Back
Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes I: Pre- and Early Disease (0530–0535)
0532: Women with Early Rheumatoid Arthritis Less Likely to Achieve Rapid and Sustainable Remission: Results from the Canadian Early Arthritis Cohort Study
Saturday, November 12, 2022
5:00 PM – 5:10 PM Eastern Time
Location: Ballroom AB
- OS
Orit Schieir, PhD
McGill University
Montréal, QC, Canada
Presenting Author(s)
orit schieir1, Susan Bartlett2, Marie-France Valois1, Glen Hazlewood3, Louis Bessette4, Gilles Boire5, Carol Hitchon6, Edward Keystone7, Janet Pope8, diane tin9, Carter Thorne10, Vivian Bykerk11 and Canadian Early Arthritis Cohort (CATCH) Investigators12, 1McGill University, Montréal, QC, Canada, 2McGill University, Montreal, QC, Canada, 3University of Calgary, Calgary, AB, Canada, 4Centre de l'Ostoporose et de Rhumatologie de Québec, Québec, QC, Canada, 5Universite de Sherbrooke, Sherbrooke, QC, Canada, 6University of Manitoba, Winnipeg, MB, Canada, 7Keystone Consulting Enterprises Inc., Toronto, ON, Canada, 8University of Western Ontario, London, ON, Canada, 9Centre of Arthritis Excellence (CArE), Newmarket, ON, Canada, 10Southlake Regional Health Centre, Newmarket, ON, Canada, 11Hospital for Special Surgery, New York, NY, 12The Canadian Early Arthritis Cohort (CATCH), Bowmanville, ON, Canada
Background/Purpose: Historical and established RA cohorts have reported sex disparities in remission outcomes favoring male patients. The objective of the present study was to compare early, and sustained remission in men and women with early rheumatoid arthritis (ERA) receiving guideline-based care in rheumatology clinics across Canada.
Methods: Data were from participants enrolled in the Canadian Early Arthritis Cohort (CATCH) study between 2007 and 2019. CATCH is a multi-center inception cohort of ERA patients (symptoms < 1 year, 83 % meeting RA criteria at enrolment) diagnosed and treated in rheumatology centers across Canada. Participants completed standardized study visits including detailed RA clinical assessments, patient-reported outcomes, and laboratory investigations every 3 months in the first year, every 6-months in the second year and annually thereafter mirroring real-world care practices in Canada. Treatment decisions were at the discretion of the treating rheumatologist in line with treat-to-target guidelines. Descriptive statistics were used to summarize and compare prevalence of SDAI remission (< 3.3.), median time to SDAI remission and sustained SDAI remission 12- and 24- months after first remission across men and women. Multivariable multinomial regression was used to identify predictors of minor flares (SDAI REM→LDA) and major flares (SDAI REM→MDA/HDA) over 24-months follow-up from first remission.
Results: The sample included 2,743 ERA patients (1933 women; 789 men). At enrolment, mean(sd) SDAI was high at 27.4 (14.6); most patients were treated with csDMARDs (92%), often with MTX, as monotherapy or in combination with csDMARDs (77%) and 29% were prescribed oral steroids. There were no notable differences in disease activity or treatment strategies observed between men and women at enrolment. Overall prevalence of SDAI remission over the study follow-up was similar across men (64%) and women (61%), however median time-to-remission was longer for women vs. men (19.2 months vs 16.1 months, p =0.0358), and a lower proportion of women vs. men reached early remission targets by 12-months (37% vs 43%, p=0.0054). Sustained remission 12- and 24- months after first remission was also higher in men vs. women (Figure). Predictors of minor and major flares after remission differed by sex (Table). Smoking, seropositivity and residual disability at first SDAI remission predicted flares in men, while obesity, comorbidities and higher SDAI at first remission predicted flares in women. Treatment with advanced therapy at first remission was associated with lower likelihood of flares after remission in women.
Conclusion: Results of this large longitudinal study of ERA patients receiving contemporary guideline-based care showed high overall rates of SDAI remission for men and women over the study period, however there were notable sex differences favoring men in the rapidity and sustainability of remission. Predictors of minor and major flares after remission also differed between men and women and highlighted potential modifiable risk factors for sustaining remission over longer periods including smoking and residual disability at remission in men, and obesity and chronic comorbidity management in women.
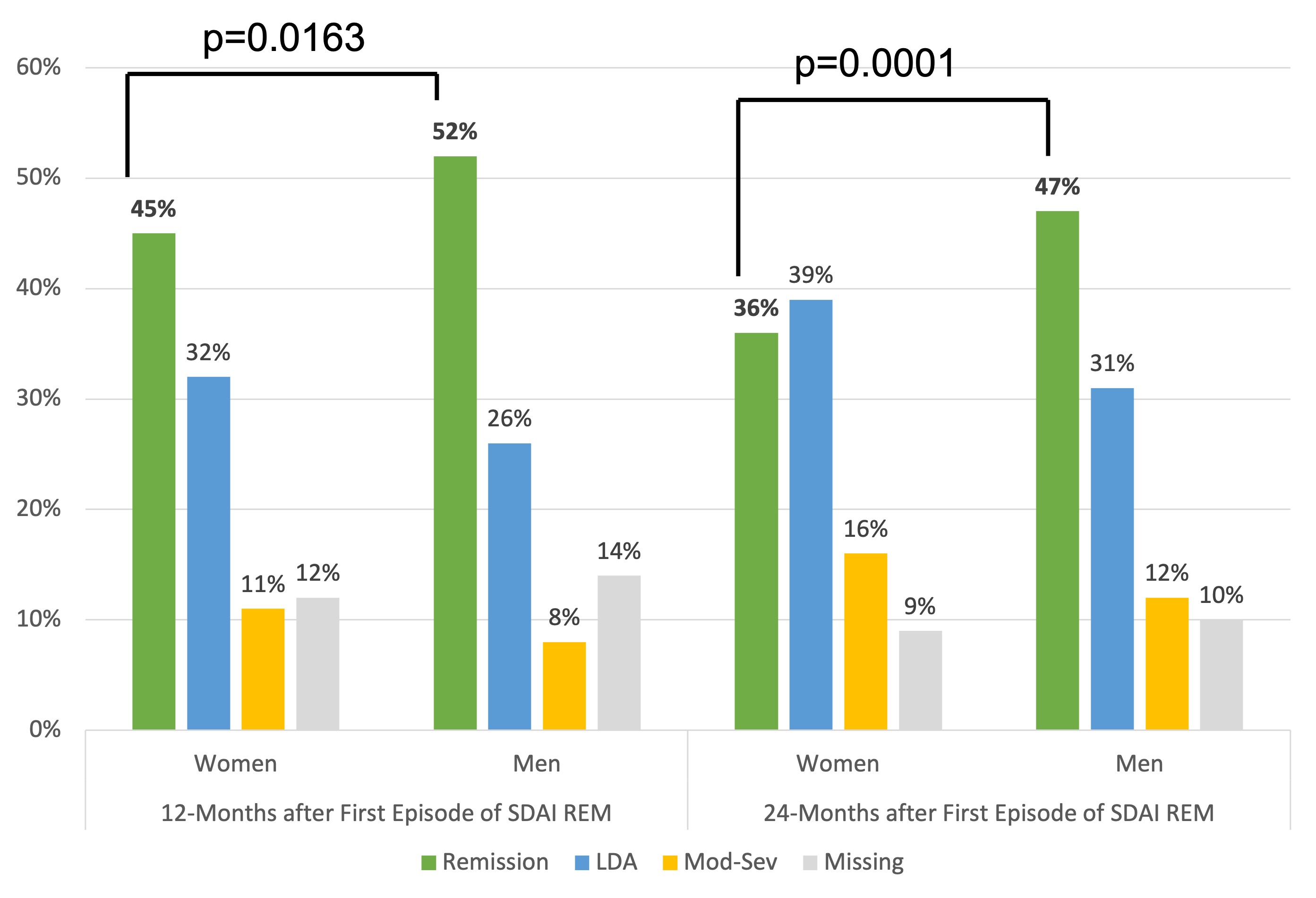 Figure. SDAI Disease Activity Status in Women and Men with Early Rheumatoid Arthritis 12- and 24 Months after First Reaching Remission
Figure. SDAI Disease Activity Status in Women and Men with Early Rheumatoid Arthritis 12- and 24 Months after First Reaching Remission
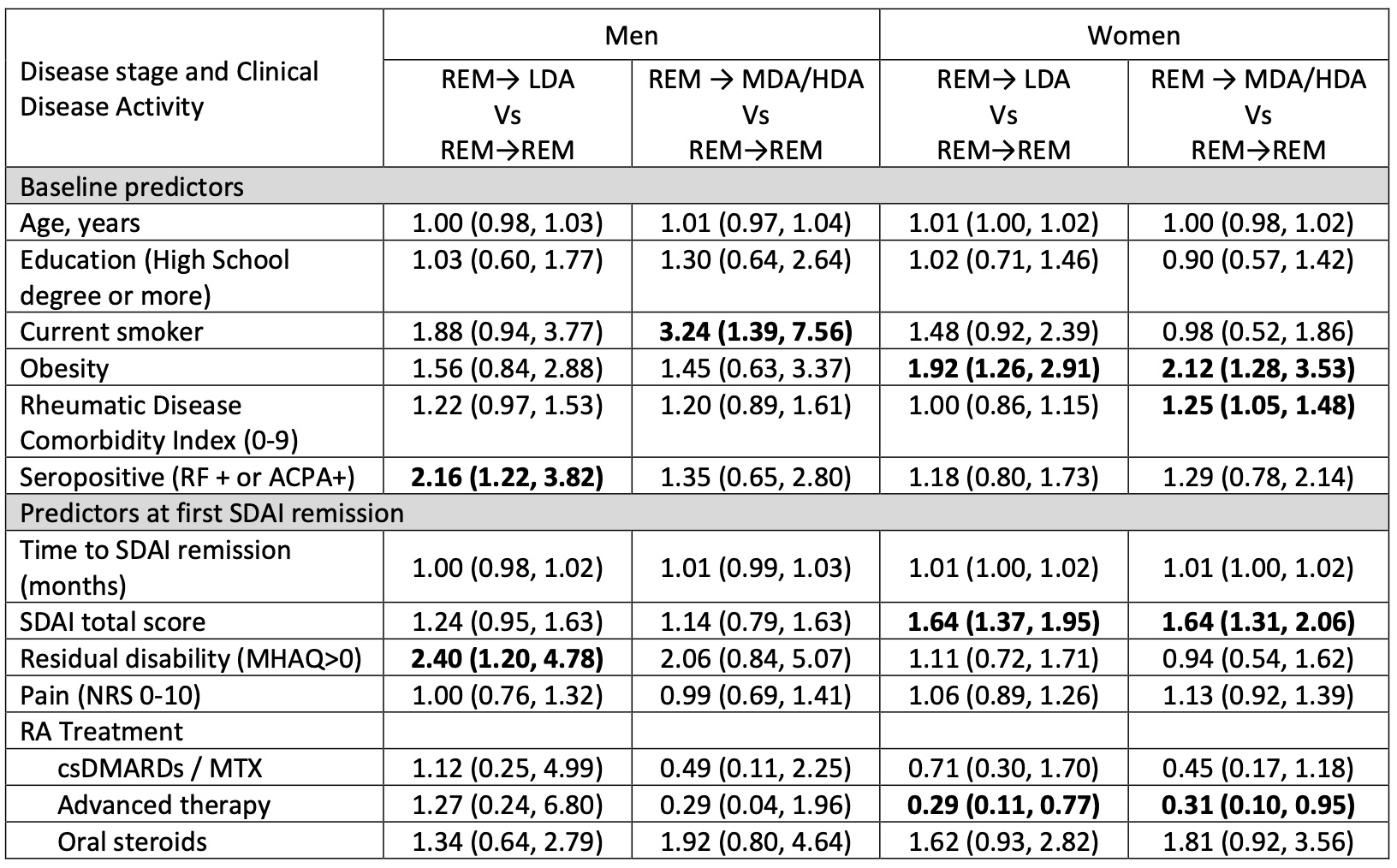 Table. Adjusted Multinomial Regression Results of Predictors of Minor and Major Flares over 24-Month Follow Up After First SDAI Remission
Table. Adjusted Multinomial Regression Results of Predictors of Minor and Major Flares over 24-Month Follow Up After First SDAI Remission
Disclosures: o. schieir, None; S. Bartlett, Pfizer, Novartis, Merck/MSD, Janssen, AbbVie/Abbott, Organon; M. Valois, None; G. Hazlewood, None; L. Bessette, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Celgene, Eli Lilly, Janssen, Novartis, Pfizer, Sanofi-Genzyme, UCB, Gilead, Merck/MSD, Organon, Roche; G. Boire, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Janssen, Eli Lilly, Merck/MSD, Novartis, Orimed Pharma, Pfizer, Samsung Bioepis, Teva, Viatris, Amgen, Celgene; C. Hitchon, Pfizer, UCB, AstraZeneca; E. Keystone, AbbVie/Abbott, Amgen, Gilead, Eli Lilly, Merck/MSD, Pfizer, Sanofi, Bristol-Myers Squibb(BMS), Celltrion, Myriad Autoimmune, F. Hoffmann-La Roche Inc, Genentech, Janssen, Sandoz, Samsung Bioepsis, AstraZeneca, Samsung Bioepsis; J. Pope, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Eli Lilly, merk, Roche, Seattle Genetics, UCB, Actelion, Amgen, Bayer, Eicos Sciences, Emerald, Gilead, Janssen, Novartis, Pfizer, Sandoz, Sanofi, Boehringer Ingelheim; d. tin, None; C. Thorne, AbbVie/Abbott, Amgen, Celgene, CaREBiodam, Centocor, Janssen, Eli Lilly, Novartis, Pfizer, Sanofi, Medexus/Medac, Merck; V. Bykerk, Amgen, Bristol-Myers Squibb(BMS), Genzyme, Brainstorm, Gilead, Regeneron, UCB, Pfizer, Sanofi, Aventis; C. (CATCH) Investigators, None.
Background/Purpose: Historical and established RA cohorts have reported sex disparities in remission outcomes favoring male patients. The objective of the present study was to compare early, and sustained remission in men and women with early rheumatoid arthritis (ERA) receiving guideline-based care in rheumatology clinics across Canada.
Methods: Data were from participants enrolled in the Canadian Early Arthritis Cohort (CATCH) study between 2007 and 2019. CATCH is a multi-center inception cohort of ERA patients (symptoms < 1 year, 83 % meeting RA criteria at enrolment) diagnosed and treated in rheumatology centers across Canada. Participants completed standardized study visits including detailed RA clinical assessments, patient-reported outcomes, and laboratory investigations every 3 months in the first year, every 6-months in the second year and annually thereafter mirroring real-world care practices in Canada. Treatment decisions were at the discretion of the treating rheumatologist in line with treat-to-target guidelines. Descriptive statistics were used to summarize and compare prevalence of SDAI remission (< 3.3.), median time to SDAI remission and sustained SDAI remission 12- and 24- months after first remission across men and women. Multivariable multinomial regression was used to identify predictors of minor flares (SDAI REM→LDA) and major flares (SDAI REM→MDA/HDA) over 24-months follow-up from first remission.
Results: The sample included 2,743 ERA patients (1933 women; 789 men). At enrolment, mean(sd) SDAI was high at 27.4 (14.6); most patients were treated with csDMARDs (92%), often with MTX, as monotherapy or in combination with csDMARDs (77%) and 29% were prescribed oral steroids. There were no notable differences in disease activity or treatment strategies observed between men and women at enrolment. Overall prevalence of SDAI remission over the study follow-up was similar across men (64%) and women (61%), however median time-to-remission was longer for women vs. men (19.2 months vs 16.1 months, p =0.0358), and a lower proportion of women vs. men reached early remission targets by 12-months (37% vs 43%, p=0.0054). Sustained remission 12- and 24- months after first remission was also higher in men vs. women (Figure). Predictors of minor and major flares after remission differed by sex (Table). Smoking, seropositivity and residual disability at first SDAI remission predicted flares in men, while obesity, comorbidities and higher SDAI at first remission predicted flares in women. Treatment with advanced therapy at first remission was associated with lower likelihood of flares after remission in women.
Conclusion: Results of this large longitudinal study of ERA patients receiving contemporary guideline-based care showed high overall rates of SDAI remission for men and women over the study period, however there were notable sex differences favoring men in the rapidity and sustainability of remission. Predictors of minor and major flares after remission also differed between men and women and highlighted potential modifiable risk factors for sustaining remission over longer periods including smoking and residual disability at remission in men, and obesity and chronic comorbidity management in women.
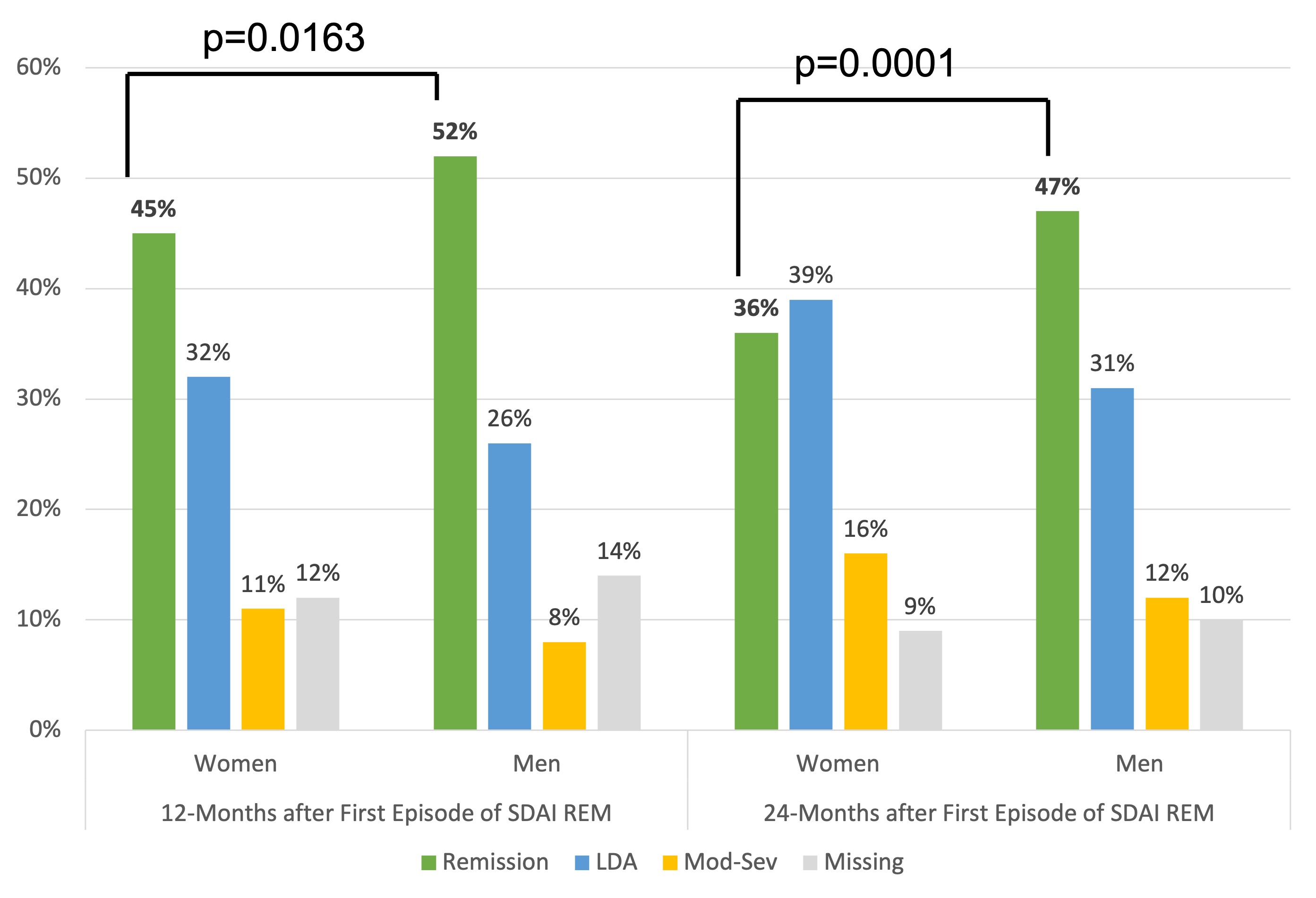 Figure. SDAI Disease Activity Status in Women and Men with Early Rheumatoid Arthritis 12- and 24 Months after First Reaching Remission
Figure. SDAI Disease Activity Status in Women and Men with Early Rheumatoid Arthritis 12- and 24 Months after First Reaching Remission 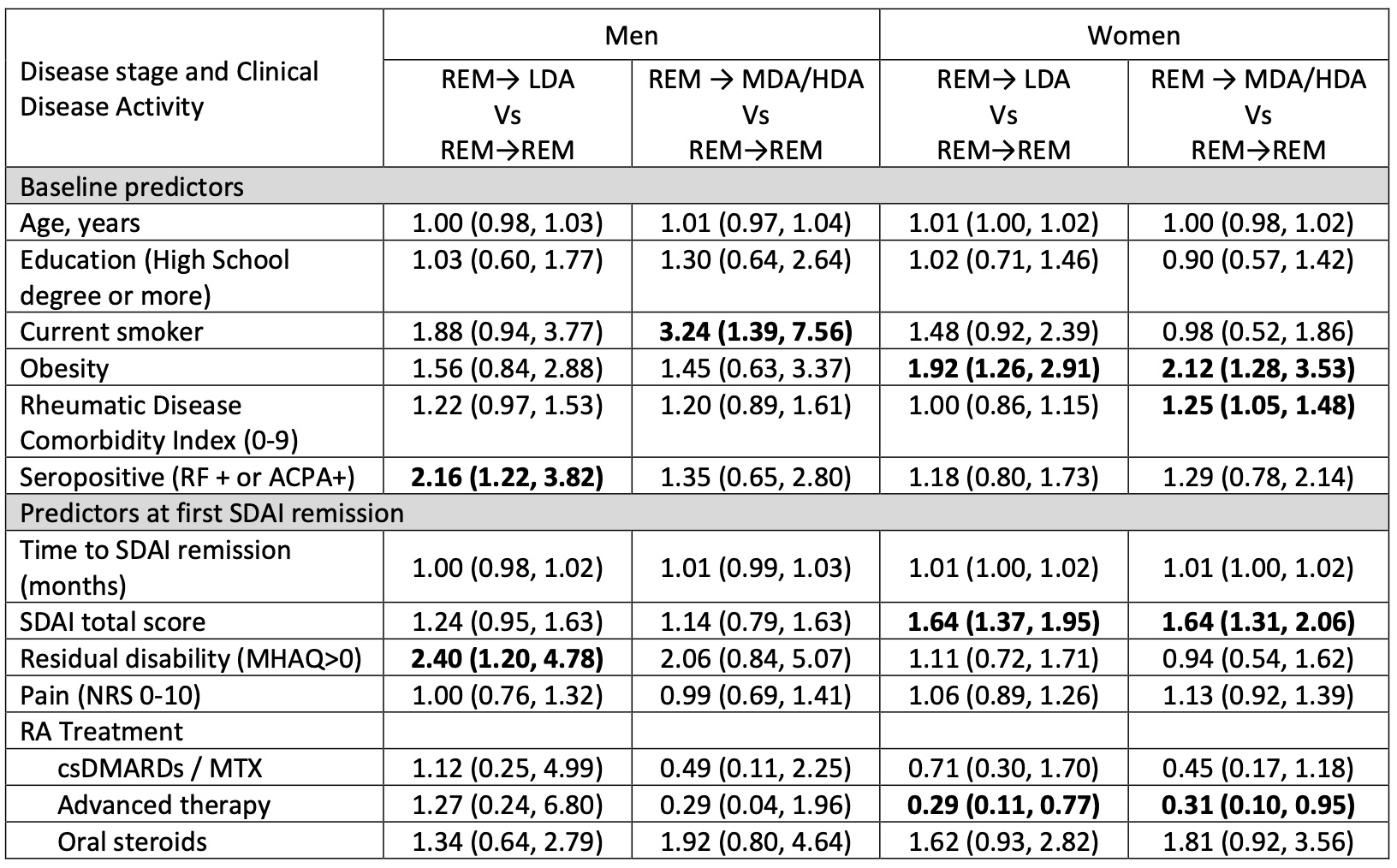 Table. Adjusted Multinomial Regression Results of Predictors of Minor and Major Flares over 24-Month Follow Up After First SDAI Remission
Table. Adjusted Multinomial Regression Results of Predictors of Minor and Major Flares over 24-Month Follow Up After First SDAI RemissionDisclosures: o. schieir, None; S. Bartlett, Pfizer, Novartis, Merck/MSD, Janssen, AbbVie/Abbott, Organon; M. Valois, None; G. Hazlewood, None; L. Bessette, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Celgene, Eli Lilly, Janssen, Novartis, Pfizer, Sanofi-Genzyme, UCB, Gilead, Merck/MSD, Organon, Roche; G. Boire, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Janssen, Eli Lilly, Merck/MSD, Novartis, Orimed Pharma, Pfizer, Samsung Bioepis, Teva, Viatris, Amgen, Celgene; C. Hitchon, Pfizer, UCB, AstraZeneca; E. Keystone, AbbVie/Abbott, Amgen, Gilead, Eli Lilly, Merck/MSD, Pfizer, Sanofi, Bristol-Myers Squibb(BMS), Celltrion, Myriad Autoimmune, F. Hoffmann-La Roche Inc, Genentech, Janssen, Sandoz, Samsung Bioepsis, AstraZeneca, Samsung Bioepsis; J. Pope, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Eli Lilly, merk, Roche, Seattle Genetics, UCB, Actelion, Amgen, Bayer, Eicos Sciences, Emerald, Gilead, Janssen, Novartis, Pfizer, Sandoz, Sanofi, Boehringer Ingelheim; d. tin, None; C. Thorne, AbbVie/Abbott, Amgen, Celgene, CaREBiodam, Centocor, Janssen, Eli Lilly, Novartis, Pfizer, Sanofi, Medexus/Medac, Merck; V. Bykerk, Amgen, Bristol-Myers Squibb(BMS), Genzyme, Brainstorm, Gilead, Regeneron, UCB, Pfizer, Sanofi, Aventis; C. (CATCH) Investigators, None.

