Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0241–0271) RA – Diagnosis, Manifestations, and Outcomes Poster I
0262: Predictors of Fragility Fracture Amongst Patients with Rheumatoid Arthritis: An Observational Cohort Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MB
Marwan Bukhari, PhD, FRCP
Rheumatology (Oxford)
Lancaster, United Kingdom
Abstract Poster Presenter(s)
Seema Sharma1 and Marwan Bukhari2, 1Lancaster Royal Infirmary, Lancaster, United Kingdom, 2University Hospitals of Morecambe Bay NHS Trust, Lancaster, United Kingdom
Background/Purpose: Rheumatoid arthritis (RA) is associated with reduced bone mineral density and almost one third of this population have osteoporosis leading to increased risk of fragility fracture. This mechanisms underlying this association are felt to be multifactorial and include the inflammatory disease process, medication burden and frailty. The fracture risk assessment tool (FRAX) is used in clinical practice to estimate risk of fragility fracture over a ten year period to guide therapy decisions. Using a large cohort of patients with RA, we aimed to establish which measure of bone mineral density (BMD) is most associated with risk of fracture in this population and the role of other traditional risk factors for fracture.
Methods: Patients presented between June 2004 and October 2016 to a district general hospital in North West England for estimation of bone mineral density (BMD) by dual energy X-ray absorptiometry (DEXA). Information was also collected on known risk factors for osteoporosis as defined by the FRAX tool. All analysis was performed on those with a history of rheumatoid arthritis and then further sub-analysis was performed by sex. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Univariate regression models were used to assess the risk of fracture using measures of BMD; namely measurements at the femoral neck, total hip and lumbar spine. Further univariate analysis was also performed using other known risk factors for osteoporosis (smoking status, alcohol use, history of parental hip fracture and steroid use). Using strongest BMD predictor of fracture, multivariate regression was performed using all known available risk factors. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Results: Out of 35,759 patients, 1527 had a diagnosis of RA. Cohort characteristics of these patients are summarised in table 1. Results of univariate analysis are shown in table 2 and results of multivariate analysis are shown in table 3.
Conclusion: BMD of left femoral neck was found to be most associated with fragility fracture in both men and women with RA. No other traditional risk factors aside from current alcohol use were found to be significantly associated with risk of fragility fracture. This may suggest that in patients with RA, traditional risk factors may not perform as well in predicting fracture.
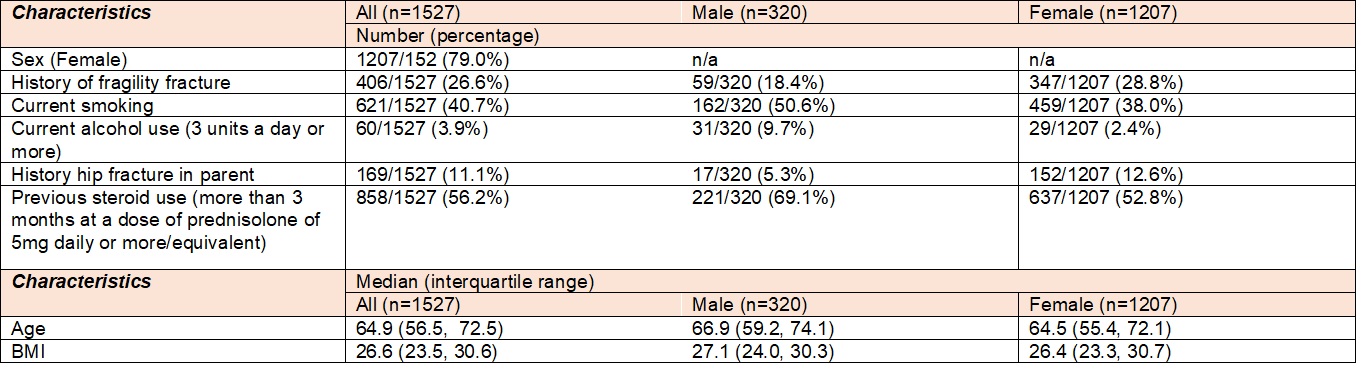 Table 1: Cohort Characteristics
Table 1: Cohort Characteristics
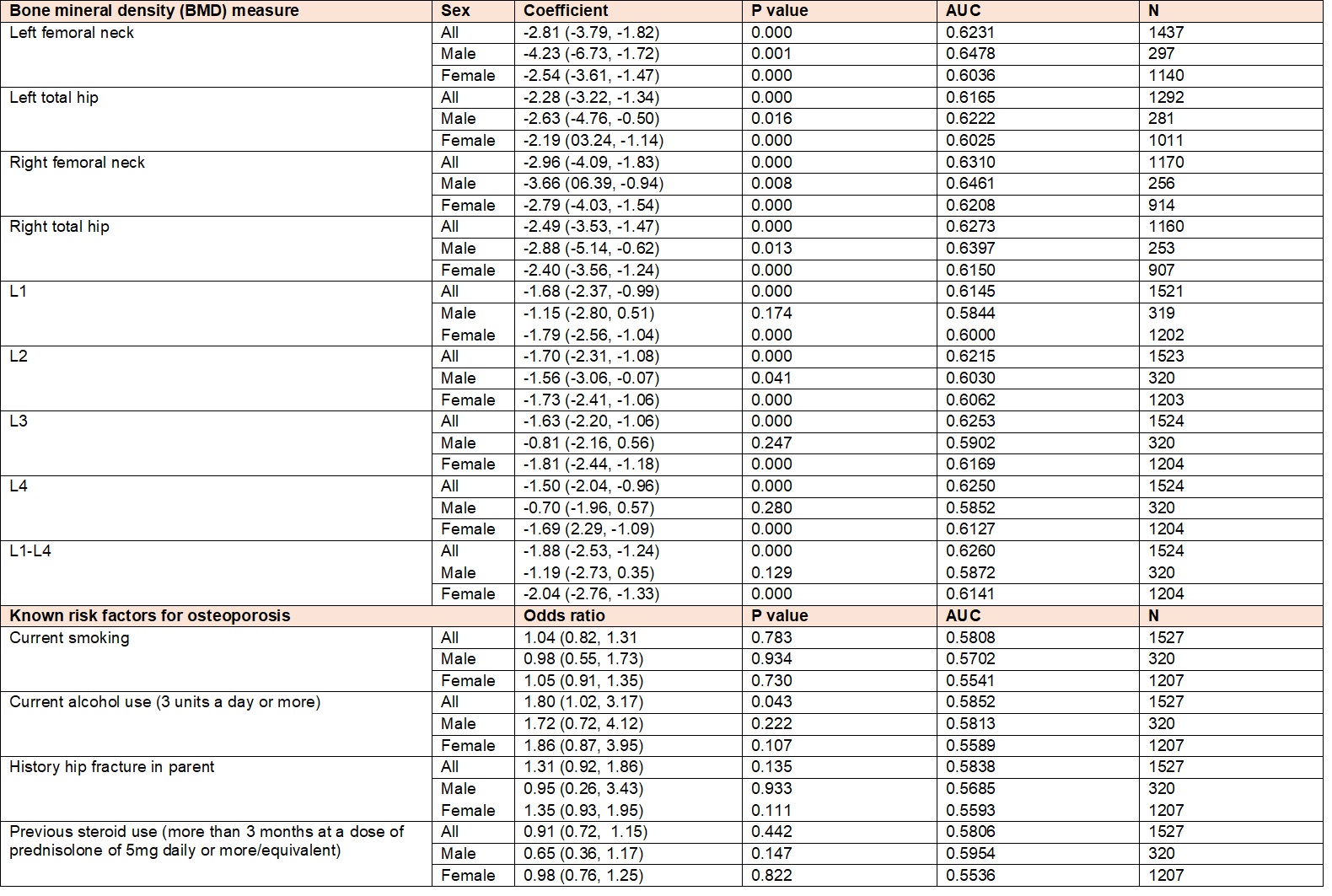 Table 2: Univariate analysis. : All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Table 2: Univariate analysis. : All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
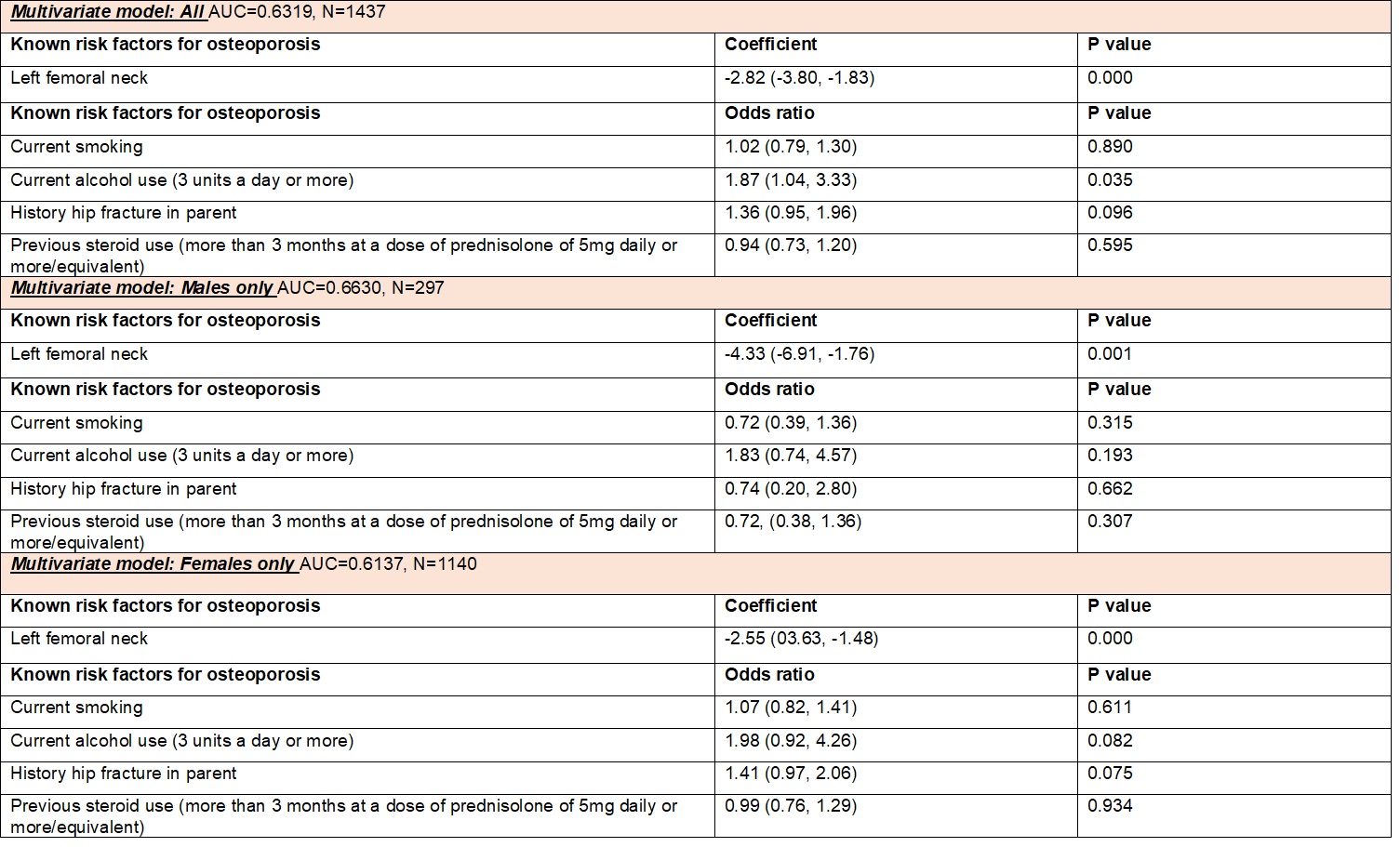 Table 3: Multivariate analysis: BMD of left femoral neck identified as most associated with fracture and used in combination with all available risk factors in 3 multivariate models. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measure, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Table 3: Multivariate analysis: BMD of left femoral neck identified as most associated with fracture and used in combination with all available risk factors in 3 multivariate models. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measure, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Disclosures: S. Sharma, None; M. Bukhari, None.
Background/Purpose: Rheumatoid arthritis (RA) is associated with reduced bone mineral density and almost one third of this population have osteoporosis leading to increased risk of fragility fracture. This mechanisms underlying this association are felt to be multifactorial and include the inflammatory disease process, medication burden and frailty. The fracture risk assessment tool (FRAX) is used in clinical practice to estimate risk of fragility fracture over a ten year period to guide therapy decisions. Using a large cohort of patients with RA, we aimed to establish which measure of bone mineral density (BMD) is most associated with risk of fracture in this population and the role of other traditional risk factors for fracture.
Methods: Patients presented between June 2004 and October 2016 to a district general hospital in North West England for estimation of bone mineral density (BMD) by dual energy X-ray absorptiometry (DEXA). Information was also collected on known risk factors for osteoporosis as defined by the FRAX tool. All analysis was performed on those with a history of rheumatoid arthritis and then further sub-analysis was performed by sex. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Univariate regression models were used to assess the risk of fracture using measures of BMD; namely measurements at the femoral neck, total hip and lumbar spine. Further univariate analysis was also performed using other known risk factors for osteoporosis (smoking status, alcohol use, history of parental hip fracture and steroid use). Using strongest BMD predictor of fracture, multivariate regression was performed using all known available risk factors. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Results: Out of 35,759 patients, 1527 had a diagnosis of RA. Cohort characteristics of these patients are summarised in table 1. Results of univariate analysis are shown in table 2 and results of multivariate analysis are shown in table 3.
Conclusion: BMD of left femoral neck was found to be most associated with fragility fracture in both men and women with RA. No other traditional risk factors aside from current alcohol use were found to be significantly associated with risk of fragility fracture. This may suggest that in patients with RA, traditional risk factors may not perform as well in predicting fracture.
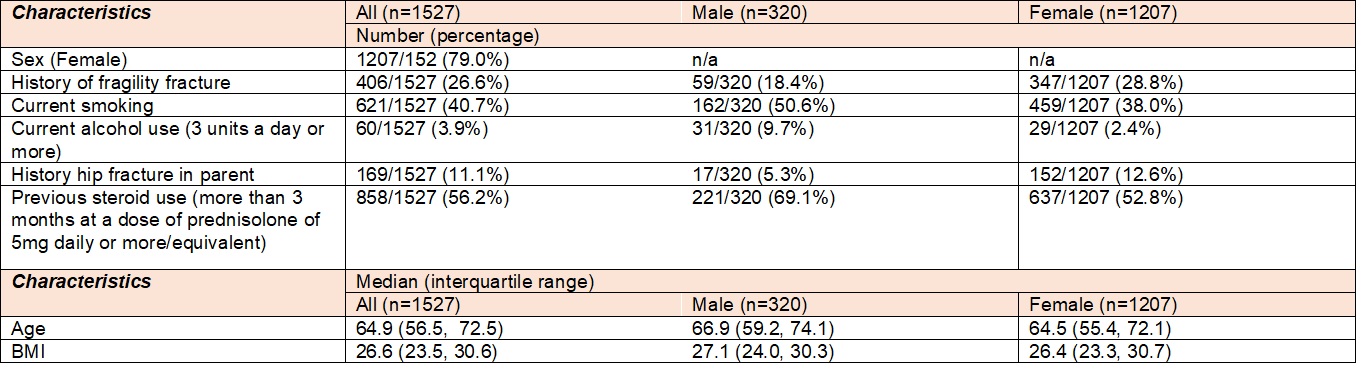 Table 1: Cohort Characteristics
Table 1: Cohort Characteristics 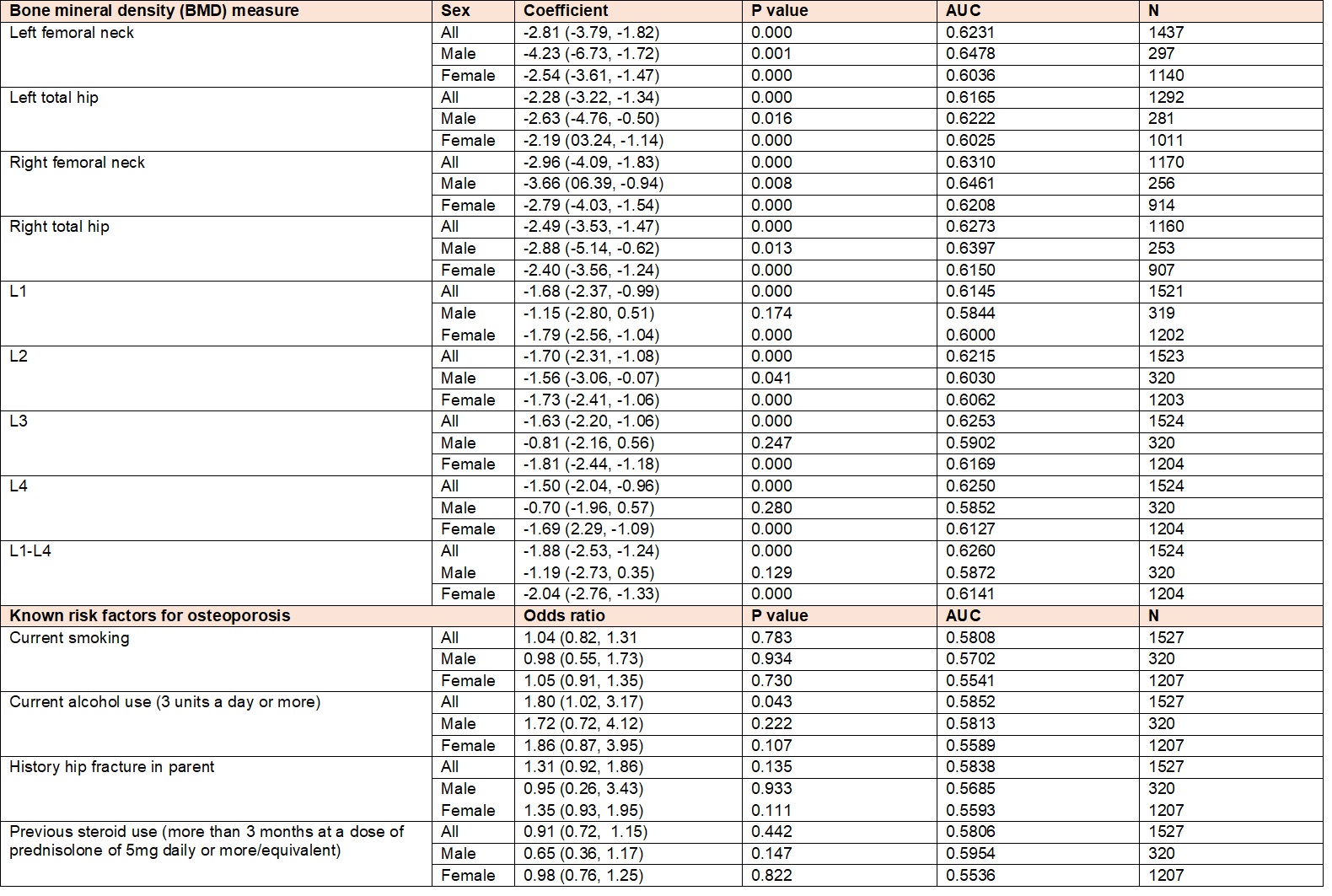 Table 2: Univariate analysis. : All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Table 2: Univariate analysis. : All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measures, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve. 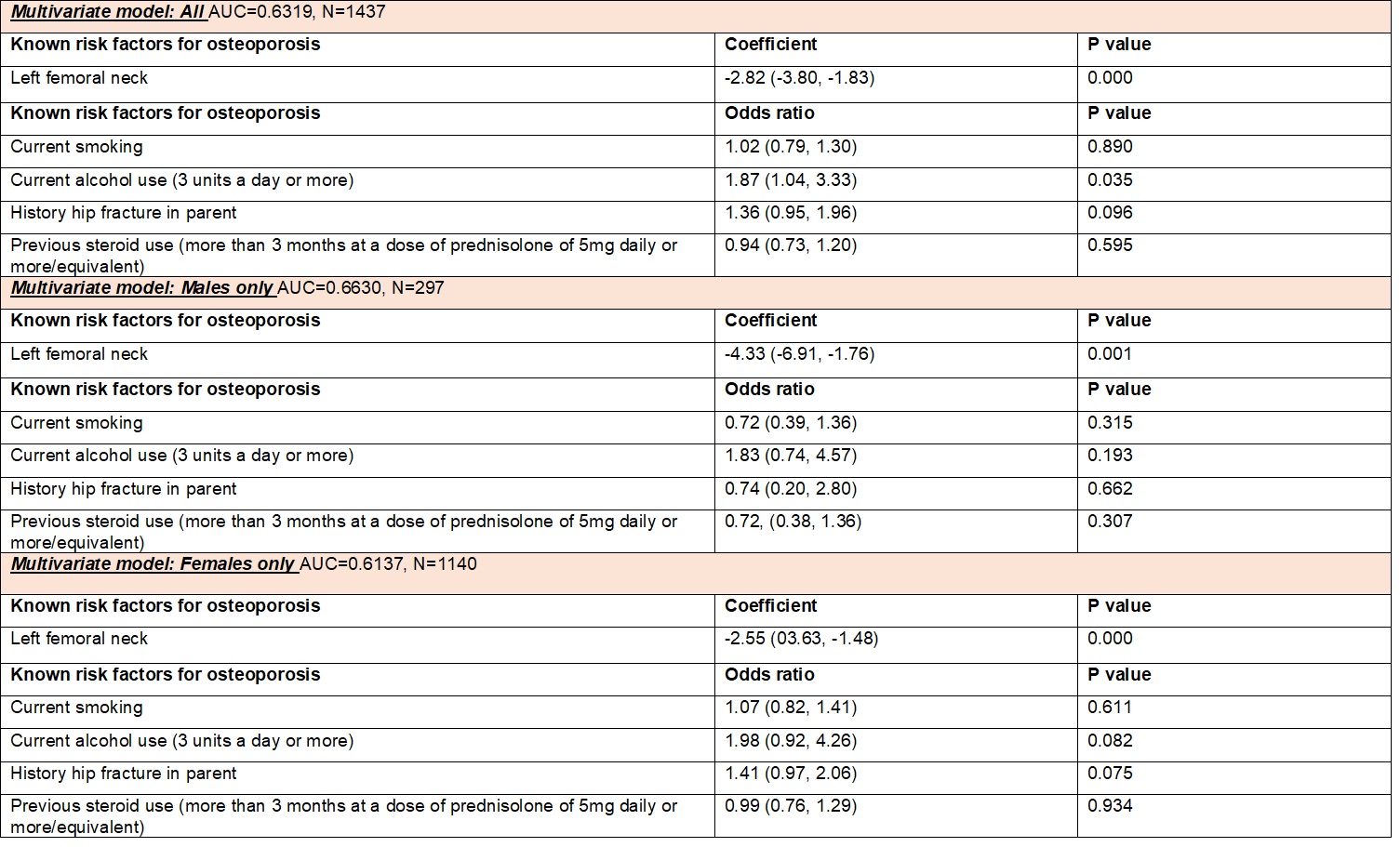 Table 3: Multivariate analysis: BMD of left femoral neck identified as most associated with fracture and used in combination with all available risk factors in 3 multivariate models. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measure, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve.
Table 3: Multivariate analysis: BMD of left femoral neck identified as most associated with fracture and used in combination with all available risk factors in 3 multivariate models. All models were adjusted for age at first scan, BMI and overall analysis was also adjusted for sex. Results are reported as beta coefficients for BMD measure, and as odds ratios for all other risk factors. Results are reported with 95% confidence intervals and area under ROC curve. Disclosures: S. Sharma, None; M. Bukhari, None.

