Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0390: Persistent Post-Covid Symptoms in Psoriatic Arthritis Patients
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SP
Sonia Pastor Navarro, MD
Hospital Universitario de Salamanca
Salamanca, Spain
Abstract Poster Presenter(s)
Sonia Pastor Navarro1, Marta Ibáñez Martínez1, Olga Compán Fernández1, Belén Miguel Ibáñez1, Olga Martínez González1, Cristina Hidalgo Calleja1, Ana Isabel Turrión Nieves1, Susana Gómez Castro2 and Carlos Montilla Morales1, 1Hospital Universitario de Salamanca, Salamanca, Spain, 2Hospital Universitario Salamanca, Salamanca, Spain
Background/Purpose: Symptomatic onset long after recovery from the acute phase of COVID-19 infection has been reported by the population. Currently, it is not known how certain "Long Covid" symptoms affect a population of patients with psoriatic arthritis (PsA).
The objective is to assess the affectation of the "Long Covid Syndrome" in the clinical and emotional condition of a group of patients with PsA.
Methods: A prospective observational study of thirty-two patients diagnosed with PsA by the CASPAR criteria has been carried out. All those who had constituted a "confirmed case" of COVID-19 were selected following the Raveendran criteria.
Fatigue was assessed in this group of patients using the FACIT-F (Functional Assessment of Chronic Illness Therapy- Fatigue) self-administered questionnaire. The existence of anxiety or depression was obtained with the HADS-A (Hospital Anxiety and Depression Scale- anxiety) and HADS-D (Hospital Anxiety and Depression Scale- depression) questionnaires. Sleep quality disturbance was examined using the ISI (Insomnia Severity Index) questionnaire. All questionnaires were applied simultaneously in person or electronically in two different occasions to each of the individuals, one before contagion and another four weeks after the COVID-19 infection had been resolved.
Results: Patients were predominantly male with a mean age of 53 years and PsA disease duration of 13.2 years, with a standard deviation (SD) of 9 and 13.2 years respectively. PsA patients had a mean fatigue score of 35.21 (SD 11.43). The average of fatigue in that same group before suffering from COVID-19 was 39.56 (SD 10.57) (p=0.001). No relationship was found in the correlation of fatigue with the rest of the parameters. 18.75% of patients showed initial anxiety and 6.25% depression. The same group of patients after COVID-19 showed rates of anxiety and depression of 43.75% and 14.29%, respectively. 12.5% of patients with PsA had insomnia prior to COVID-19, which caused a 43.75% increase in sleep disturbances in the same study group (Table 1).
Regarding the relation between changes in fatigue, anxiety, depression and sleep quality and baseline characteristics, an increase in anxiety and a worsening in sleep quality were observed after COVID-19, which were related to baseline anxiety and baseline sleep quality respectively. No differences were found in the other parameters. No differences were found between increased fatigue and baseline variables (Table 2).
Finally, no significant differences were found between changes in fatigue, anxiety, depression and sleep quality and COVID-19 clinical characteristics.
Conclusion: COVID-19 influences fatigue, sleep, anxiety and depression. Except for anxiety and sleep quality, this increase is not due to presence of previous features or the characteristics of COVID-19 infection.
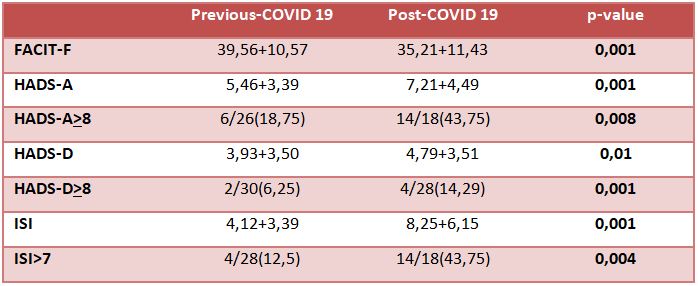 Table 1: Differences between fatigue, anxiety, depression and sleep before and after COVID-19 disease.
Table 1: Differences between fatigue, anxiety, depression and sleep before and after COVID-19 disease.
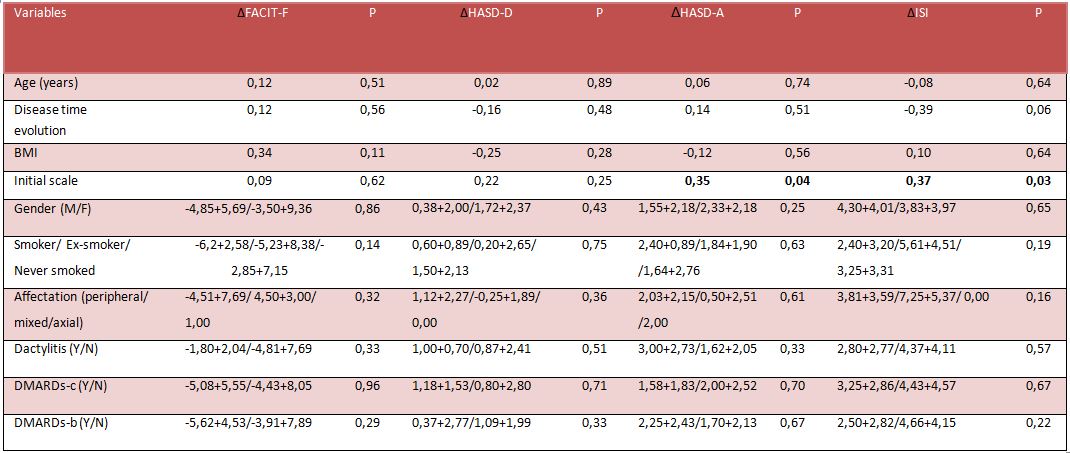 Table 2: Correlation between baseline characteristics and different scales.
Table 2: Correlation between baseline characteristics and different scales.
*p: p-value, BMI: body mass index, M/F: male/female, Y/N: yes/no, DMARDs-c: conventional disease-modifying antirheumatic drug, DMARDs-b: biological disease-modifying antirheumatic drug.
Disclosures: S. Pastor Navarro, None; M. Ibáñez Martínez, None; O. Compán Fernández, None; B. Miguel Ibáñez, None; O. Martínez González, None; C. Hidalgo Calleja, None; A. Turrión Nieves, None; S. Gómez Castro, None; C. Montilla Morales, None.
Background/Purpose: Symptomatic onset long after recovery from the acute phase of COVID-19 infection has been reported by the population. Currently, it is not known how certain "Long Covid" symptoms affect a population of patients with psoriatic arthritis (PsA).
The objective is to assess the affectation of the "Long Covid Syndrome" in the clinical and emotional condition of a group of patients with PsA.
Methods: A prospective observational study of thirty-two patients diagnosed with PsA by the CASPAR criteria has been carried out. All those who had constituted a "confirmed case" of COVID-19 were selected following the Raveendran criteria.
Fatigue was assessed in this group of patients using the FACIT-F (Functional Assessment of Chronic Illness Therapy- Fatigue) self-administered questionnaire. The existence of anxiety or depression was obtained with the HADS-A (Hospital Anxiety and Depression Scale- anxiety) and HADS-D (Hospital Anxiety and Depression Scale- depression) questionnaires. Sleep quality disturbance was examined using the ISI (Insomnia Severity Index) questionnaire. All questionnaires were applied simultaneously in person or electronically in two different occasions to each of the individuals, one before contagion and another four weeks after the COVID-19 infection had been resolved.
Results: Patients were predominantly male with a mean age of 53 years and PsA disease duration of 13.2 years, with a standard deviation (SD) of 9 and 13.2 years respectively. PsA patients had a mean fatigue score of 35.21 (SD 11.43). The average of fatigue in that same group before suffering from COVID-19 was 39.56 (SD 10.57) (p=0.001). No relationship was found in the correlation of fatigue with the rest of the parameters. 18.75% of patients showed initial anxiety and 6.25% depression. The same group of patients after COVID-19 showed rates of anxiety and depression of 43.75% and 14.29%, respectively. 12.5% of patients with PsA had insomnia prior to COVID-19, which caused a 43.75% increase in sleep disturbances in the same study group (Table 1).
Regarding the relation between changes in fatigue, anxiety, depression and sleep quality and baseline characteristics, an increase in anxiety and a worsening in sleep quality were observed after COVID-19, which were related to baseline anxiety and baseline sleep quality respectively. No differences were found in the other parameters. No differences were found between increased fatigue and baseline variables (Table 2).
Finally, no significant differences were found between changes in fatigue, anxiety, depression and sleep quality and COVID-19 clinical characteristics.
Conclusion: COVID-19 influences fatigue, sleep, anxiety and depression. Except for anxiety and sleep quality, this increase is not due to presence of previous features or the characteristics of COVID-19 infection.
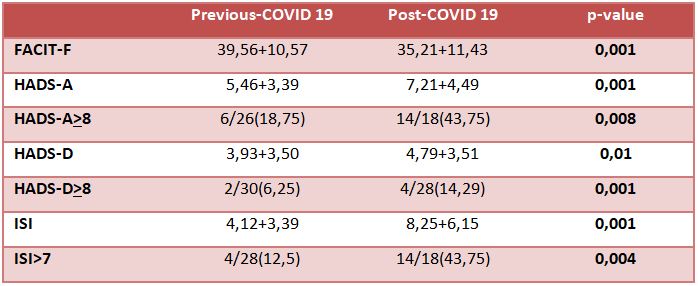 Table 1: Differences between fatigue, anxiety, depression and sleep before and after COVID-19 disease.
Table 1: Differences between fatigue, anxiety, depression and sleep before and after COVID-19 disease.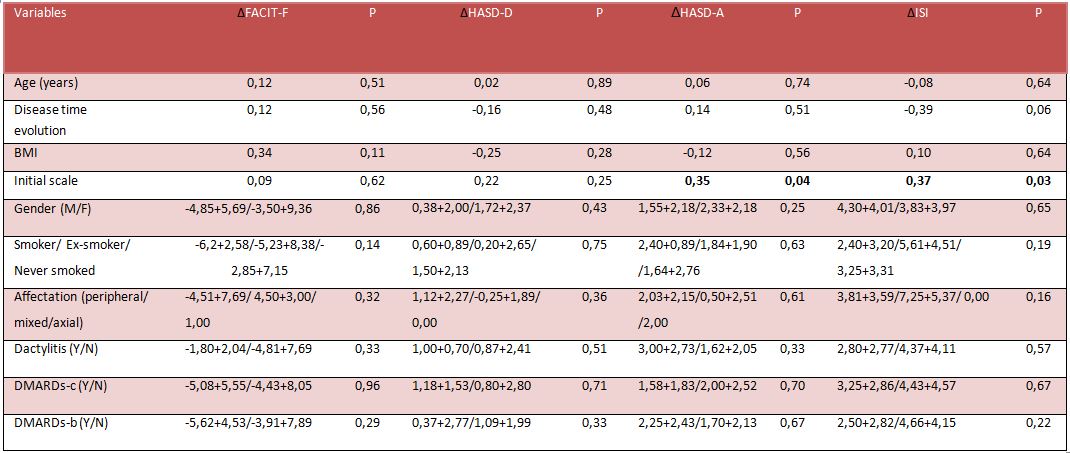 Table 2: Correlation between baseline characteristics and different scales.
Table 2: Correlation between baseline characteristics and different scales.*p: p-value, BMI: body mass index, M/F: male/female, Y/N: yes/no, DMARDs-c: conventional disease-modifying antirheumatic drug, DMARDs-b: biological disease-modifying antirheumatic drug.
Disclosures: S. Pastor Navarro, None; M. Ibáñez Martínez, None; O. Compán Fernández, None; B. Miguel Ibáñez, None; O. Martínez González, None; C. Hidalgo Calleja, None; A. Turrión Nieves, None; S. Gómez Castro, None; C. Montilla Morales, None.

