation was assessed. Only patients who were followed for at least 6 months after GCA diagnosis were included. PVL was defined as persisting complete or partial vision loss in at least one eye.
Results: The cohort includes 740 patients with suspicion of GCA. Of those, 311 patients were newly diagnosed with GCA. 282 (mean age 72.9 ± 8.3 years, 64% females) fulfilled inclusion criteria. Among these, 47 patients (17%) developed PVL. In 43 (91%) patients, PVL manifested at GCA diagnosis whereas in 4 (9%) patients, PVL developed more than one month after diagnosis (median time from GCA diagnosis to first visual symptom 59.5 days (IQR 42.3-90.5 days)). AION was the most common cause of PVL (Table 1). Characteristics of patients with and without PVL are similar to previous reports (Table 2). Patients with PVL were older, had more frequent hypertension, diabetes, and jaw claudication. Polymyalgia symptoms at diagnosis were less frequent among PVL patients. The incidence of PVL over 15 years remained constant (Figure 1).
Of the patients who developed PVL, the majority sought first medical contact because of new-onset visual symptoms (n=40, 85%). However, 27 (57%) patients with PVL reported having other cranial or systemic symptoms before the onset of visual manifestations with a median time from first symptom until first contact with their general practitioners (GP) of 21.0 days (IQR 9.5-31 days). The median time from first GP contact until steroid initiation was 0.0 days (IQR 0-1 days) in all patients who developed PVL.
Conclusion: In most patients, PVL manifested at diagnosis and only few cases developed PVL while being under treatment. Known risk factors for arteriosclerosis are significantly associated with PVL in our cohort. Despite immediate initiation of steroid treatment after first GP contact, incidence of PVL at GCA diagnosis does not decline since 2006, because in most patients PVL manifests before the first contact with GPs. However, more than half of the patients with PVL reported GCA symptoms other than ocular, which occurred a median of 25.0 days before the onset of visual disturbances. Thus, earlier diagnosis and treatment is possible. Education of patients and public as well as training of GPs is needed to shorten the time from first GCA associated symptom to start of treatment and hence to reduce the frequency of PVL.
References:
1. Monti S, Bartoletti A, Bellis E, Delvino P, Montecucco C. Fast-Track Ultrasound Clinic for the Diagnosis of Giant Cell Arteritis Changes the Prognosis of the Disease but Not the Risk of Future Relapse. Front Med (Lausanne). 2020;7:589794.
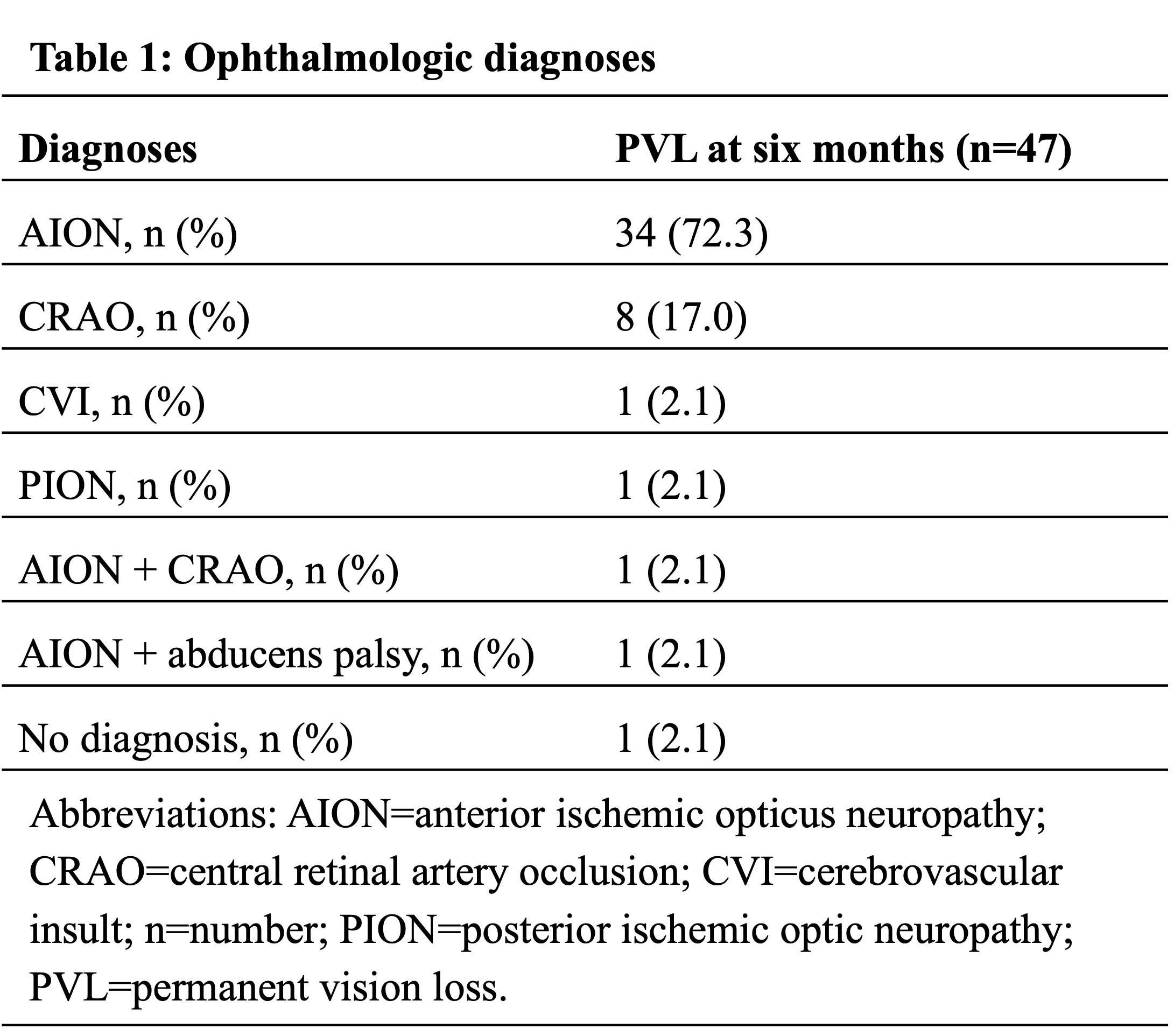
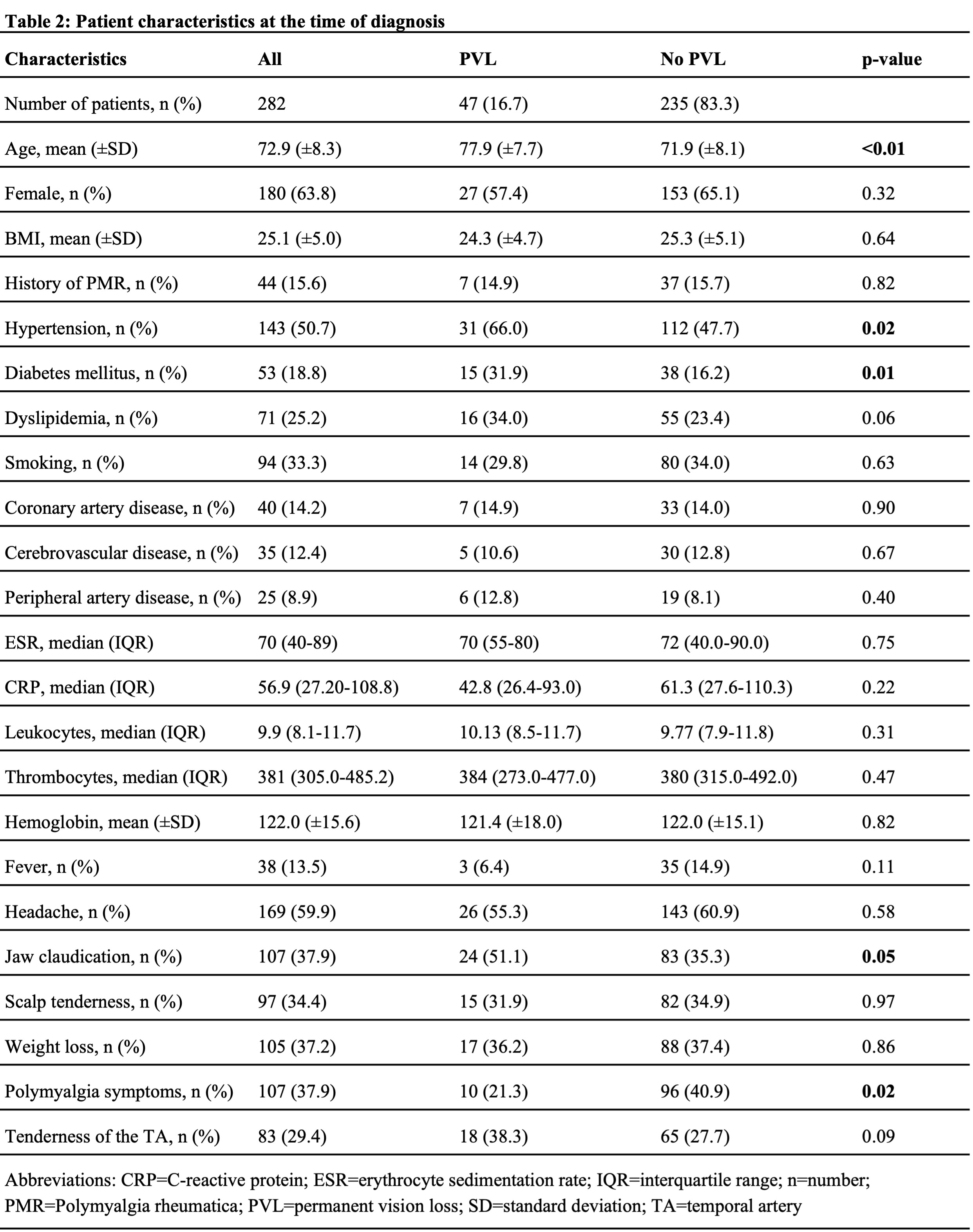
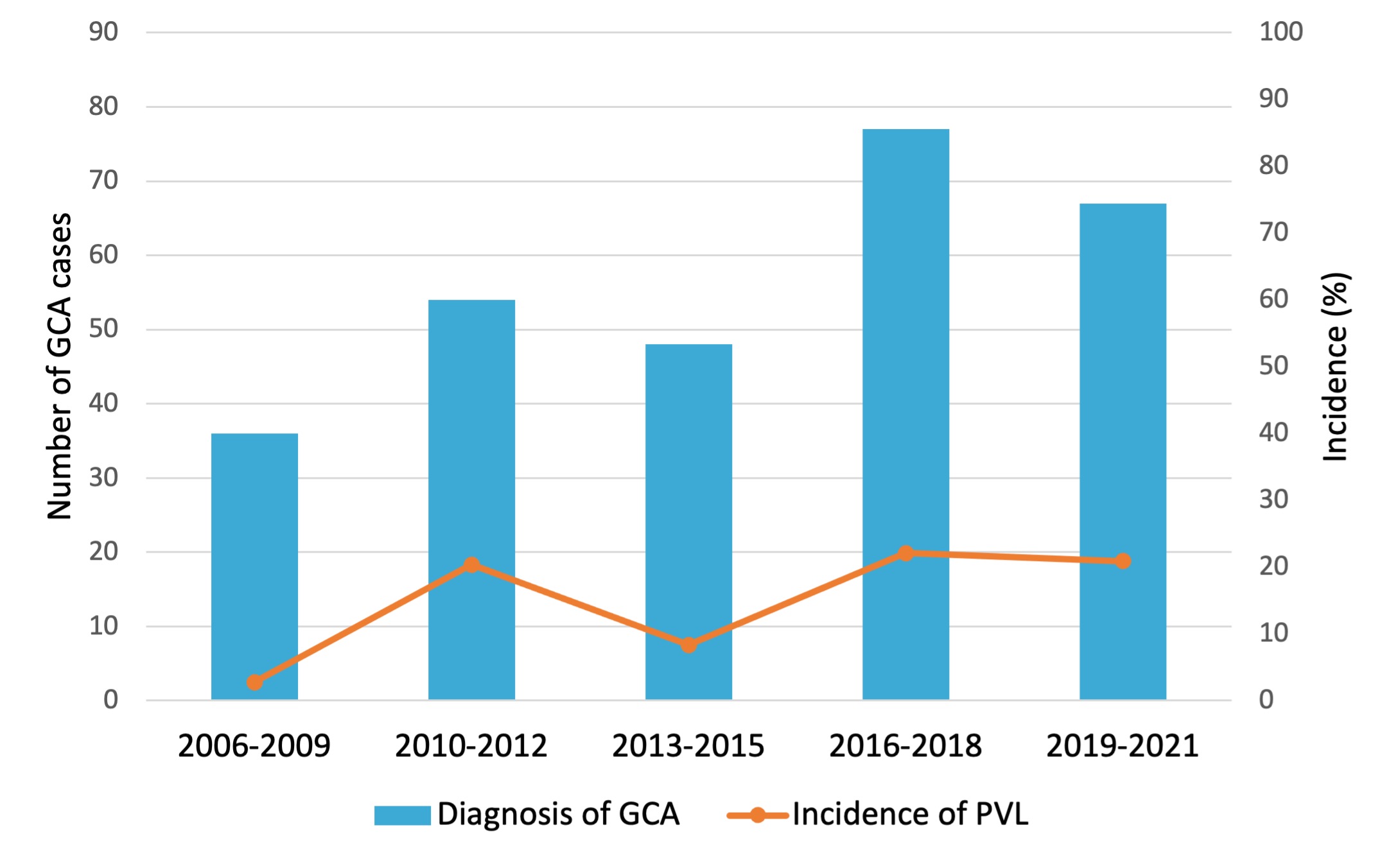 Figure 1: Incidence of PVL over the last 15 years.
Figure 1: Incidence of PVL over the last 15 years.Disclosures: A. Hemmig, None; M. Aschwanden, None; S. Seiler, None; C. Berger, None; P. Köhn, None; N. Mensch, None; D. Staub, None; M. Stegert, None; S. Imfeld, None; T. Daikeler, None.

