Back
Poster Session A
Vasculitis
Session: (0432–0457) Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
0446: The Burden of Coronary Artery Calcification in ANCA-Associated Vasculitis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ZW
Zachary Wallace, MD, MSc
Massachusetts General Hospital
Newton, MA, United States
Abstract Poster Presenter(s)
Anushri Parakh1, Claire Cook1, Xiaoqing Fu1, sandeep hedgire1, John Stone2, Hyon Choi3, Michael Lu1 and Zachary Wallace1, 1Massachusetts General Hospital, Boston, MA, 2Massachusetts General Hospital Rheumatology Unit, Harvard Medical School, Boston, MA, 3MASSACHUSETTS GENERAL HOSPITAL, Lexington, MA
Background/Purpose: ANCA-associated vasculitis (AAV) is associated with an increased risk of cardiovascular (CV) disease, with MPO- AAV conferring a higher risk of CV events than PR3-ANCA+ AAV1,2. The coronary artery calcium (CAC) score is a measure of atherosclerotic burden and associated with future CV events in the general population. We investigated the burden of CAC in AAV.
Methods: We identified patients in the 2002-2019 Mass General Brigham (MGB) AAV Cohort with a non-contrast computed tomography (CT) scan of the chest performed for clinical purposes. The 2002-2019 MGB AAV Cohort includes consecutive patients who are PR3- or MPO-ANCA+. Patients with prior coronary intervention or bypass surgery were excluded. CAC scores were calculated using the Agatston method. We determined age, sex, and race-standardized percentiles of CAC scores using the Multi-Ethnic Study of Atherosclerosis (MESA) tool. We assessed the association of baseline features of AAV disease activity with CAC using linear regression. We determined the differences in CAC among MPO- vs PR3-ANCA+ AAV using t-tests and linear regression. When comparing CAC scores, we adjusted for age and sex.
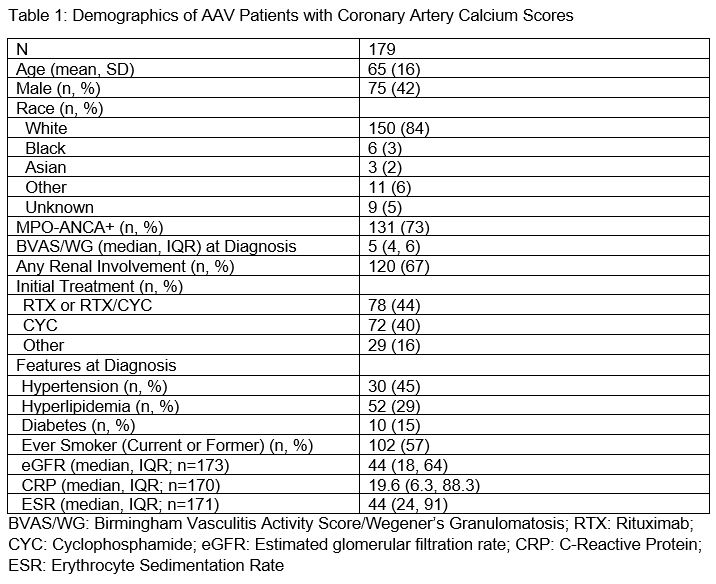
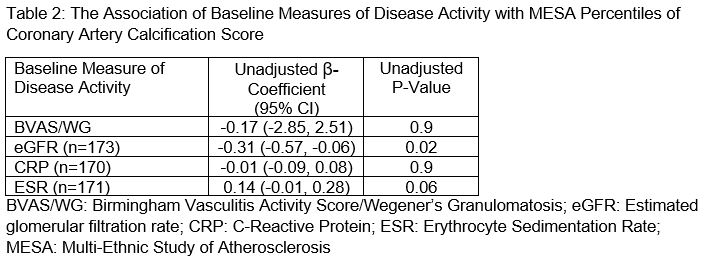
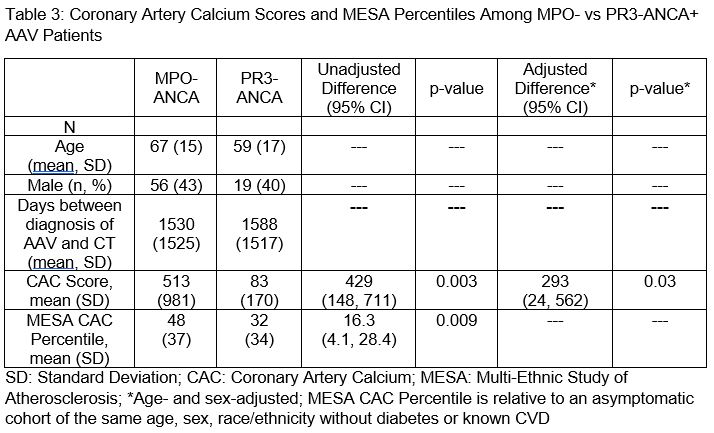
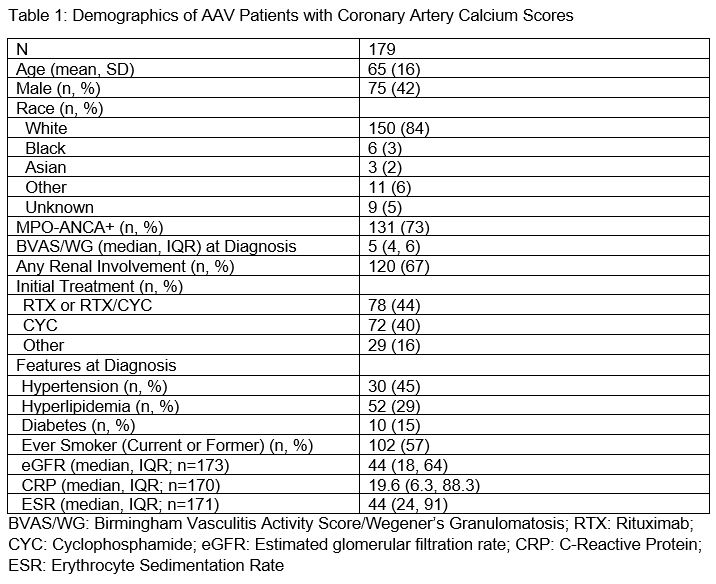
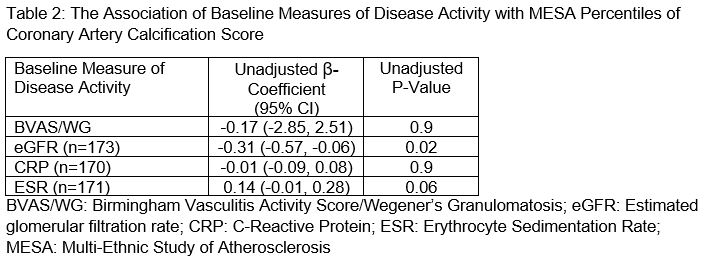
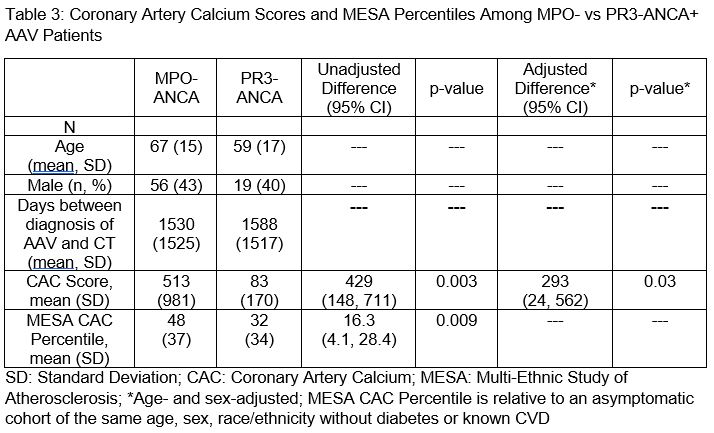
Results: Of 179 patients, the mean age was 65 years, 58% were female, and 73% were MPO-ANCA+. At diagnosis, 45% had hypertension, 29% had hyperlipidemia, 15% had diabetes, and 57% were ever smokers. The mean baseline eGFR was 44 ml/min. MPO-ANCA+ patients were older than PR3-ANCA+ patients (67 vs 59 yrs); a similar proportion were female (57% vs 60%). The mean CAC score was 398 (±865) and 120 (67%) patients had calcification. In the entire cohort, the mean MESA percentile was 44 (±37). There was an inverse association of eGFR at AAV diagnosis with MESA percentile (β -0.31 (95%CI -0.57 to -0.06) / 1ml/min, p=0.02). There was a trend toward association of baseline ESR with MESA percentile (β 0.14 (95%CI -0.01 to 0.28) / 1mm/hr increase, p=0.06). Baseline BVAS/WG and CRP were not associated with MESA percentiles. The mean days from AAV diagnosis to the CT used to measure CAC was similar in MPO- and PR3-ANCA+ patients (1530 vs 1588 days, p=0.8). The mean MESA percentile was higher among MPO- vs PR3-ANCA+ AAV (48 (37) vs 32 (34), difference +16.3 [95% CI 4.1-28.4], p=0.009). The mean CAC score was greater in MPO- vs PR3-ANCA+ AAV (adjusted difference +293 [95%CI 24-562], p=0.03).
Conclusion: Coronary artery calcification is common in AAV and associated with renal function and the inflammatory state. Compared with PR3-ANCA+, CAC burden in MPO-ANCA+ was greater than expected based on age, sex, and race. These findings support prior observations that MPO-ANCA+ AAV has a higher risk for CVD. The overall burden of CAC was not greater than expected for age, sex, and race. This has been observed in other inflammatory conditions (e.g., HIV) where non-calcified plaque is a strong contributor to CV risk2. Prospective studies are needed to comprehensively investigate both calcified and non-calcified plaque among patients to elucidate factors driving CV risk.
1Arthritis Care Res 2011;63:588
2Rheumatology 2020;59:2308
3J Am Heart Assoc. 2021;10:e019291
Disclosures: A. Parakh, None; C. Cook, None; X. Fu, None; s. hedgire, None; J. Stone, Horizon Theraputics, Sanofi, Amgen, Argenx, Bristol-Myers Squibb(BMS), Chemocentryx, Kyverna, Novartis, Palleon Pharmaceuticals, PPD, Q32, Star Therapeutics, Roche, Mirabio, Spruce Biosciences, Steritas, Zenas; H. Choi, Horizon, Allena, LG, Protalix; M. Lu, AstraZeneca, MedImmune, Kowa; Z. Wallace, Sanofi, Bristol-Myers Squibb(BMS), Zenas Biopharma, Shionogi, Horizon.
Background/Purpose: ANCA-associated vasculitis (AAV) is associated with an increased risk of cardiovascular (CV) disease, with MPO- AAV conferring a higher risk of CV events than PR3-ANCA+ AAV1,2. The coronary artery calcium (CAC) score is a measure of atherosclerotic burden and associated with future CV events in the general population. We investigated the burden of CAC in AAV.
Methods: We identified patients in the 2002-2019 Mass General Brigham (MGB) AAV Cohort with a non-contrast computed tomography (CT) scan of the chest performed for clinical purposes. The 2002-2019 MGB AAV Cohort includes consecutive patients who are PR3- or MPO-ANCA+. Patients with prior coronary intervention or bypass surgery were excluded. CAC scores were calculated using the Agatston method. We determined age, sex, and race-standardized percentiles of CAC scores using the Multi-Ethnic Study of Atherosclerosis (MESA) tool. We assessed the association of baseline features of AAV disease activity with CAC using linear regression. We determined the differences in CAC among MPO- vs PR3-ANCA+ AAV using t-tests and linear regression. When comparing CAC scores, we adjusted for age and sex.
Results: Of 179 patients, the mean age was 65 years, 58% were female, and 73% were MPO-ANCA+. At diagnosis, 45% had hypertension, 29% had hyperlipidemia, 15% had diabetes, and 57% were ever smokers. The mean baseline eGFR was 44 ml/min. MPO-ANCA+ patients were older than PR3-ANCA+ patients (67 vs 59 yrs); a similar proportion were female (57% vs 60%). The mean CAC score was 398 (±865) and 120 (67%) patients had calcification. In the entire cohort, the mean MESA percentile was 44 (±37). There was an inverse association of eGFR at AAV diagnosis with MESA percentile (β -0.31 (95%CI -0.57 to -0.06) / 1ml/min, p=0.02). There was a trend toward association of baseline ESR with MESA percentile (β 0.14 (95%CI -0.01 to 0.28) / 1mm/hr increase, p=0.06). Baseline BVAS/WG and CRP were not associated with MESA percentiles. The mean days from AAV diagnosis to the CT used to measure CAC was similar in MPO- and PR3-ANCA+ patients (1530 vs 1588 days, p=0.8). The mean MESA percentile was higher among MPO- vs PR3-ANCA+ AAV (48 (37) vs 32 (34), difference +16.3 [95% CI 4.1-28.4], p=0.009). The mean CAC score was greater in MPO- vs PR3-ANCA+ AAV (adjusted difference +293 [95%CI 24-562], p=0.03).
Conclusion: Coronary artery calcification is common in AAV and associated with renal function and the inflammatory state. Compared with PR3-ANCA+, CAC burden in MPO-ANCA+ was greater than expected based on age, sex, and race. These findings support prior observations that MPO-ANCA+ AAV has a higher risk for CVD. The overall burden of CAC was not greater than expected for age, sex, and race. This has been observed in other inflammatory conditions (e.g., HIV) where non-calcified plaque is a strong contributor to CV risk2. Prospective studies are needed to comprehensively investigate both calcified and non-calcified plaque among patients to elucidate factors driving CV risk.
1Arthritis Care Res 2011;63:588
2Rheumatology 2020;59:2308
3J Am Heart Assoc. 2021;10:e019291
Disclosures: A. Parakh, None; C. Cook, None; X. Fu, None; s. hedgire, None; J. Stone, Horizon Theraputics, Sanofi, Amgen, Argenx, Bristol-Myers Squibb(BMS), Chemocentryx, Kyverna, Novartis, Palleon Pharmaceuticals, PPD, Q32, Star Therapeutics, Roche, Mirabio, Spruce Biosciences, Steritas, Zenas; H. Choi, Horizon, Allena, LG, Protalix; M. Lu, AstraZeneca, MedImmune, Kowa; Z. Wallace, Sanofi, Bristol-Myers Squibb(BMS), Zenas Biopharma, Shionogi, Horizon.

