Back
Poster Session A
Professional development and education
Session: (0214–0240) Professional Education Poster
0231: Primary Care Physician’s Perspective and Needs on Early Rheumatoid Arthritis Diagnosis: REUCARE Program for Early Referral
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CB
Camille Bourgeois, MD
Hospital general universitario Gregorio Marañón
Madrid, Spain
Abstract Poster Presenter(s)
Camille Bourgeois1, Jorge Olmedo Galindo2, Juan Molina1, Gema Fernandez-Plana2, Julia Martinez-Barrio1, Javier Rivera3 and Isabel Castrejon4, 1Hospital General Universitario Gregorio Marañón, Madrid, Spain, 2Gerencia Asistencial Atención Primaria, Comunidad de Madrid, Madrid, Spain, 3Department of Rheumatology, Hospital General Universitario Gregorio Marañón, Madrid, Spain, 4Hospital Universitario Gregorio Marañón, Madrid, Spain
Background/Purpose: Primary care physicians (PCPs) play a crucial role in early recognition and rapid referral of patients with inflammatory arthritis to improve early management and patient outcomes. However, there is limited information on perceived barriers for referral and areas of improvement (1). The purpose of this study is to explore the perspective and needs of PCPs to guide a specialist's referral program.
Methods: A PCPs-rheumatology early referral program (REUCARE) has been initiated at our area in January 2022 with 257 PCPs participating. Up to May 2022, 88 patients have been referred, however only 24 (27%) fulfill inclusion criteria. In order to improve the referral strategy, a survey has been developed in collaboration with primary care investigators to explore areas of improvement. The survey included 5 domains covering: PCPs demographics, previous knowledge about RA, level of confidence, factors and potential barriers influencing referral and interest on rheumatological training. Data were captured using four-point Likert scales, yes/no question or free text, and were analyzed descriptively.
Results: E-mail invitations were sent to 257 PCPs through their primary care center coordinator and completed by 26 (10% response rate). More respondents were women (76%) in practice for over more than 20 years who reported having 30-40 patients per day and only 1-5 patients diagnosed of RA in the last year. The majority (83%) reported additional rheumatological training besides medical school, however they were no familiar with the incidence and prevalence of the disease. Around 67% were aware of the importance of early diagnosis and treatment, however they felt not very confident making the initial diagnostic (61% "somehow confident" and 35% "not confident"). Main reasons for referral were clinical presentation (65%), positive rheumatoid factor (46%) and elevation of acute phase reactants (46%). Most PCPs considered the waiting time for rheumatology prolonged (65%) and very prolonged (22%) and reported insufficient feedback information from rheumatologists (60%). Main reasons for delay from PCPs perspective were nonspecific initial symptoms of the disease (48%) followed by rheumatology long waiting list (39%) (Figure 1). Although 77% indicated using additional resources to improve their knowledge in RA, all participants stated that they would be interested in receiving more information on early diagnosis, being the preferred resources a specific e-consult (87%), updated mini guidelines (78%) and face-to face meetings with rheumatologists (Figure 2).
Conclusion: Most PCPs are aware of the importance of early diagnosis and management of RA but feel uncomfortable making the initial diagnosis. Non-specific initial symptoms and long waiting lists for rheumatology are the main reasons for delay from PCPs perspective. Resources to improve referral, including e-consult and specific guidelines, are in need as part of the actual referral program.
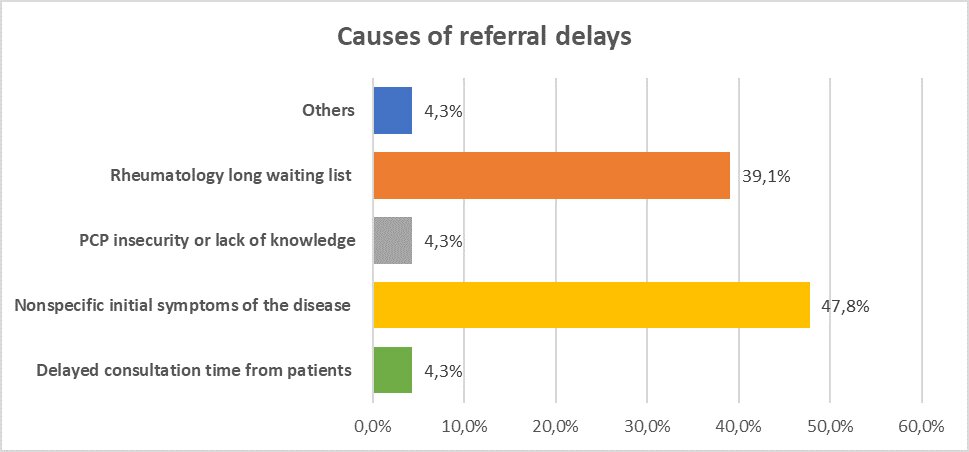 Figure 1: Causes of referral delays
Figure 1: Causes of referral delays
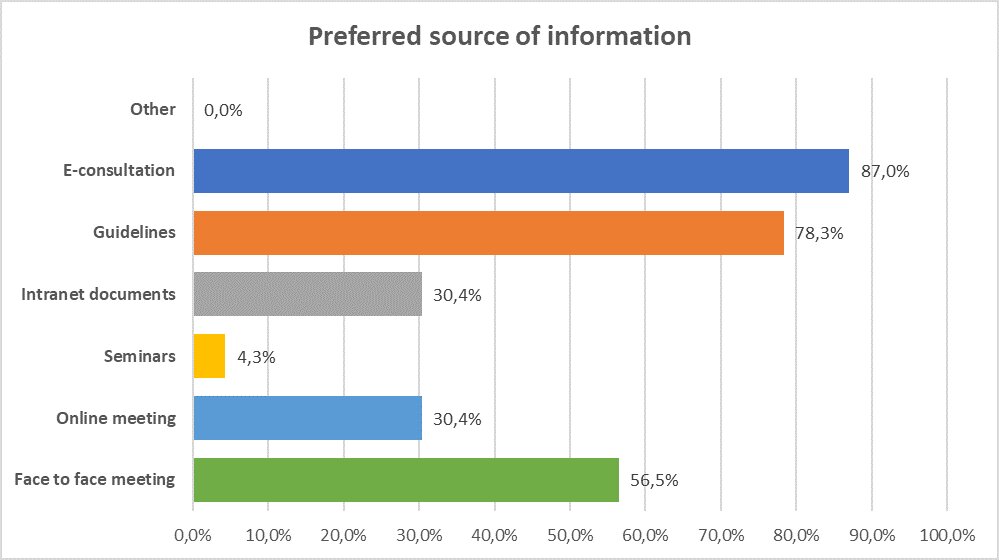 Figure 2: Preferred source of information
Figure 2: Preferred source of information
Disclosures: C. Bourgeois, None; J. Olmedo Galindo, None; J. Molina, None; G. Fernandez-Plana, None; J. Martinez-Barrio, None; J. Rivera, None; I. Castrejon, None.
Background/Purpose: Primary care physicians (PCPs) play a crucial role in early recognition and rapid referral of patients with inflammatory arthritis to improve early management and patient outcomes. However, there is limited information on perceived barriers for referral and areas of improvement (1). The purpose of this study is to explore the perspective and needs of PCPs to guide a specialist's referral program.
Methods: A PCPs-rheumatology early referral program (REUCARE) has been initiated at our area in January 2022 with 257 PCPs participating. Up to May 2022, 88 patients have been referred, however only 24 (27%) fulfill inclusion criteria. In order to improve the referral strategy, a survey has been developed in collaboration with primary care investigators to explore areas of improvement. The survey included 5 domains covering: PCPs demographics, previous knowledge about RA, level of confidence, factors and potential barriers influencing referral and interest on rheumatological training. Data were captured using four-point Likert scales, yes/no question or free text, and were analyzed descriptively.
Results: E-mail invitations were sent to 257 PCPs through their primary care center coordinator and completed by 26 (10% response rate). More respondents were women (76%) in practice for over more than 20 years who reported having 30-40 patients per day and only 1-5 patients diagnosed of RA in the last year. The majority (83%) reported additional rheumatological training besides medical school, however they were no familiar with the incidence and prevalence of the disease. Around 67% were aware of the importance of early diagnosis and treatment, however they felt not very confident making the initial diagnostic (61% "somehow confident" and 35% "not confident"). Main reasons for referral were clinical presentation (65%), positive rheumatoid factor (46%) and elevation of acute phase reactants (46%). Most PCPs considered the waiting time for rheumatology prolonged (65%) and very prolonged (22%) and reported insufficient feedback information from rheumatologists (60%). Main reasons for delay from PCPs perspective were nonspecific initial symptoms of the disease (48%) followed by rheumatology long waiting list (39%) (Figure 1). Although 77% indicated using additional resources to improve their knowledge in RA, all participants stated that they would be interested in receiving more information on early diagnosis, being the preferred resources a specific e-consult (87%), updated mini guidelines (78%) and face-to face meetings with rheumatologists (Figure 2).
Conclusion: Most PCPs are aware of the importance of early diagnosis and management of RA but feel uncomfortable making the initial diagnosis. Non-specific initial symptoms and long waiting lists for rheumatology are the main reasons for delay from PCPs perspective. Resources to improve referral, including e-consult and specific guidelines, are in need as part of the actual referral program.
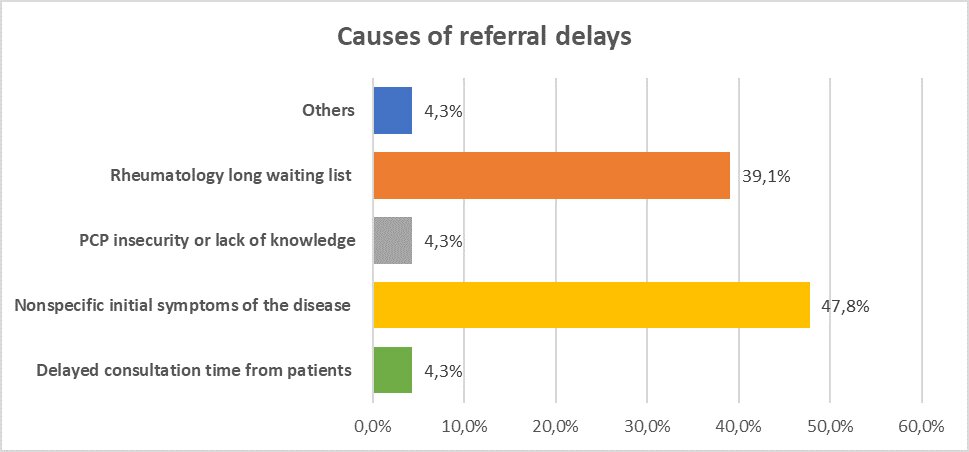 Figure 1: Causes of referral delays
Figure 1: Causes of referral delays 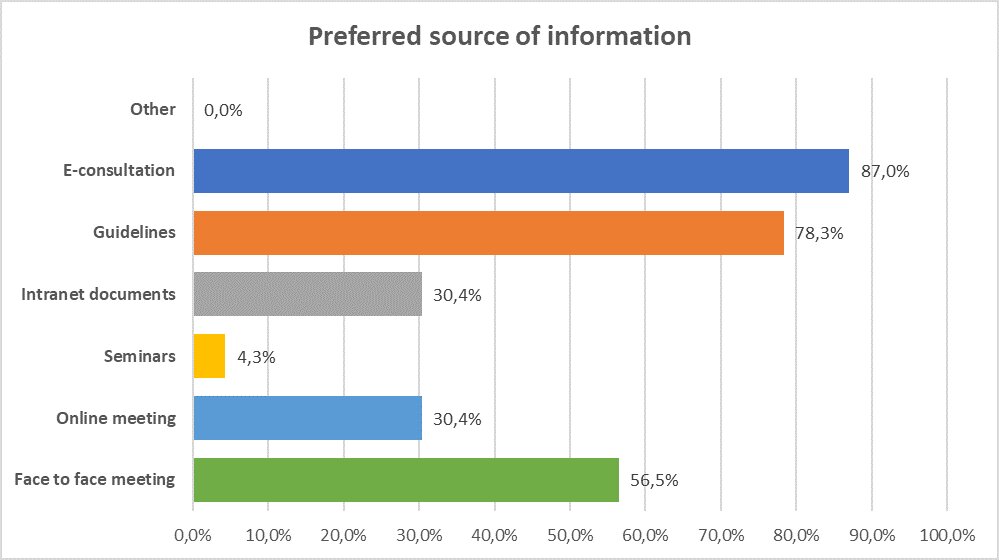 Figure 2: Preferred source of information
Figure 2: Preferred source of information Disclosures: C. Bourgeois, None; J. Olmedo Galindo, None; J. Molina, None; G. Fernandez-Plana, None; J. Martinez-Barrio, None; J. Rivera, None; I. Castrejon, None.

