Back
Abstract Session
Pediatric autoimmune diseases: Kawasaki disease, juvenile dermatomyositis and juvenile localized scleroderma
Session: Abstracts: Pediatric Rheumatology – Clinical I: Connective Tissue Disease (0512–0517)
0513: The Association Between Age of Diagnosis and Disease Characteristics and Damage in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis
Saturday, November 12, 2022
3:15 PM – 3:25 PM Eastern Time
Location: Room 126
- JB
Jessica Bloom, MD, MS
University of Colorado
Denver, CO, United States
Presenting Author(s)
Jessica Bloom1, Kaci Pickett2, Lori Silveira2, David Cuthbertson3, Nader Khalidi4, Curry Koening5, Carol Langford6, Carol McAlear7, Paul Monach8, Larry Moreland1, Christian Pagnoux9, Rennie Rhee10, Philip Seo11, Ulrich Specks12, Kenneth J. Warrington12, Robert Fuhlbrigge1 and Peter Merkel10, 1University of Colorado, Denver, CO, 2University of Colorado Anschutz Medical Campus, Aurora, CO, 3University of South Florida, Tampa, FL, 4McMaster University, Hamilton, ON, Canada, 5University of Texas Dell Medical School, Austin, TX, 6Cleveland Clinic, Cleveland, OH, 7University of Pennsylvania, Philadelphia, 8VA Boston Healthcare System, Boston, MA, 9Mount Sinai Hospital, Toronto, ON, Canada, 10University of Pennsylvania, Philadelphia, PA, 11Johns Hopkins University, Baltimore, MD, 12Mayo Clinic, Rochester, MN
Background/Purpose: Clinical characteristics and outcomes often differ between children and adults diagnosed with the same rheumatic condition; however, such comparative data is limited in ANCA-associated vasculitis (AAV). The objective of this study was to examine the relationship between age of diagnosis and disease characteristics and damage outcomes in patients with AAV.
Methods: This was a retrospective cohort analysis of patients with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021. Cohorts were divided by age of diagnosis (years): children (< 18), young adults (18-40), middle-aged ( > 40-65), and older adults ( > 65). Outcomes included demographics, ANCA type, and clinical characteristics. Group differences were tested using the Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical. Univariate and multivariate linear regression were used to estimate the differences in damage scores, Vasculitis Damage Index [VDI] and ANCA Vasculitis Index of Damage [AVID].
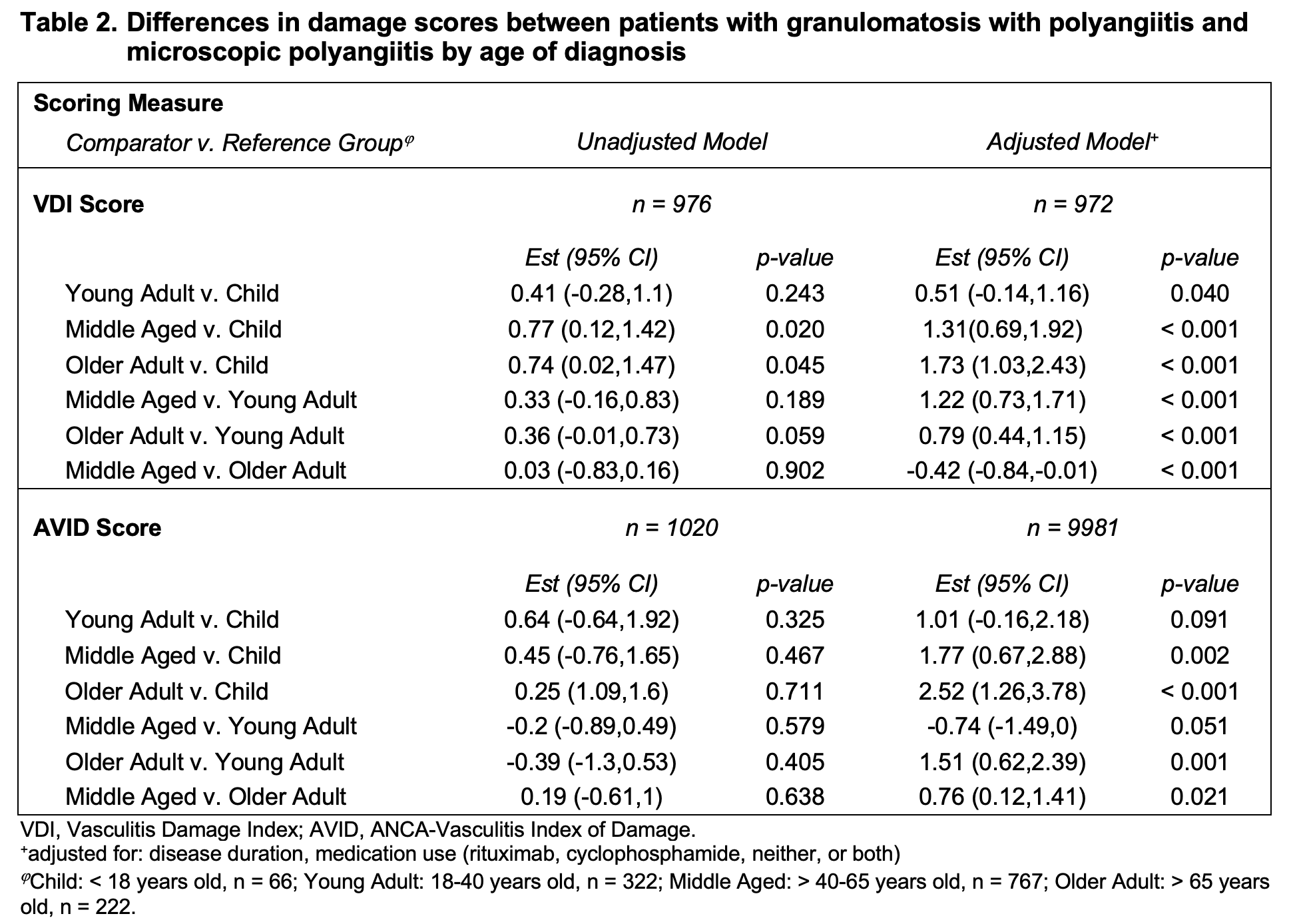
Results: Data from 1020 patients were analyzed: 61 children, 240 young adults, 560 middle aged, and 159 older adults (Table 1). 852 (84%) had GPA and 165 (16%) had MPA. 893 (92%) of patients with ANCA results were ANCA positive: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA, and 9 (1%) with both. AAV diagnosed in childhood had a female predominance that decreased with age and was more often GPA and ANCA/PR3-ANCA positive. Older adults had more MPA and MPO-ANCA. Those diagnosed in childhood experienced more subglottic stenosis and alveolar hemorrhage at diagnosis and ever. Ocular, nasal, sinus, renal, gastrointestinal, and nervous system manifestations were also different between groups. Over half of patients diagnosed in childhood received both cyclophosphamide (CYC) and rituximab (RTX) (Figure 1), a rate that decreased with increasing age groups. The percentage of patients receiving neither CYC or RTX, or CYC alone increased with older age at diagnosis. After adjusting for disease duration and use of CYC and/or RTX, the VDI and AVID scores of those diagnosed at age > 65 years were estimated to be 1.73 and 2.52 points higher, respectively, than those diagnosed as children (95%CI: [1.03,2.43], p < 0.001; [1.26,3.78], p < 0.001) (Table 2).
Conclusion: There is an association between age of diagnosis and clinical characteristics in patients with AAV, particularly when diagnosed in childhood. Most notably, children experience more subglottic stenosis and alveolar hemorrhage. An early-age female predominance wanes across age groups. Patients diagnosed in childhood are more likely to receive both CYC and RTX, a finding that may indicate different practices in pediatrics. Those diagnosed at an older age accrued more damage than those diagnosed at a younger age. While studies often exclude children, sub-analyses of adults diagnosed in childhood and more specific damage scores could provide insight into the unique aspects of AAV across the lifespan, allowing for more evidence-based care and improved outcomes.
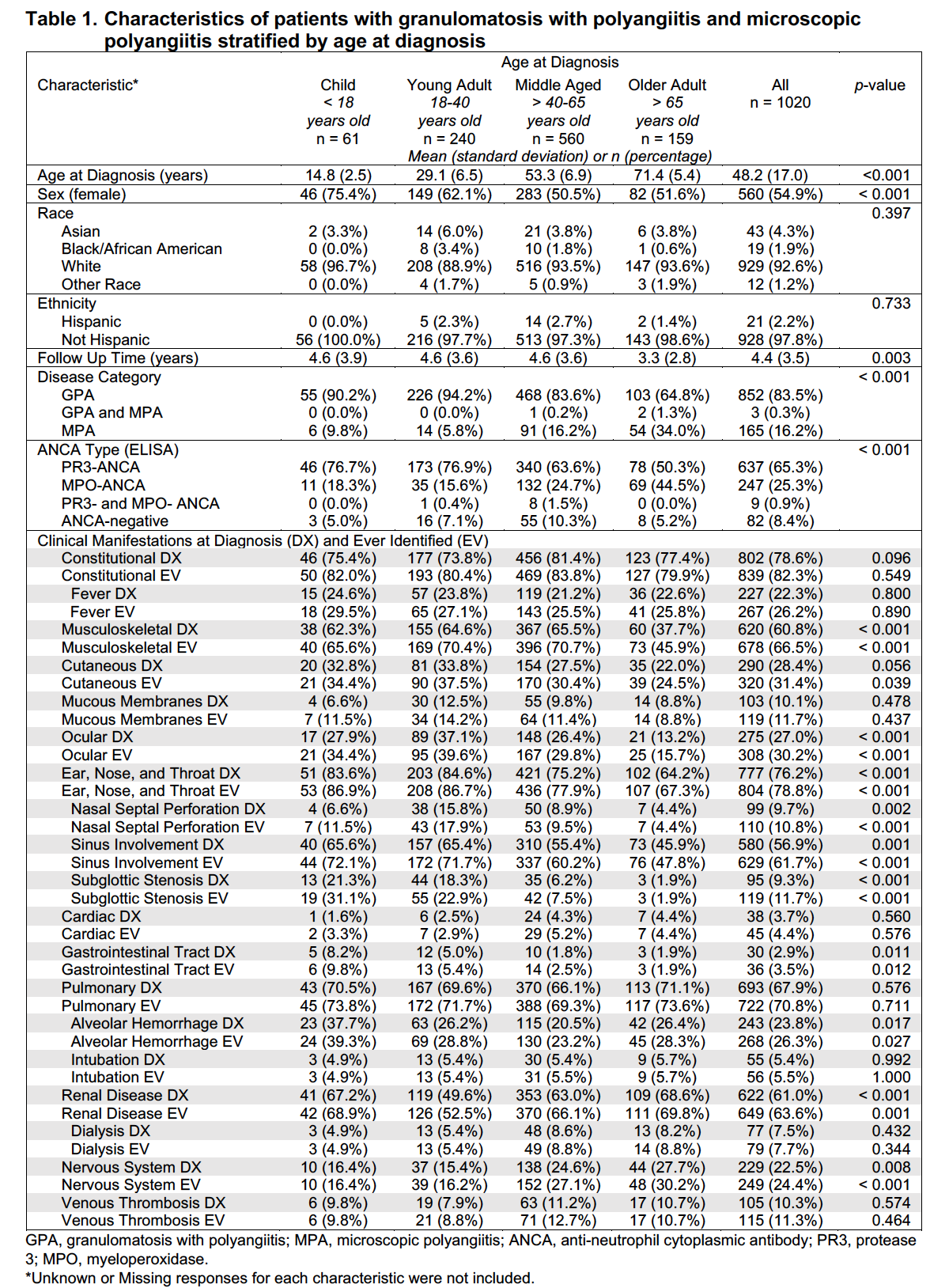
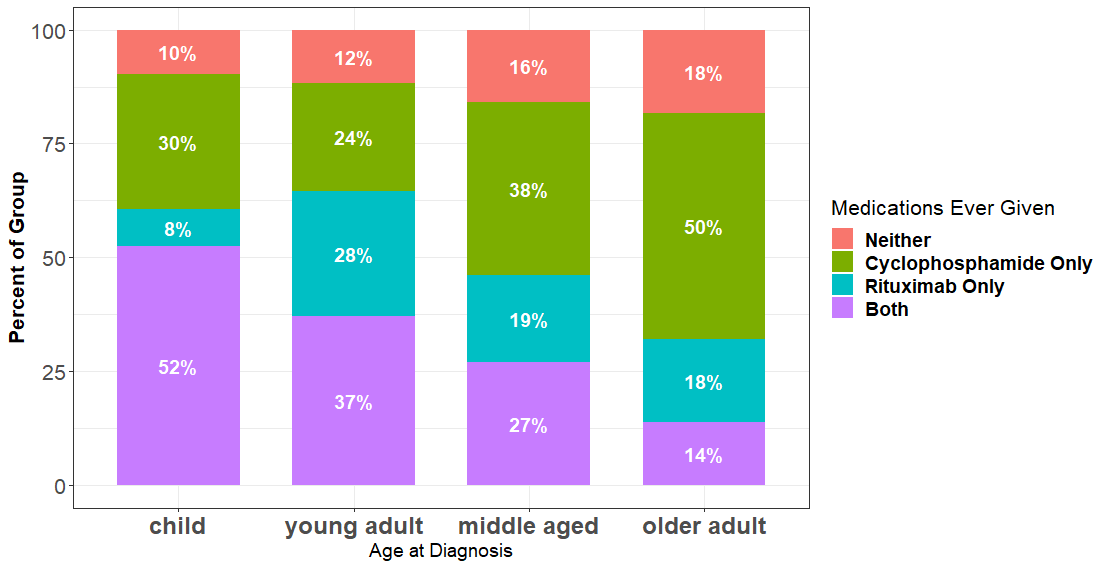 Figure 1. Medications ever received by patients with granulomatosis with polyangiitis and microscopic polyangiitis stratified by age at diagnosis
Figure 1. Medications ever received by patients with granulomatosis with polyangiitis and microscopic polyangiitis stratified by age at diagnosis
Disclosures: J. Bloom, None; K. Pickett, None; L. Silveira, None; D. Cuthbertson, None; N. Khalidi, AstraZeneca, Bristol-Myers Squibb(BMS), GlaxoSmithKlein(GSK), Roche, Sanofi, AbbVie/Abbott, Katsaka Medical, Otsuka; C. Koening, chemocentryx; C. Langford, None; C. McAlear, None; P. Monach, Chemocentryx, Kiniksa, BMS/Celgene, Gilead; L. Moreland, None; C. Pagnoux, otsuka, AstraZeneca, pfizer; R. Rhee, ChemoCentryx; P. Seo, None; U. Specks, AstraZeneca, Bristol-Myers Squibb(BMS), GlaxoSmithKlein(GSK), Genentech, AstraZeneca, Boehringer-Ingelheim, ChemoCentryx; K. Warrington, Eli Lilly, GlaxoSmithKlein(GSK), Kiniksa, Chemocentryx; R. Fuhlbrigge, None; P. Merkel, AbbVie, AstraZeneca, Boeringher-Ingelheim, Bristol-Myers Squibb, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Neutrolis, Takeda, CSL Behring, Dynacure, EMDSerono, Immagene, Jannsen, Kiniksa, Magenta, Novartis, Pfizer, Q32, Regeneron, Sparrow, Eicos, Electra, Kyverna, UpToDate.
Background/Purpose: Clinical characteristics and outcomes often differ between children and adults diagnosed with the same rheumatic condition; however, such comparative data is limited in ANCA-associated vasculitis (AAV). The objective of this study was to examine the relationship between age of diagnosis and disease characteristics and damage outcomes in patients with AAV.
Methods: This was a retrospective cohort analysis of patients with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021. Cohorts were divided by age of diagnosis (years): children (< 18), young adults (18-40), middle-aged ( > 40-65), and older adults ( > 65). Outcomes included demographics, ANCA type, and clinical characteristics. Group differences were tested using the Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical. Univariate and multivariate linear regression were used to estimate the differences in damage scores, Vasculitis Damage Index [VDI] and ANCA Vasculitis Index of Damage [AVID].
Results: Data from 1020 patients were analyzed: 61 children, 240 young adults, 560 middle aged, and 159 older adults (Table 1). 852 (84%) had GPA and 165 (16%) had MPA. 893 (92%) of patients with ANCA results were ANCA positive: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA, and 9 (1%) with both. AAV diagnosed in childhood had a female predominance that decreased with age and was more often GPA and ANCA/PR3-ANCA positive. Older adults had more MPA and MPO-ANCA. Those diagnosed in childhood experienced more subglottic stenosis and alveolar hemorrhage at diagnosis and ever. Ocular, nasal, sinus, renal, gastrointestinal, and nervous system manifestations were also different between groups. Over half of patients diagnosed in childhood received both cyclophosphamide (CYC) and rituximab (RTX) (Figure 1), a rate that decreased with increasing age groups. The percentage of patients receiving neither CYC or RTX, or CYC alone increased with older age at diagnosis. After adjusting for disease duration and use of CYC and/or RTX, the VDI and AVID scores of those diagnosed at age > 65 years were estimated to be 1.73 and 2.52 points higher, respectively, than those diagnosed as children (95%CI: [1.03,2.43], p < 0.001; [1.26,3.78], p < 0.001) (Table 2).
Conclusion: There is an association between age of diagnosis and clinical characteristics in patients with AAV, particularly when diagnosed in childhood. Most notably, children experience more subglottic stenosis and alveolar hemorrhage. An early-age female predominance wanes across age groups. Patients diagnosed in childhood are more likely to receive both CYC and RTX, a finding that may indicate different practices in pediatrics. Those diagnosed at an older age accrued more damage than those diagnosed at a younger age. While studies often exclude children, sub-analyses of adults diagnosed in childhood and more specific damage scores could provide insight into the unique aspects of AAV across the lifespan, allowing for more evidence-based care and improved outcomes.
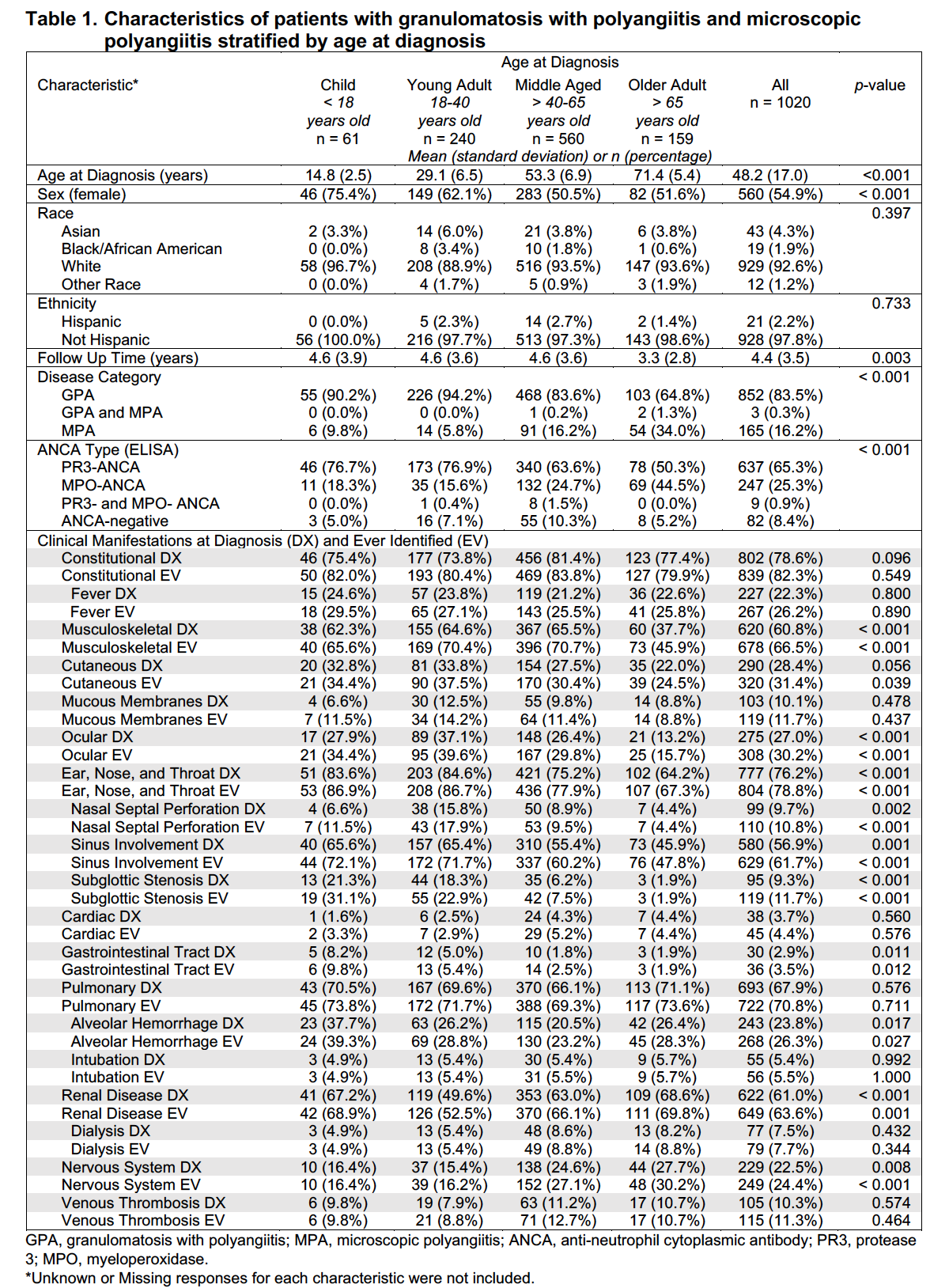
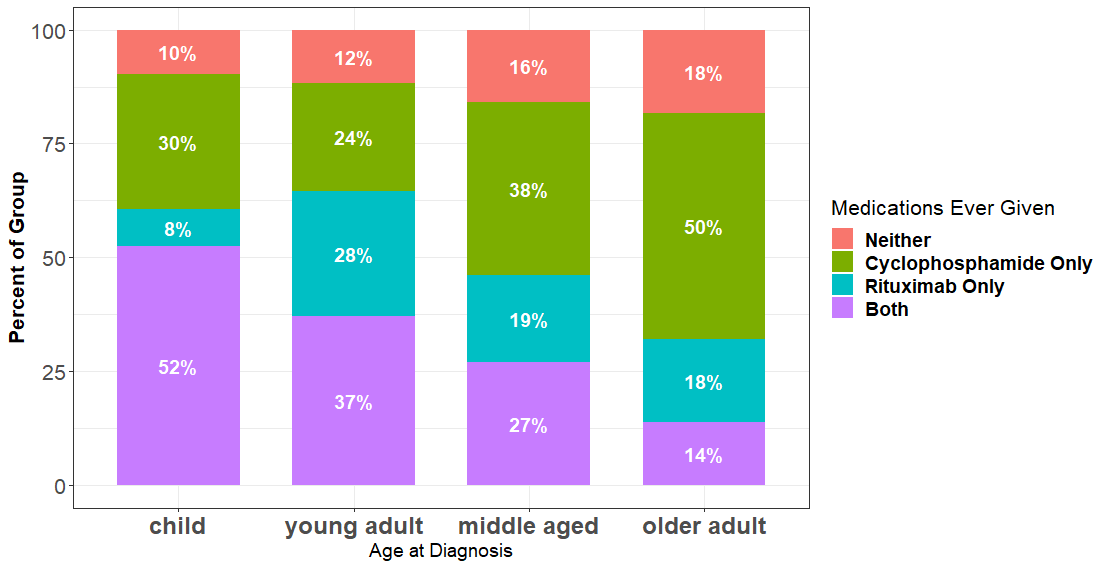 Figure 1. Medications ever received by patients with granulomatosis with polyangiitis and microscopic polyangiitis stratified by age at diagnosis
Figure 1. Medications ever received by patients with granulomatosis with polyangiitis and microscopic polyangiitis stratified by age at diagnosis 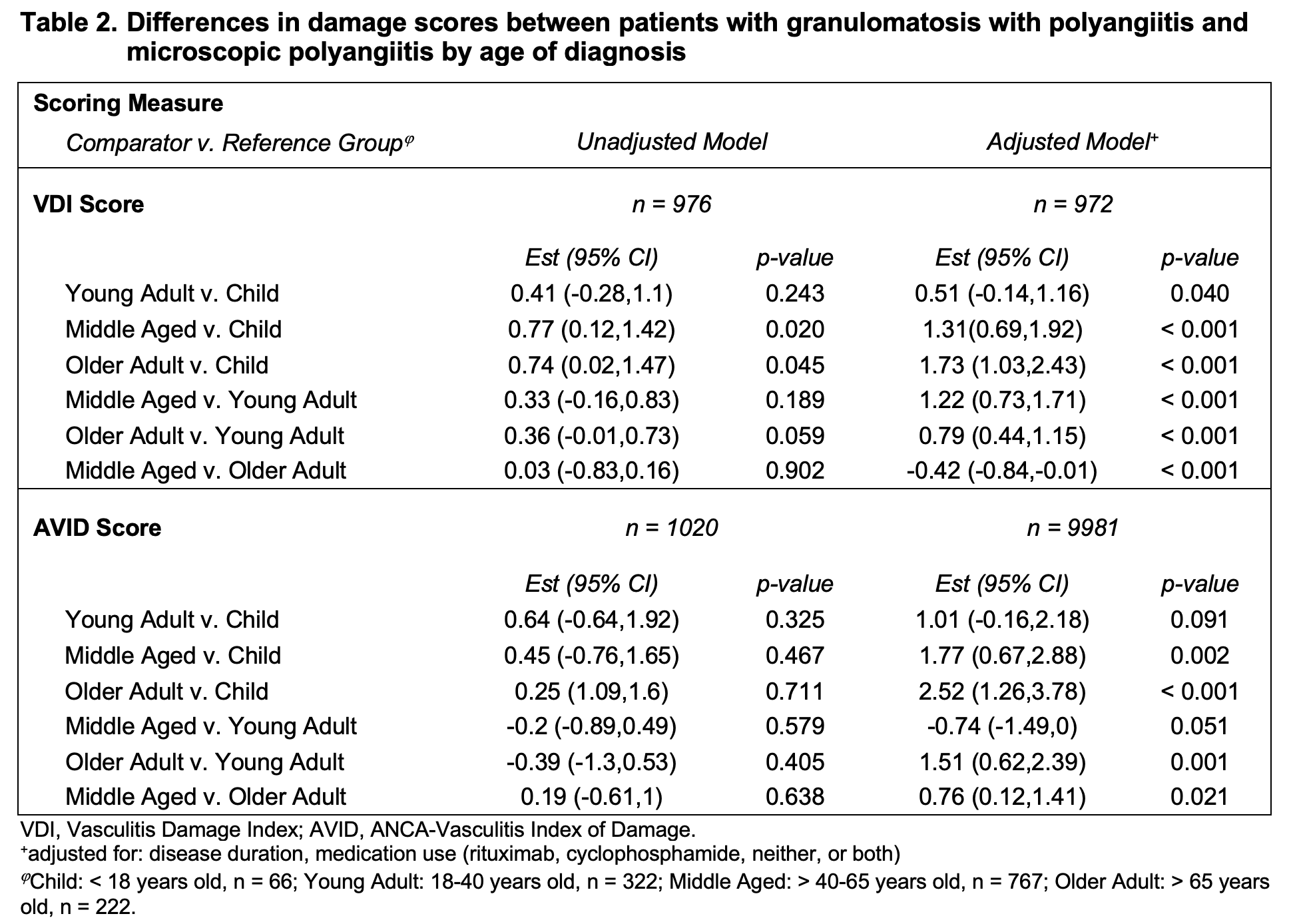
Disclosures: J. Bloom, None; K. Pickett, None; L. Silveira, None; D. Cuthbertson, None; N. Khalidi, AstraZeneca, Bristol-Myers Squibb(BMS), GlaxoSmithKlein(GSK), Roche, Sanofi, AbbVie/Abbott, Katsaka Medical, Otsuka; C. Koening, chemocentryx; C. Langford, None; C. McAlear, None; P. Monach, Chemocentryx, Kiniksa, BMS/Celgene, Gilead; L. Moreland, None; C. Pagnoux, otsuka, AstraZeneca, pfizer; R. Rhee, ChemoCentryx; P. Seo, None; U. Specks, AstraZeneca, Bristol-Myers Squibb(BMS), GlaxoSmithKlein(GSK), Genentech, AstraZeneca, Boehringer-Ingelheim, ChemoCentryx; K. Warrington, Eli Lilly, GlaxoSmithKlein(GSK), Kiniksa, Chemocentryx; R. Fuhlbrigge, None; P. Merkel, AbbVie, AstraZeneca, Boeringher-Ingelheim, Bristol-Myers Squibb, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Neutrolis, Takeda, CSL Behring, Dynacure, EMDSerono, Immagene, Jannsen, Kiniksa, Magenta, Novartis, Pfizer, Q32, Regeneron, Sparrow, Eicos, Electra, Kyverna, UpToDate.

