Back
Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0343–0371) SLE – Treatment Poster I
0368: Which Are the Best Therapeutic Strategies for Systemic Lupus Erythematosus Severe Thrombocytopenia? A Ten Year Analysis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EC
Erik Cimé-Aké, MD
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán
Merida, Yucat�n, Mexico
Abstract Poster Presenter(s)
Erik Cimé-Aké, Ana Barrera-Vargas, Roberta Demichelis-Gómez, Martha Ramírez-Alemón and Marina Rull-Gabayet, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Ciudad de México, Mexico
Background/Purpose: Severe thrombocytopenia in systemic lupus erythematosus (SLE) is characterized by poor response to glucocorticoids and frequent relapses. Information regarding the risk of relapse with different treatment strategies is quite scant. The aim of this study was to analyze the acute and one-year response of severe thrombocytopenia to different treatment regimens.
Methods: This is a 10 year (2010–2019) retrospective study, in a third-level hospital in Mexico City. We included patients ≥18 years old, fulfilling the 2019 EULAR/ACR criteria for SLE, who were hospitalized because of a platelet count ≤30,000/µL due to SLE activity. Patients with another autoimmune disease except for antiphospholipid syndrome, thrombocytopenia due to other etiologies and thrombotic thrombocytopenic purpura were excluded. Remission was defined as a platelet count ≥100,000/µL after twelve months of initial treatment and relapse as a platelet count < 100,000/µL in at least two determinations. Relapse-free survival was considered as the time period from the date of hospital admission until the relapse date or up to one year after the initial treatment.
Results: A total of 47 patients were included, 83% were women with a median age of 31 years. During one year follow-up, 17% of patients relapsed. No difference was found between the relapse and no relapse groups regarding the years of SLE evolution (4 vs 4, p=0.656), APS (62.5% vs 25.6%, p=0.056), SLEDAI-2K (8 vs 7, p=0.875) and platelet count at admission (7,500/µL vs 8,000/µL, p=0.765). Table 1.
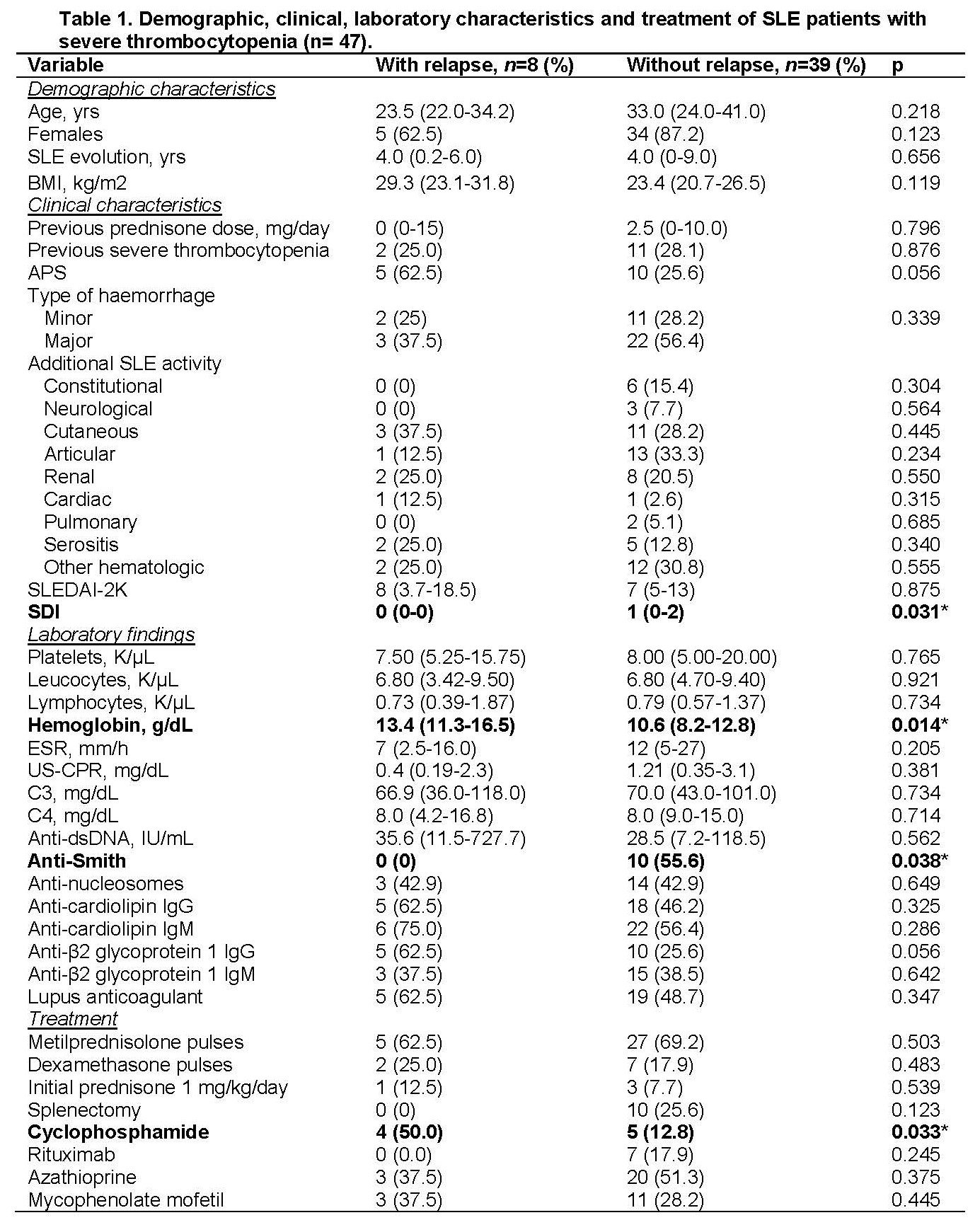
Cyclophosphamide administration was more frequent in patients without remission (50.0% vs 8.8%, p=0.017). For the time of relapse-free survival there was no difference in the initial management when using three pulses of 1 g methylprednisolone vs 40 mg dexamethasone for four days (50.0 vs 44.6 weeks, p=0.480), receiving steroid pulses or 1 mg/kg/day prednisone as initial glucocorticoid treatment (48.9 vs 42.1 weeks, p=0.646) or splenectomy (49.5 vs 43.7 weeks, p=0.114). Patients who received rituximab 1 g on days 1 and 15 as acute immunosuppressive therapy had longer relapse-free survival than those who were treated with cyclophosphamide 500-1200 mg monthly for 6 months (44.8 vs 37.8 weeks, p=0.040). For maintenance therapy there was no difference in relapse-free survival between using azathioprine 1-2 mg/kg/day or mycophenolate mofetil 1-3 g/day (51.2 vs 44.9 weeks, p=0.424). Figure 1.
Conclusion: Demographic and laboratory characteristics do not seem to influence the occurrence of relapse of SLE severe thrombocytopenia. We found no difference between receiving different IV or oral glucocorticoid regimens. Rituximab provided a longer relapse-free survival. Our study provides evidence on deciding for a better treatment strategy for SLE severe thrombocytopenia.
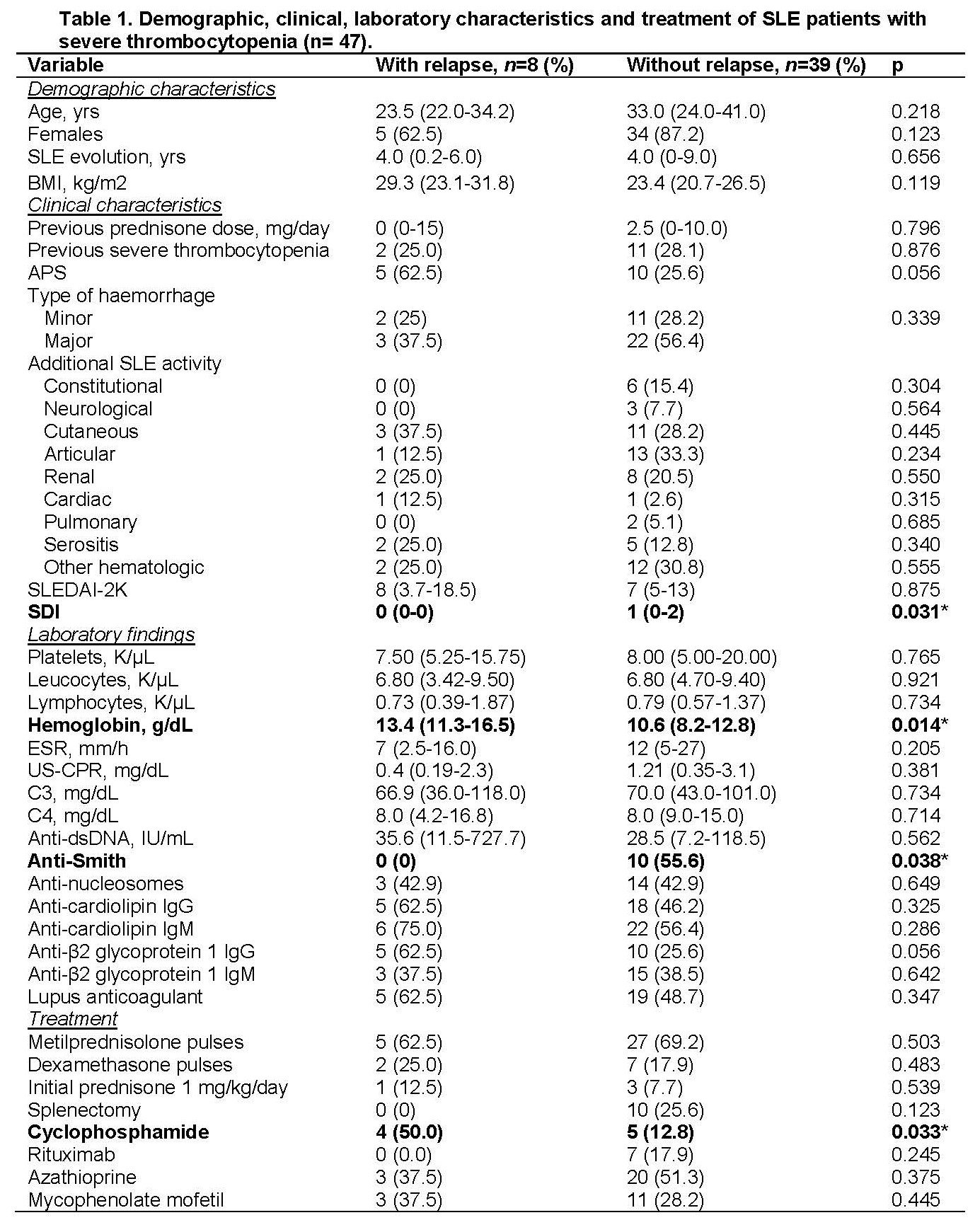 Data are expressed as number (percentage) or median (interquartile range). Statistical analysis: chi-square test or Fisher's exact test were used for nominal variables, and the Mann-Whitney U test was used for numerical variables.
Data are expressed as number (percentage) or median (interquartile range). Statistical analysis: chi-square test or Fisher's exact test were used for nominal variables, and the Mann-Whitney U test was used for numerical variables.
SDI: SLICC/ACR Damage Index, US-CPR: Ultra-Sensitive C-Reactive Protein.
*Statistically significant.
.jpg) Relapse-free survival according to the different therapeutic options and their comparisons. A: comparison of different intravenous steroid pulses; B: difference between starting the steroid as a pulse or orally; C: comparison of acute intravenous immunosuppressive therapy; D: difference between oral immunosuppressive maintenance treatments.
Relapse-free survival according to the different therapeutic options and their comparisons. A: comparison of different intravenous steroid pulses; B: difference between starting the steroid as a pulse or orally; C: comparison of acute intravenous immunosuppressive therapy; D: difference between oral immunosuppressive maintenance treatments.
MTP: metilprednisolone, DXM: dexamethasone, PDN: prednisone, RTX: rituximab, CYC: Cyclophosphamide, AZA: azathioprine, MMF: mycophenolate mofetil, wks: weeks.
Disclosures: E. Cimé-Aké, None; A. Barrera-Vargas, AstraZeneca, Sanofi; R. Demichelis-Gómez, AbbVie/Abbott, Amgen, Amgen, Gilead; M. Ramírez-Alemón, None; M. Rull-Gabayet, None.
Background/Purpose: Severe thrombocytopenia in systemic lupus erythematosus (SLE) is characterized by poor response to glucocorticoids and frequent relapses. Information regarding the risk of relapse with different treatment strategies is quite scant. The aim of this study was to analyze the acute and one-year response of severe thrombocytopenia to different treatment regimens.
Methods: This is a 10 year (2010–2019) retrospective study, in a third-level hospital in Mexico City. We included patients ≥18 years old, fulfilling the 2019 EULAR/ACR criteria for SLE, who were hospitalized because of a platelet count ≤30,000/µL due to SLE activity. Patients with another autoimmune disease except for antiphospholipid syndrome, thrombocytopenia due to other etiologies and thrombotic thrombocytopenic purpura were excluded. Remission was defined as a platelet count ≥100,000/µL after twelve months of initial treatment and relapse as a platelet count < 100,000/µL in at least two determinations. Relapse-free survival was considered as the time period from the date of hospital admission until the relapse date or up to one year after the initial treatment.
Results: A total of 47 patients were included, 83% were women with a median age of 31 years. During one year follow-up, 17% of patients relapsed. No difference was found between the relapse and no relapse groups regarding the years of SLE evolution (4 vs 4, p=0.656), APS (62.5% vs 25.6%, p=0.056), SLEDAI-2K (8 vs 7, p=0.875) and platelet count at admission (7,500/µL vs 8,000/µL, p=0.765). Table 1.
Cyclophosphamide administration was more frequent in patients without remission (50.0% vs 8.8%, p=0.017). For the time of relapse-free survival there was no difference in the initial management when using three pulses of 1 g methylprednisolone vs 40 mg dexamethasone for four days (50.0 vs 44.6 weeks, p=0.480), receiving steroid pulses or 1 mg/kg/day prednisone as initial glucocorticoid treatment (48.9 vs 42.1 weeks, p=0.646) or splenectomy (49.5 vs 43.7 weeks, p=0.114). Patients who received rituximab 1 g on days 1 and 15 as acute immunosuppressive therapy had longer relapse-free survival than those who were treated with cyclophosphamide 500-1200 mg monthly for 6 months (44.8 vs 37.8 weeks, p=0.040). For maintenance therapy there was no difference in relapse-free survival between using azathioprine 1-2 mg/kg/day or mycophenolate mofetil 1-3 g/day (51.2 vs 44.9 weeks, p=0.424). Figure 1.
Conclusion: Demographic and laboratory characteristics do not seem to influence the occurrence of relapse of SLE severe thrombocytopenia. We found no difference between receiving different IV or oral glucocorticoid regimens. Rituximab provided a longer relapse-free survival. Our study provides evidence on deciding for a better treatment strategy for SLE severe thrombocytopenia.
 Data are expressed as number (percentage) or median (interquartile range). Statistical analysis: chi-square test or Fisher's exact test were used for nominal variables, and the Mann-Whitney U test was used for numerical variables.
Data are expressed as number (percentage) or median (interquartile range). Statistical analysis: chi-square test or Fisher's exact test were used for nominal variables, and the Mann-Whitney U test was used for numerical variables.SDI: SLICC/ACR Damage Index, US-CPR: Ultra-Sensitive C-Reactive Protein.
*Statistically significant.
.jpg) Relapse-free survival according to the different therapeutic options and their comparisons. A: comparison of different intravenous steroid pulses; B: difference between starting the steroid as a pulse or orally; C: comparison of acute intravenous immunosuppressive therapy; D: difference between oral immunosuppressive maintenance treatments.
Relapse-free survival according to the different therapeutic options and their comparisons. A: comparison of different intravenous steroid pulses; B: difference between starting the steroid as a pulse or orally; C: comparison of acute intravenous immunosuppressive therapy; D: difference between oral immunosuppressive maintenance treatments. MTP: metilprednisolone, DXM: dexamethasone, PDN: prednisone, RTX: rituximab, CYC: Cyclophosphamide, AZA: azathioprine, MMF: mycophenolate mofetil, wks: weeks.
Disclosures: E. Cimé-Aké, None; A. Barrera-Vargas, AstraZeneca, Sanofi; R. Demichelis-Gómez, AbbVie/Abbott, Amgen, Amgen, Gilead; M. Ramírez-Alemón, None; M. Rull-Gabayet, None.

